Postmenopausal bleeding (PMB) is a significant health concern that affects many women after they have stopped menstruating for a full year. While this unexpected bleeding can often be attributed to benign conditions, it may also signal serious issues, such as endometrial cancer. Understanding the causes of postmenopausal bleeding, recognizing PMB symptoms, and knowing when to seek medical attention are crucial for women’s health awareness. In this article, we will delve into the various aspects of PMB, including its diagnosis and potential implications for women’s health. By shedding light on this important topic, we aim to empower women to take charge of their health and seek timely care.
Also referred to as abnormal vaginal bleeding after menopause, postmenopausal bleeding raises important questions about women’s reproductive health. This condition can manifest in various ways, including spotting or heavier bleeding, and often requires careful evaluation to determine its underlying causes. While many women might assume any bleeding is a natural consequence of hormonal changes, it is vital to recognize when such symptoms could indicate more serious health concerns, including postmenopausal bleeding and cancer. Through increased awareness and understanding of the diagnosis of postmenopausal bleeding, women can better navigate their health journeys and advocate for themselves effectively.
Understanding the Symptoms of Postmenopausal Bleeding (PMB)
Postmenopausal bleeding (PMB) manifests primarily as any vaginal bleeding that occurs after a woman has reached menopause, which is defined as having no menstrual periods for twelve consecutive months. The symptoms of PMB can vary widely among women, ranging from light spotting to heavy bleeding that may resemble menstrual flow. Additionally, some women might experience dark brown or red discharge, often accompanied by other symptoms such as pelvic pain or unusual discharge. Understanding these symptoms is crucial for early detection and diagnosis.
Recognizing the symptoms of PMB is vital, as it can often be a signal of underlying health issues that require medical attention. While some women may attribute PMB to benign hormonal changes or the body adjusting post-menopause, it is essential not to ignore these signs. Women experiencing PMB should maintain an open dialogue with their healthcare providers about any changes or concerns, as prompt evaluation can lead to better health outcomes.
Common Causes of Postmenopausal Bleeding
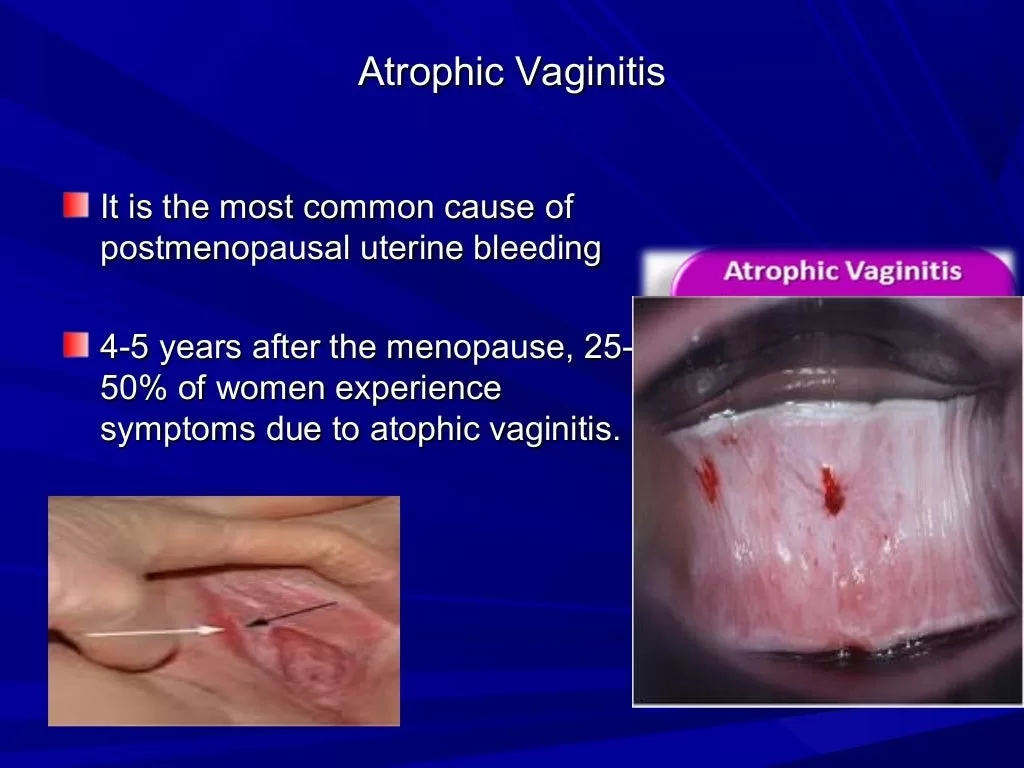
The causes of postmenopausal bleeding can be classified into both benign and serious conditions. One of the most common causes is hormonal changes, particularly fluctuations in estrogen levels leading to endometrial atrophy, where the lining of the uterus becomes thin and fragile. Other benign causes include uterine polyps and fibroids, which can also result in abnormal bleeding. Understanding these causes is essential for women to navigate their health effectively.
Apart from benign conditions, it is critical to be aware that PMB can also be an indicator of more serious health issues, including endometrial hyperplasia and endometrial cancer. Endometrial hyperplasia involves thickening of the uterine lining and, if left unchecked, can develop into cancer. Therefore, women experiencing postmenopausal bleeding should seek immediate medical evaluation to rule out any significant concerns, ensuring timely intervention if necessary.
