Pneumococcal infections represent a significant global health challenge, often exacerbated by viral illnesses such as influenza. These infections, caused by the bacteria Streptococcus pneumoniae, can lead to serious conditions like pneumonia and even meningitis, particularly in vulnerable populations like young children and the elderly. The interplay between viral and bacterial pathogens creates a concerning environment that elevates the risk of secondary bacterial infections post-influenza. Recent studies have shown that infections like COVID-19 can further complicate this relationship, increasing the chances of viral-bacterial coinfections and worsening patient outcomes. Understanding these dynamics is crucial for improving prevention strategies and treatment protocols to combat the burden of pneumococcal infections.
Respiratory infections caused by the bacterium Streptococcus pneumoniae are often interlinked with viral diseases, particularly influenza. After viral infections, individuals frequently find themselves susceptible to opportunistic secondary infections that complicate recovery—highlighting the dual threat posed by these pathogens. Pneumococcus infections can thrive in altered respiratory environments, making it imperative to study their interactions with influenza and other respiratory viruses, including COVID-19. The escalating occurrence of viral-bacterial coinfections calls for a deeper understanding of their mechanisms, especially how they relate to public health strategies for prevention. Effective management of these overlapping infections is essential to reduce morbidity and mortality associated with respiratory illnesses.
Understanding Pneumococcal Infections and Their Impact on Public Health
Pneumococcal infections, primarily caused by the bacterium Streptococcus pneumoniae, remain a critical public health concern worldwide. These infections can manifest as pneumonia, bacteremia, or meningitis, particularly affecting high-risk populations, including the elderly and young children. The intricacies of these infections are often exacerbated by pre-existing viral infections, most notably influenza. The interaction between these pathogens underscores the importance of understanding how pneumococci can survive and proliferate in a host whose defenses have been compromised by viral invasion.
The burden of pneumococcal disease often escalates during influenza outbreaks, leading to significant morbidity and mortality rates. This alarming trend highlights the necessity for public health initiatives aimed at increasing vaccination rates against both influenza and pneumococcal diseases. Vaccines play a crucial role in preventing not only viral infections but also the subsequent bacterial complications that can follow, underscoring the intersection of viral and bacterial pathogens in respiratory illnesses.
The Role of Viral-Bacterial Coinfections in Respiratory Disease
Viral-bacterial coinfections significantly complicate the clinical management of respiratory diseases. When influenza virus attacks the respiratory system, it creates an environment ripe for secondary bacterial infections, particularly with Streptococcus pneumoniae. This dual infection leads to a heightened inflammatory response and can overwhelm the host’s immune defenses, making it critical for healthcare professionals to recognize and treat these complications early.
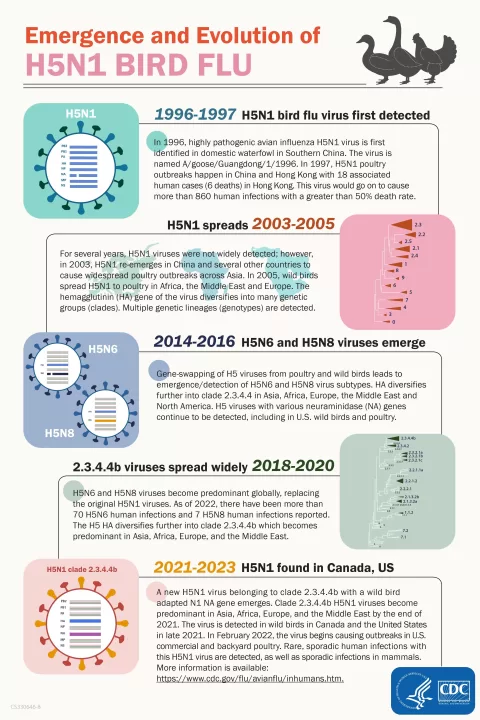
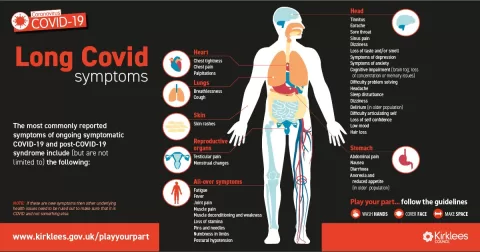
Recent studies have elucidated how coinfections with influenza and bacteria can lead to worse health outcomes than either infection alone. For example, patients suffering from COVID-19 may face similar challenges, as hospitalizations often involve the additional burden of secondary bacterial infections like pneumonia. The awareness of these complications can guide treatment strategies, emphasizing the importance of vaccinations and proactive management of respiratory infections.
