Public health funding cuts are becoming a significant concern as state health departments face challenges in maintaining operations amidst diminishing resources. These cuts, often cyclical in nature, see funding dry up after a crisis like the COVID-19 pandemic, which can severely impact the effectiveness of health programs. With federal funding primarily sourced from key agencies such as the CDC, the implications of these funding changes could include fewer staff and reduced capacity to address public health threats. Public health is a cornerstone of community well-being, and the ongoing funding cuts could threaten our ability to respond to future outbreaks and health emergencies effectively. As communities grapple with the repercussions of these budget reductions, understanding the broader impact of public health funding on local health initiatives becomes paramount.
The landscape of public health is under siege as authorities grapple with severe budgetary reductions and the subsequent challenges of sustaining health programs. The recent reductions in financial support, particularly from state and federal levels, are creating vast uncertainties for health departments across the nation. As the importance of a robust public health infrastructure cannot be overstated, cuts to agencies like the CDC jeopardize the essential services provided to communities. Furthermore, the termination of COVID-related funding has raised alarms among health officials who are concerned about their ability to respond to emerging health crises. In this context, it is critical to discuss the implications of these funding alterations on public health preparedness and the disparities they create in ensuring communal health safety.
The Consequences of Public Health Funding Cuts
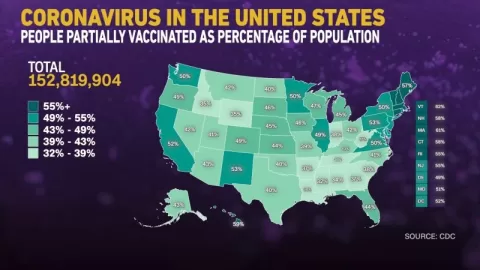
Public health funding cuts have a domino effect, drastically limiting the resources available for state and local health departments. As funding diminishes, programs that were previously established to monitor and combat infectious diseases face elimination or significant scaling back. For instance, when a substantial portion of COVID-19 funding was revoked, states like Alabama and Minnesota reported losses in the hundreds of millions, affecting essential vaccination initiatives and emergency preparedness activities. These cuts not only threaten public health programs but also compromise the ability of health departments to effectively respond to outbreaks.
Moreover, the abrupt cessation of funds often leads to layoffs and staff reductions within health departments, further exacerbating the issue. With fewer personnel, the remaining staff members struggle to fulfill their duties effectively, creating a bottleneck in public health response efforts. In Minnesota, the health department had to issue layoff notices to over a hundred employees, signifying a serious reduction in workforce dedicated to monitoring public health. This dire situation underscores the crucial necessity for stable public health funding and the profound impact short-term budget decisions can have on long-term health outcomes.
Impact of CDC Funding Changes on Local Health Departments
The Centers for Disease Control and Prevention (CDC) plays a pivotal role in providing resources and expertise to state and local health departments. However, recent CDC funding changes have raised alarms about the sustainability of public health infrastructures across the nation. According to reports, significant CDC grants, which account for the majority of budgets for local health departments, have not been disbursed on time, resulting in halted programs and delayed public health initiatives. This unpredictability complicates the already precarious financial landscape that health departments must navigate, especially during periods when timely responses to health crises are critical.
As CDC funding continues to dwindle, local health officials express their fears that vital public health functions may become nonviable. The American Public Health Association highlights that these funding cuts might mean entire health programs would be unable to fulfill their intended purposes. State health officials emphasize the reliance on CDC grants for tackling pressing public health issues, such as immunization programs and health equity initiatives. The changes in CDC funding thus pose a direct threat not only to existing health programs but also to the overall public health landscape.
The Importance of Public Health Funding Stability
The importance of stable public health funding cannot be overstated. During crises like the COVID-19 pandemic, funding tends to surge in response to immediate threats; however, this short-term approach neglects the underlying need for consistent support. Public health expert Brian Castrucci emphasizes that sustainable funding is crucial for maintaining a protective public health framework capable of addressing both current and future health challenges. Without this stability, health departments are left vulnerable to budgetary cuts, severely affecting their operational capacity and efficacy.
