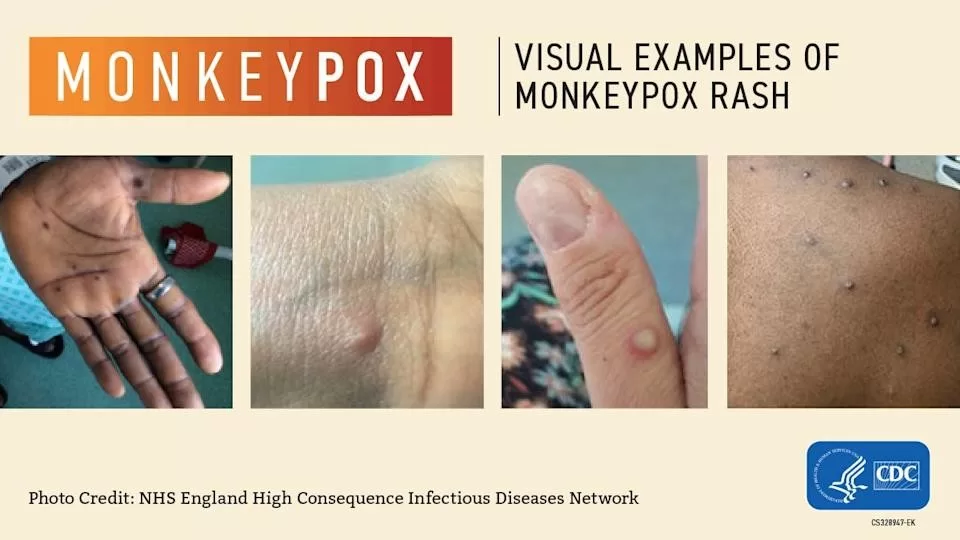
Prolonged monkeypox infections have emerged as a concerning aspect of the ongoing mpox outbreak, particularly in California from May 2022 through August 2024. While the standard duration for monkeypox virus (MPXV) infections typically spans 14 to 28 days, cases exceeding this timeframe have been identified, warranting further investigation. Preliminary data reveals intriguing demographic trends, with individuals suffering from prolonged MPXV infections often being more likely to be Black or African American and having concurrent HIV conditions. Furthermore, these prolonged cases highlight the critical role of the JYNNEOS vaccine, as no prolonged infections have been recorded among those who received two doses. Understanding the monkeypox duration and its implications for public health is essential, especially as we explore the nexus between HIV and monkeypox within affected populations.
The ongoing challenge posed by mpox, the disease synonymous with the monkeypox virus, underscores the importance of addressing prolonged infections. Known for its characteristic symptoms, this viral infection generally resolves within a few weeks; however, some individuals experience symptoms that extend far beyond the typical timeframe, indicating a more complex path of infection. With the intersection of factors such as HIV status and vaccination efforts—specifically the JYNNEOS vaccine—prolonged MPXV cases demand focused attention. There is a pressing need to analyze the patterns and demographic disparities associated with these extended infections, notably in regions like California. By unveiling insights associated with prolonged cases, health agencies can better support high-risk groups and enhance preventive measures.
Understanding Prolonged Monkeypox Infections
Prolonged monkeypox infections, characterized by symptoms lasting beyond the typical 14-28 day period, have been a point of concern especially given their low incidence among total cases. According to data from California, only 1.3% of cases fell into this category; however, the health implications for affected individuals are substantial. Most notably, certain demographics, particularly those with HIV, presented higher risks, necessitating more focused research and awareness to mitigate potential outbreaks. Recognizing the significance of prolonged infections is vital for both individual health management and broader public health strategy.
In instances of prolonged MPXV infections, the interplay with factors such as race and HIV status has revealed troubling trends. For example, data indicates that over 61% of those experiencing prolonged symptoms were also living with HIV. These individuals often had lower CD4 counts, highlighting an intersection of vulnerabilities that could be exacerbated by delayed treatment or care engagement. Understanding these patterns not only aids in improving treatment and health outcomes for those affected but also enhances preventive strategies to avoid such prolonged cases in the future.
Impact of HIV on Monkeypox Duration
The relationship between HIV status and prolonged monkeypox infections signifies a critical area of focus for health professionals. Individuals living with HIV are known to have compromised immune systems, which could lead to an increased duration of viral infections such as monkeypox. The California mpox registry data reveals that those with lower CD4 counts exhibited significantly higher rates of prolonged MPXV infections, underscoring the need for tailored interventions for this at-risk population. By integrating HIV care with targeted monkeypox preventive measures, healthcare providers can better manage these dual health challenges.