Mechanisms of Infection: The Synergy Between Influenza and Pneumococcus
The pathogenic relationship between influenza and Streptococcus pneumoniae is characterized by distinct mechanisms that enhance the severity of the disease. Upon influenza infection, the immune system is activated; however, this activation can inadvertently facilitate the colonization and invasion of pneumococci. Influenza compromises the respiratory mucosal barrier, making it easier for pneumococcus to penetrate and establish an infection in the lungs and other sterile spaces.
Moreover, the altered pulmonary environment during an influenza infection promotes conditions favorable for the growth of pneumococci. Changes in epithelial cell structure and the availability of nutrients due to immune responses make the respiratory tract a hospitable niche for bacterial growth. Understanding these complex interactions is critical to developing effective therapeutic strategies to limit the impact of secondary infections.
COVID-19 and Its Relationship with Pneumococcal Infections
The COVID-19 pandemic has further emphasized the significance of understanding pneumococcal infections within the context of viral infections. Emerging evidence suggests that patients with COVID-19 are more susceptible to secondary bacterial infections, including those caused by Streptococcus pneumoniae. This heightened risk warrants the need for vigilant monitoring and management of bacterial superinfections in patients hospitalized with COVID-19.
Health authorities are increasingly recognizing the importance of vaccinating vulnerable populations against pneumococcal disease, especially in the wake of COVID-19, as these co-infections potentially lead to increased complications and mortality rates. In the context of public health, strategizing around the dual threat posed by viral-bacterial coinfections is crucial to mitigate the overall burden on healthcare systems.
Influenza Pneumonia: A Gateway to Secondary Bacterial Infections
Influenza pneumonia represents a significant risk factor for secondary bacterial infections, with Streptococcus pneumoniae being one of the most implicated pathogens. The direct damage caused by the influenza virus on lung tissue can create an opportunity for bacteria to invade, leading to more severe disease outcomes. Thus, the understanding of influenza pneumonia is vital for preventing the subsequent development of pneumococcal infections.
Preventative strategies against influenza pneumonia, including vaccination and early antiviral treatments, can potentially reduce the incidence of pneumococcal coinfections. By targeting the influenza virus itself, healthcare practitioners can also help diminish the risk of complications arising from secondary bacterial infections, leading to improved health outcomes for patients and alleviating the strain on healthcare resources.
Impact of Secondary Bacterial Infections on Healthcare Systems
The repercussions of secondary bacterial infections, particularly those caused by Streptococcus pneumoniae in the context of viral infections, pose significant challenges to healthcare systems worldwide. Increased hospitalizations, the need for intensive care treatment, and extended recovery times contribute to the overall burden on medical resources and infrastructure. Understanding these infections’ impact becomes paramount for healthcare planning and resource allocation.
In light of the COVID-19 pandemic, the healthcare community must remain vigilant about the potential rise in secondary bacterial infections. The integration of proactive strategies to prevent, diagnose, and treat these infections can mitigate healthcare costs and improve patient outcomes. Moreover, emphasizing vaccination efforts for both influenza and pneumococcal diseases can provide a downstream effect of safeguarding public health.
Preventing Secondary Infections: Therapeutic Strategies
Effective prevention and management of secondary bacterial infections require a multifaceted approach. Vaccination remains the cornerstone of preventing infections caused by Streptococcus pneumoniae. Individuals are encouraged to receive pneumococcal vaccines alongside annual influenza vaccinations to bolster their defenses against both viral and bacterial pathogens. This dual strategy is particularly critical for high-risk populations such as children, the elderly, and individuals with chronic health conditions.
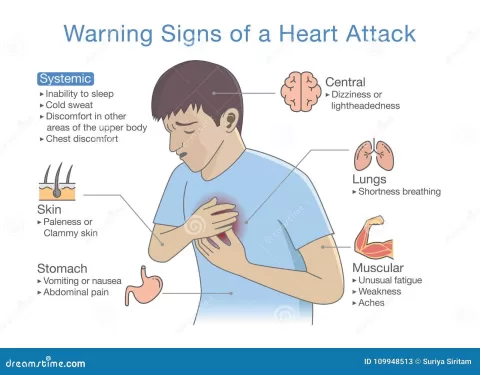
In addition to vaccinations, clinicians should prioritize prompt diagnosis and treatment of respiratory infections, implementing a combined antiviral and antibiotic strategy when necessary. Raising awareness about the signs and symptoms of pneumonia, particularly in the context of concurrent viral infections, will facilitate early intervention and reduce the risk of severe disease outcomes.