Moreover, a stable funding environment fosters the development of long-term public health strategies that can proactively address community health issues. This includes staffing skilled professionals, investing in data infrastructure, and enhancing community outreach programs. As echoed by public health leaders, consistent funding allows departments to plan and execute initiatives instead of scrambling for resources only during emergencies. It highlights the need for a fundamental shift in how public health is funded, transitioning from reactive to proactive budgeting that prioritizes public health integrity long-term.
Long-Term Impacts of State Health Departments Budget Cuts
The long-term impacts of budget cuts to state health departments are profound, often resulting in weakened public health systems that struggle to respond to crises effectively. As health departments are forced to downsize, the loss of institutional knowledge and personnel expertise creates gaps that can take years to fill. This degradation in capabilities means that public health departments may find it increasingly challenging to manage routine health issues and respond to the next public health crisis, thereby endangering community health and safety.
Furthermore, the implications of such budget cuts extend beyond immediate operational challenges. Health departments serve as the frontline for managing preventable diseases and health disruptions. With fewer resources, initiatives aimed at disease prevention, health education, and community outreach become significantly hampered. As public health systems spiral downwards, states may find themselves in a precarious situation where they are ill-equipped to handle outbreaks, which could potentially lead to larger public health crises in the future.
Public Health Infrastructure: A National Concern
Public health infrastructure is a critical component of the nation’s health strategy, yet it often receives less attention compared to other sectors such as education and law enforcement. The recent wave of budget cuts serves as a reminder of the fragile state of public health systems, which rely heavily on federal support. As funding fluctuates, public health leaders urge that it’s not only a matter of state and local jurisdictions but a national concern that affects everyone. The consequences of inadequately funded public health systems are far-reaching, impacting everything from food safety to vaccination rates.
Moreover, the lack of robust public health infrastructure has broader societal implications, particularly in times of crisis. When the health system is overwhelmed due to resource constraints, the population suffers—leading to increased morbidity and mortality rates. This unavoidable reality emphasizes that improving public health infrastructure should be a priority for policymakers at all levels. By advocating for and investing in stable funding, there is a potential to enhance the nation’s resilience against future public health threats.
Building Public Awareness of Health Funding Needs
Increased public awareness about the importance of funding public health is essential for securing the necessary resources and support. Despite the clear implications of funding cuts, many citizens remain unaware of how these decisions directly affect their health and safety. Public health advocates suggest that health leaders need to better communicate the value of stable funding through community engagement and education initiatives. By making the connection between funding and health outcomes more explicit, there is a stronger chance to garner public support for ongoing funding efforts.