Moreover, the disparity in monkeypox duration across various HIV status emphasizes the need for combined health strategies. Patients who are not engaged in HIV care face an alarming increased risk of enduring monkeypox symptoms for an extended period. Introducing timely health education initiatives about the importance of continuous care and vaccination could substantially mitigate this risk. Addressing these healthcare gaps is essential to improve health outcomes for individuals who may experience prolonged monkeypox infections.
The Role of the JYNNEOS Vaccine in Monkeypox Management
The JYNNEOS vaccine has played a pivotal role in the management and prevention of monkeypox, particularly for vulnerable populations. The results from California demonstrate that none of the individuals who received a complete two-dose regimen of the JYNNEOS vaccine experienced prolonged monkeypox symptoms. This finding underscores the vaccine’s efficacy in not only preventing infection but potentially reducing the severity and duration of the disease in vaccinated individuals.
As public health efforts advance, increasing awareness and accessibility of the JYNNEOS vaccine for high-risk groups remains a priority. Health departments must focus their outreach on educating populations disproportionately affected, including communities with higher rates of prolonged infections. Enhancing vaccination uptake can significantly contribute to curtailing the spread of monkeypox and alleviating the health burden on individuals, particularly for those living with HIV and other underlying health conditions.
Epidemiological Trends of Mpox in California
The epidemiological trends surrounding mpox cases in California from May 2022 to August 2024 reveal critical insights into the demographics impacted by this viral outbreak. Data analysis indicates that Black or African American individuals were disproportionately affected, and there exists a notable correlation with prolonged monkeypox infections among those with HIV. Understanding these trends is crucial for effectively targeting public health interventions and addressing the unique needs of affected communities.
Furthermore, by leveraging the data obtained from the California mpox registry, health authorities can implement more informed strategies to monitor and respond to outbreaks. With a historical baseline established, future epidemiological studies can better track the evolution of mpox, assess the efficacy of vaccination efforts, and facilitate the development of tailored public health campaigns to educate at-risk populations about prevention and care.
The Significance of Outreach Programs for Vulnerable Populations
Outreach programs targeting vulnerable populations are essential in combating the spread of monkeypox and in addressing the issue of prolonged infections. For instance, communities with higher rates of HIV and lower health literacy may lack the necessary resources or information to prevent or treat monkeypox effectively. Establishing proactive outreach initiatives that educate these populations on the risks of prolonged infections and the importance of vaccination can significantly enhance health outcomes.
Additionally, incorporating educational components regarding the interconnectedness of HIV and monkeypox into existing health services can empower individuals to take charge of their health. Public health campaigns should disseminate clear, accessible information about symptoms, treatment options, and vaccination benefits. By prioritizing outreach efforts aimed at marginalized populations, health officials can help reduce the incidence of prolonged MPXV cases and ultimately control the spread of monkeypox in community settings.
Monkeypox Case Management Strategies for Public Health Officials
Effective case management strategies are paramount in minimizing the impact of monkeypox outbreaks. Public health officials must prioritize swift identification and containment of cases, particularly in populations vulnerable to prolonged infections. By employing robust surveillance measures and leveraging data from registries like California’s, officials can quickly assess and respond to rising case numbers, tailoring resources to where they are needed most.
Moreover, integrating data on individuals with HIV into case management strategies provides a clearer picture of the risks associated with prolonged monkeypox infections. Public health response teams must ensure that affected individuals receive follow-up care and are aware of available vaccinations, such as JYNNEOS, that can help prevent future infections. This multifaceted approach is essential for effective long-term management of monkeypox and promoting overall community health.
Long-term Effects of Monkeypox Infections
Long-term effects of monkeypox, particularly for individuals with prolonged infections, remain an essential area of research. While most cases resolve within a month, those who experience extended symptoms may face residual health issues that could impact their quality of life. Studies should focus on comprehensive assessments of the long-term health implications of MPXV infections, especially among populations with coexisting conditions such as HIV.
Understanding the long-term consequences of monkeypox infections will help in developing better support systems and healthcare resources for affected individuals. It is vital for healthcare providers to monitor patients with prolonged cases for ongoing health complications, thereby fostering a holistic approach to care that addresses both immediate and chronic health needs. This focus will ensure that those impacted by the virus receive adequate support and management moving forward.