Diagnosis of Postmenopausal Bleeding: What to Expect
If a woman experiences postmenopausal bleeding, seeking a thorough diagnosis is crucial to determine the underlying cause. The diagnostic process typically begins with a detailed medical history and pelvic examination by a healthcare provider. This initial assessment may be complemented by imaging tests such as a transvaginal ultrasound, which helps evaluate the thickness of the endometrial lining and identify any abnormalities.
In some cases, a healthcare provider may recommend an endometrial biopsy to collect tissue samples from the uterine lining. This procedure is essential for ruling out pre-cancerous or cancerous changes, particularly in women over the age of 50. By understanding the diagnostic process, women can be more proactive about their health and ensure they receive appropriate care and treatment for postmenopausal bleeding.
The Emotional Impact of Postmenopausal Bleeding
Experiencing postmenopausal bleeding can significantly impact a woman’s emotional well-being. The uncertainty surrounding the cause of the bleeding can lead to feelings of anxiety and fear, as many women may worry about the possibility of serious health issues such as cancer. This emotional distress is sometimes compounded by societal stigma surrounding women’s health issues, making it difficult for women to engage in open conversations about their symptoms.
It’s important for women to acknowledge and address the emotional aspects of PMB, as this can influence their overall health outcomes. Sharing personal experiences and seeking support from healthcare professionals or support groups can help alleviate some of the fear and anxiety associated with postmenopausal bleeding. Women’s health awareness initiatives are increasingly emphasizing the importance of emotional support alongside medical treatment.
Guidelines for Managing Postmenopausal Bleeding
When it comes to managing postmenopausal bleeding, women should prioritize their health by treating any unexpected vaginal bleeding as a significant concern that warrants prompt medical attention. Following the onset of PMB, scheduling a consultation with a healthcare provider for an assessment is essential. During this visit, women can discuss their symptoms, undergo necessary evaluations, and explore potential treatment options.
Staying informed about the risks associated with postmenopausal bleeding is also crucial for women’s health awareness. By understanding what constitutes abnormal bleeding and the potential underlying causes, women can be more vigilant and proactive in seeking care. Education plays a vital role in ensuring that women do not overlook symptoms and are empowered to advocate for their health.
Frequently Asked Questions
What are the common causes of postmenopausal bleeding (PMB)?
Postmenopausal bleeding (PMB) can be caused by several factors, including hormonal changes, endometrial atrophy, endometrial hyperplasia, uterine polyps or fibroids, and in some cases, endometrial cancer. Hormonal fluctuations can lead to thinning of the vaginal lining, while conditions like endometrial hyperplasia may pose risks for cancer if untreated.
What are the symptoms associated with postmenopausal bleeding (PMB)?
The primary symptom of postmenopausal bleeding (PMB) is any vaginal bleeding occurring after menopause. This can include spotting, light bleeding, or heavier bleeding that resembles a menstrual period. Some women may also experience pelvic pain or unusual discharge, but the key indicator is the unexpected return of bleeding.
How is the diagnosis of postmenopausal bleeding (PMB) conducted?
The diagnosis of postmenopausal bleeding (PMB) typically involves a thorough evaluation by a healthcare provider. This may include a pelvic exam, transvaginal ultrasound to assess endometrial thickness, and an endometrial biopsy to rule out pre-cancerous or cancerous changes.
Is postmenopausal bleeding (PMB) always a sign of cancer?
No, postmenopausal bleeding (PMB) is not always indicative of cancer. While it can be a symptom of endometrial cancer, PMB can also result from benign conditions such as hormonal changes or uterine polyps. However, it is crucial to seek medical evaluation to rule out serious conditions.
Why is women’s health awareness important in relation to postmenopausal bleeding (PMB)?
Women’s health awareness is vital regarding postmenopausal bleeding (PMB) because many women underestimate its significance. Increased awareness can lead to timely diagnosis and treatment, improving health outcomes. Understanding PMB symptoms helps women recognize when to seek medical advice, which is crucial for addressing potential health risks.
| Aspect | Details |
|---|---|
| Definition | Vaginal bleeding occurring after menopause, defined as 12 months without a menstrual period. |
| Symptoms | – Spotting or light bleeding – Heavier bleeding resembling a menstrual period – Dark brown or red discharge Other symptoms may include pelvic pain or unusual discharge. |
| Common Causes | 1. Hormonal Changes 2. Endometrial Atrophy 3. Endometrial Hyperplasia 4. Uterine Polyps or Fibroids 5. Endometrial Cancer |
| Importance of Medical Evaluation | Seeking medical advice is crucial as PMB may indicate serious conditions. Early diagnosis can be life-saving. |
| Guidelines for Women | – Treat any unexpected bleeding as urgent. – Consult a healthcare provider for assessment. – Stay informed about risks and treatment options. |
Summary
Postmenopausal bleeding is a significant health concern that requires immediate attention and understanding. As highlighted in this article, it is essential for women to recognize that any vaginal bleeding after menopause is abnormal and should not be overlooked. The symptoms can range from light spotting to heavier bleeding, and the causes can vary from benign hormonal changes to serious conditions like endometrial cancer. Seeking timely medical advice is crucial for diagnosis and management. By being informed and proactive, women can improve their health outcomes and ensure that any potential issues are addressed appropriately. Education and awareness about postmenopausal bleeding are vital for women’s health, emphasizing the importance of consultation with healthcare professionals upon experiencing any abnormal symptoms.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.