Moreover, grassroots campaigns and partnerships with local organizations can play a significant role in raising awareness. Engaging with community leaders and influencers can amplify the message that public health funding is a community asset, not just a government obligation. By fostering a collaborative environment that highlights the real-life impacts of public health initiatives, advocates can ensure that public health remains a priority in the eyes of funders and decision-makers alike. Ultimately, informed citizens can advocate more effectively for the resources their health departments need.
The Role of Federal Support in Local Public Health
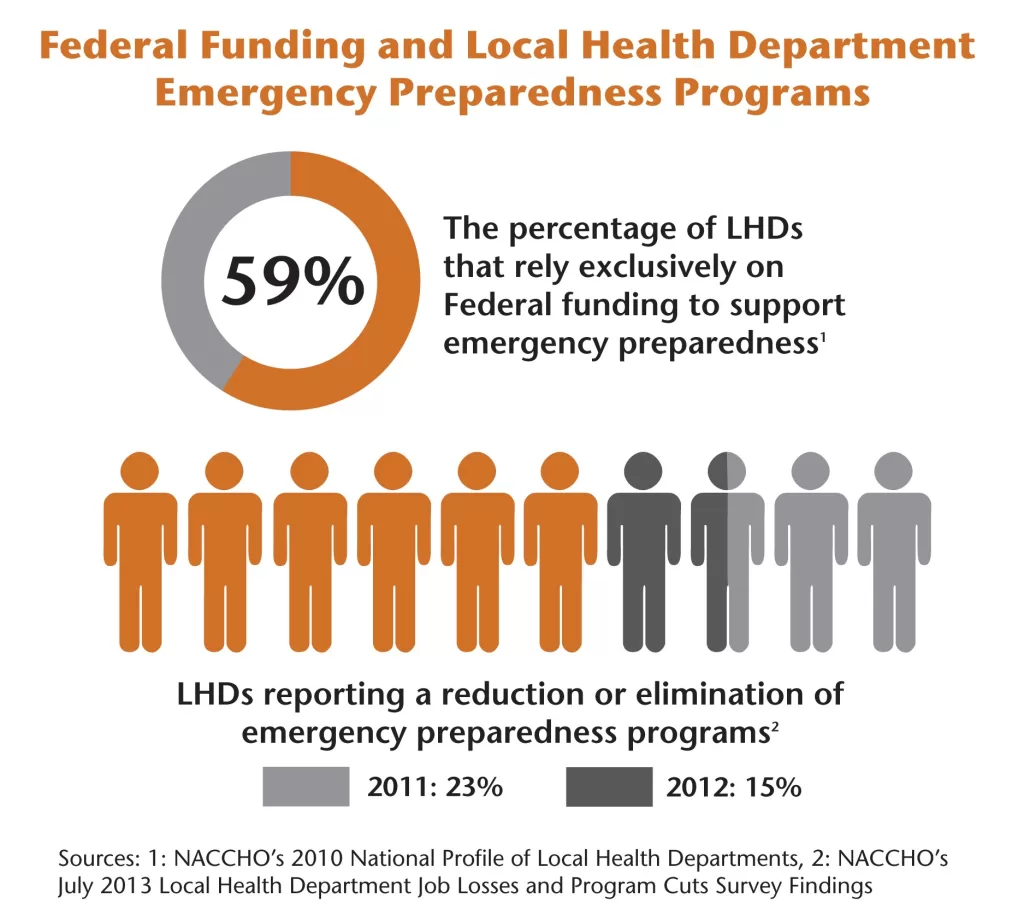
Federal support is a cornerstone for local public health operations, as the majority of funding flows from federal agencies like the CDC to state and local health departments. The current trend of budget cuts and uncertainty poses a serious risk to the continuity of public health services. Experts such as Scott Harris emphasize that the collaboration between federal and local health agencies is essential for addressing public health emergencies effectively. Without a fortified partnership, the ability of local health officials to handle crises is significantly compromised.
The ramifications of reduced federal support manifest in various ways, including stalled programs that rely heavily on federal resources. As federal funding fluctuates, local health departments are left scrambling to adjust their budgets, often at the expense of essential services. This instability can stifle innovation and hinder the development of vital public health initiatives, making it more challenging for jurisdictions to respond to emerging health threats. Therefore, maintaining federal support is crucial for enabling state and local health departments to carry out their mission effectively.
A Call for Reimagining Public Health Funding
As the public health landscape continues to evolve, there is an urgent call to reassess and reimagine how public health funding is structured. Several experts argue that the heavy reliance on short-term funding cycles leads to inefficiencies and vulnerabilities in the public health system. Castrucci advocates for a systemic overhaul that prioritizes consistent funding models designed to withstand the inevitable cycles of public health funding. By establishing a more reliable funding framework, public health agencies can operate with greater stability and predictability.
Additionally, public health officials suggest that collaboration between various sectors—such as health, education, and community services—can create a united front for advocating for increased and sustained funding. A coherent approach to public health financing that encompasses a multitude of stakeholders may play a pivotal role in shaping a future where public health systems are robust and adequately supported. This proactive stance can potentially transform the public health infrastructure into a strong foundation that ensures the well-being of communities nationwide.
Looking Toward the Future of Public Health Funding
The future of public health funding remains uncertain, with looming budget cuts raising concerns among health officials. As the pandemic exposed existing weaknesses in the public health infrastructure, there is a pressing need to build back stronger systems that can withstand future health crises. Public health leaders emphasize that this vision requires not only increased funding but also a commitment to long-term planning that encompasses workforce development, data systems, and outreach initiatives.
Moreover, as public awareness about the importance of health departments grows, there may be newfound political will to allocate necessary resources. Engaging with communities to raise awareness about the impacts of health funding on everyday life is crucial. By fostering a greater understanding of public health’s role in ensuring community well-being, advocates hope to spur policy changes that lead to a more resilient public health system in the future.