Monkeypox Vaccination Trends Among High-Risk Groups
Vaccination trends among high-risk groups are crucial in understanding how to effectively manage monkeypox outbreaks. The JYNNEOS vaccine has shown efficacy in reducing the severity and duration of infections, especially among individuals with high-risk profiles. Tracking the uptake of vaccination within communities disproportionately affected by prolonged MPXV infections is essential for public health planning.
Data collection and analysis should focus on barriers to vaccination, such as accessibility and misinformation, which may disproportionately affect marginalized populations. Ensuring that these high-risk groups are educated about the benefits of the JYNNEOS vaccine, along with overcoming obstacles to access, are integral for improving vaccination rates and decreasing cases of prolonged infections in the community.
Future Directions in Monkeypox Research and Policy
As monkeypox continues to pose health challenges, future research must focus on understanding the nuances of prolonged infections and how they relate to various demographic factors, including HIV status. It’s critical to establish long-term studies that can guide effective policies aimed at high-risk populations. By aligning ongoing research with health policy efforts, public health officials can ensure that interventions are based on solid evidence, potentially leading to better health outcomes.
Moreover, collaboration between researchers, healthcare providers, and community organizations will be vital for implementing strategies that address the multifactorial nature of monkeypox. This will enable a comprehensive approach that not only targets the virus but also considers the wider social determinants of health that affect vulnerable groups, ultimately leading to reduced transmission and improved public health trajectories.
Frequently Asked Questions
What are the signs of prolonged monkeypox infections?
Prolonged monkeypox infections typically exceed the standard duration of 14 to 28 days, with symptoms persisting beyond 28 days. Common signs include persistent rashes, fever, and swollen lymph nodes that continue beyond the usual recovery period.
How does HIV influence prolonged monkeypox infections?
HIV significantly increases the risk of prolonged monkeypox infections. In a study, 61% of individuals with prolonged MPXV infections were living with HIV, especially those with lower CD4 counts or who were not engaged in HIV care.
What is the role of the JYNNEOS vaccine in preventing prolonged MPXV infections?
The JYNNEOS vaccine plays a critical role in preventing prolonged MPXV infections, as no prolonged cases were reported among individuals who received both doses of the vaccine. Vaccination is crucial for high-risk groups.
What demographic factors are associated with prolonged monkeypox infections?
Demographic factors associated with prolonged monkeypox infections include being Black or African American and having a diagnosis of HIV. These groups have shown higher susceptibility to infections that last longer than 28 days.
How common are prolonged MPXV infections based on California data?
According to data from California, only 1.3% of recorded monkeypox infections were categorized as prolonged, indicating that while most cases resolve within the typical timeframe, certain individuals are at higher risk of prolonged symptoms.
What public health measures are needed for prolonged monkeypox infections?
Increased education and outreach are vital for populations disproportionately affected by prolonged monkeypox infections, particularly individuals living with HIV. Public health strategies should focus on promoting vaccine uptake, particularly among high-risk communities.
Can prolonged monkeypox infections be treated effectively?
While there is no specific antiviral treatment for mpox, supportive care can help manage symptoms of prolonged monkeypox infections. Monitoring and treatment of complications are essential, especially in individuals with weakened immune systems.
| Key Points | Details |
|---|---|
| Typical Duration of MPXV Infection | 14 to 28 days. |
| Prolonged Infections | Symptoms or tests positive for over 28 days, 1.3% of cases. |
| Demographic Factors | Higher prevalence in Black/African American (20.7%) and HIV-positive individuals (61%). |
| Impact of HIV Status | Lower CD4 count (<200) increased risk (10% vs. 3.9% non-prolonged). 46% of non-engaged HIV care individuals had prolonged infections. |
| JYNNEOS Vaccine Effectiveness | No prolonged infections among individuals who received 2 doses of the vaccine. |
| Public Health Recommendations | Targeted vaccine education and outreach for disproportionately affected groups. |
Summary
Prolonged monkeypox infections have become a pivotal issue in understanding the dynamics of monkeypox outbreaks, particularly following the resurgence of cases starting in May 2022. This extended duration of symptoms calls attention to the specific populations, such as Black or African American communities and individuals living with HIV, who are disproportionately affected. Additionally, effective strategies such as promoting the JYNNEOS vaccine could significantly curb the incidence of these prolonged infections. Public health initiatives must therefore focus on education and outreach in at-risk demographics to mitigate future outbreaks.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.