Research Innovations in Treating Viral-Bacterial Coinfections
Innovative research continues to evolve in understanding and treating viral-bacterial coinfections, particularly those involving Streptococcus pneumoniae and influenza. Studies focused on the pathophysiological mechanisms of these interactions illuminate potential therapeutic targets, paving the way for new treatment modalities. Research is also exploring the efficacy of existing vaccines and the development of novel vaccines that could provide better cross-protection against multiple pathogens.
Additionally, ongoing investigations are examining the role of host factors in susceptibility to coinfections. Personalized medicine approaches that consider individual patient immunology may yield more effective treatment strategies in combatting viral-bacterial interactions and improving patient care. These advancements signal a promising path forward in managing respiratory infections.
The Future of Vaccination: Combating Viral-Bacterial Interactions
The future of combating pneumococcal infections and related respiratory diseases hinges significantly on vaccination strategies. The integration of universal flu vaccines with pneumococcal vaccination protocols could reduce the incidence of both influenza and its associated bacterial complications. Efforts to increase vaccination coverage, particularly in vulnerable populations, will be crucial in preventing widespread outbreaks of respiratory infections.
Furthermore, research into novel vaccine candidates that offer broader protection against pneumococcal strains and other respiratory pathogens could drastically alter the landscape of preventive healthcare. As the scientific community pushes the boundaries of immunization strategies, the potential to decrease the incidence and complications of viral-bacterial interactions grows, leading to a healthier population.
Frequently Asked Questions
What are pneumococcal infections and how are they linked to secondary bacterial infections?
Pneumococcal infections are caused by the bacterium Streptococcus pneumoniae, which can lead to severe diseases such as pneumonia, meningitis, and bacteremia. These infections are often secondary to viral illnesses like influenza, where the immune response is compromised. This increased susceptibility results from changes in the respiratory tract environment, allowing pneumococcus to thrive and cause secondary bacterial infections.
How do influenza infections increase the risk of pneumococcal infections?
Influenza infections alter the immune response and respiratory tract environment, which can lead to a higher risk of pneumococcal infections. The influenza virus affects mucociliary clearance and promotes conditions favorable for bacterial growth, significantly increasing the likelihood of secondary infections with Streptococcus pneumoniae.
What role does Streptococcus pneumoniae play in viral-bacterial coinfections?
Streptococcus pneumoniae plays a critical role in viral-bacterial coinfections, particularly following viral infections like influenza. The bacterium can exploit the weakened immune response caused by the virus, leading to increased morbidity and mortality, primarily in vulnerable populations such as the elderly and those with preexisting conditions.
What is the connection between COVID-19 and pneumonia related to pneumococcal infections?
COVID-19 has been associated with an increased risk of pneumonia, including pneumococcal infections. The viral infection can compromise lung function and immune defenses, leading to secondary bacterial infections with Streptococcus pneumoniae, which complicates clinical outcomes and increases disease severity.
What strategies can help prevent pneumococcal infections secondary to influenza?
Preventive measures against pneumococcal infections, especially following influenza, include vaccination with the pneumococcal vaccine, annual flu vaccinations, and maintaining good hygiene practices. These strategies can help minimize the risk of developing secondary bacterial infections in vulnerable populations.
Are there any specific mechanisms that allow pneumococcus to thrive after influenza infections?
Yes, Streptococcus pneumoniae has developed mechanisms to adapt to the changes induced by influenza. These include alterations in the host neighborhood that increase nutrient availability and modifications to host cell receptors that facilitate bacterial adherence and invasion, enhancing the risk of secondary infections.
| Key Points | Details |
|---|---|
| Role of Streptococcus pneumoniae | Streptococcus pneumoniae (the pneumococcus) is a significant pathogen that increases the morbidity and mortality associated with influenza. |
| Impact of Viral Infections | Infections like influenza and COVID-19 predispose individuals to secondary pneumococcal infections due to altered immune responses and environmental conditions. |
| Mechanisms of Coinfection | Influenza infections disrupt the immune system and epithelial barriers, facilitating pneumococcal invasion and growth. |
| Importance of Immune Response | Ineffective innate immune responses can increase susceptibility to secondary infections during viral infections. |
| Need for Improved Strategies | There is a necessity to enhance prevention and treatment strategies for viral-bacterial co-infections, highlighting the potential benefits of vaccines and antiviral treatments. |
Summary
Pneumococcal infections are a serious concern, particularly as they can follow viral infections such as influenza and COVID-19. Understanding the interplay between these pathogens is essential in mitigating their health impacts. Enhanced research into the mechanisms of these secondary infections is crucial, paving the way for innovative therapeutic approaches and effective prevention strategies.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.