Frequently Asked Questions
What are the impacts of public health funding cuts on state health departments?
Public health funding cuts critically reduce the budgets of state health departments, directly affecting staff expertise, operational capacities, and the ability to respond to health crises. Reports indicate that federal funding accounts for a significant portion of state health budgets, meaning cuts can lead to layoffs, program disruptions, and hindered emergency responses to outbreaks.
How have CDC funding changes affected local health departments during the COVID-19 pandemic?
CDC funding changes, particularly cuts initiated during and post-COVID-19, have drastically impacted local health departments. These reductions have resulted in the loss of vital resources for programs dealing with infectious diseases, health equity initiatives, and overall public health infrastructure, severely limiting their operational capabilities and emergency preparedness.
What is the importance of public health in the face of funding cuts?
The importance of public health becomes starkly evident during funding cuts, as these reductions jeopardize the foundational support for disease monitoring and prevention efforts. A well-funded public health system ensures community health, emergency preparedness, and the capacity to address both chronic and infectious diseases, which is vital in maintaining public safety.
What are the potential effects of COVID-19 funding cuts on future public health responses?
COVID-19 funding cuts threaten future public health responses by diminishing the resources available for critical programs, leading to layoffs and reduced capabilities within health departments. This lack of funding can result in slower responses to outbreaks and compromised public health initiatives, increasing vulnerability to future health crises.
How do public health funding cuts impact job security for public health professionals?
Public health funding cuts significantly affect job security for health professionals, as budget reductions often lead to layoffs and decreased hiring. The current atmosphere of uncertainty can discourage prospective students from pursuing careers in public health and compel current professionals to seek employment in more stable fields.
What strategies can be employed to advocate for public health funding at the community level?
To advocate for public health funding, public health leaders should engage with community stakeholders, such as school officials and business leaders, to communicate the value of robust health systems. Establishing collaborative networks can amplify their message and foster community support for sustained public health investments.
What role does federal expertise play in state health departments, especially during funding cuts?
Federal expertise is crucial for state health departments, particularly during funding cuts that limit local capabilities. Federal agencies provide specialized knowledge and support essential for managing public health emergencies and outbreaks. Reductions in federal staffing can hinder these collaborative efforts, exacerbating public health challenges.
How can the public health funding cycle in the U.S. be reimagined for greater stability?
Reimagining the public health funding cycle requires moving away from boom-and-bust patterns by fostering consistent, reliable funding mechanisms. This transformation involves enhanced advocacy, communication with communities about public health benefits, and strategic policy changes to ensure a stable investment in public health infrastructure.
What are the long-term consequences of public health funding cuts on community health?
Long-term consequences of public health funding cuts on community health include increased disease outbreaks, diminished public health services, lower vaccination rates, and greater health disparities. These effects can lead to a cycle of increased healthcare costs and poorer health outcomes for vulnerable populations.
How do public perceptions of public health change during times of funding cuts?
Public perceptions of public health can shift dramatically during funding cuts, often only recognizing their importance during a crisis. This lack of awareness may lead to diminished support for public health initiatives until problems arise, highlighting the need for sustained community education on public health’s critical role.
| Key Issues | Impacts of Funding Cuts | Experts’ Opinions |
|---|---|---|
| Historical Boom-and-Bust Cycles in Funding | Loss of federal funding leads to layoffs and halted programs. | Experts warn of diminished capacity to respond to public health emergencies. |
| Recent cuts under the Trump Administration | State health departments are losing vital CDC grants necessary for disease monitoring. | Rising concerns over public health infrastructure sustainability raised by officials. |
| Federal Expertise Loss | Colleges may see reduced interest in public health careers due to instability. | Calls for restructuring funding models to ensure future stability. |
Summary
Public health funding cuts pose a significant threat to the nation’s ability to respond effectively to health emergencies. As federal funding diminishes, state and local health departments face unprecedented challenges including workforce reductions and program suspensions. Experts warn that these cuts not only jeopardize existing public health initiatives but also impair the infrastructure needed for crisis response. Without immediate and sustained investment in public health, the ramifications of these funding cuts could lead to dire consequences for public health preparedness and community well-being.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.