Pediatric antibiotic prescriptions have come under scrutiny as researchers uncover the significant role that common viral infections such as respiratory syncytial virus (RSV) and influenza play in outpatient settings. A recent study revealed that a staggering portion of antibiotic prescriptions for children aged 0 to 17 is associated with these acute respiratory infections (ARIs). Out of more than 21.5 million outpatient antibiotic prescriptions dispensed over a decade, nearly two-thirds were linked to ARIs, highlighting a concerning trend in pediatric healthcare. These findings underscore the importance of understanding pediatric antibiotic use, especially as it relates to rising concerns around antibiotic resistance in children. By addressing this issue through vaccination and education, we can potentially reduce unnecessary prescriptions and improve public health outcomes.
In the realm of child healthcare, prescriptions for antibiotics represent a vital aspect of managing infections that frequently impact the pediatric population. Frequent occurrences of viral ailments, particularly those caused by pathogens like RSV and the flu, lead to significant outpatient antibiotic use among young patients. Analyzing the patterns of these prescriptions helps illuminate the broader implications for childhood illnesses, as many viral respiratory infections often lead to misprescribing of antibiotics. As healthcare professionals strive to balance effective treatment with the urgency of preventing antibiotic resistance in children, understanding the dynamics of outpatient antibiotic dispensing becomes crucial. Strategies focused on vaccination and alternative treatment methods may serve as key interventions to optimize care and minimize unnecessary antibiotic consumption.
Understanding Pediatric Antibiotic Prescriptions
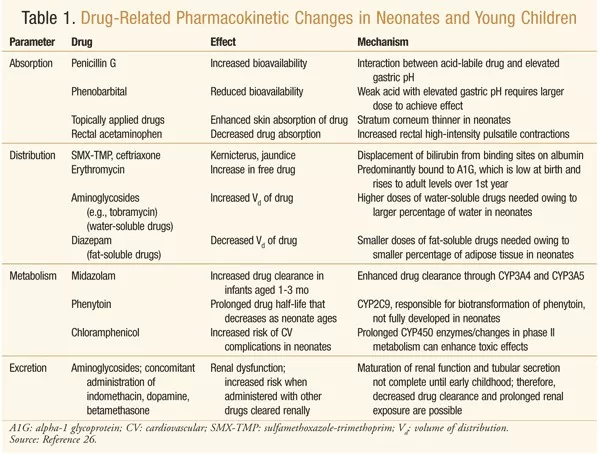
Antibiotic prescriptions for children remain a significant concern in pediatric healthcare. A comprehensive study spanning a decade analyzed antibiotic prescribing patterns among children aged 0 to 17, revealing that a substantial proportion of these prescriptions are linked to respiratory infections. With over 21.5 million outpatient antibiotic prescriptions recorded, it was found that a staggering 66.8% were associated with acute respiratory infections (ARIs), often leading to potential overprescription issues. Doctors must balance treating infections effectively while minimizing the risk of developing antibiotic resistance in children.
The study shows that the incidence of pediatric antibiotic prescriptions due to respiratory viruses such as RSV and influenza is considerably high. Given that more than 72.6 prescriptions per 1,000 children annually were associated with RSV and about 40.0 linked to influenza, it’s crucial for healthcare professionals to review and refine their prescribing practices. Continuous education on the appropriate use of antibiotics and alternatives for managing viral infections may reduce unnecessary prescriptions and combat the growing challenge of antibiotic resistance.
RSV and Influenza’s Role in Antibiotic Prescribing
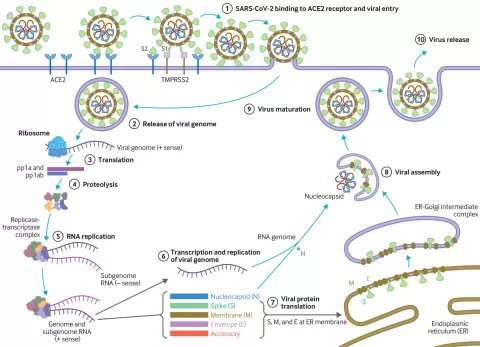
Respiratory syncytial virus (RSV) and influenza have long been recognized as notable contributors to pediatric antibiotic prescriptions. The research highlighted that during peak seasons for RSV, antibiotic prescribing rates soared above 10%, consequently putting younger patients at greater risk for antibiotic-related side effects and resistance. The link between RSV and serious respiratory conditions, such as pneumonia and bronchiolitis, makes it essential for physicians to distinguish between bacterial and viral infections before prescribing antibiotics.
Similarly, influenza is monitored closely for its impact on outpatient antibiotic use, particularly in children over the age of five. With flu-associated antibiotic prescriptions commonly related to viral upper respiratory infections and bronchitis, careful diagnosis is vital. Understanding the biological impact of these viruses not only informs treatment strategies but also plays a pivotal role in addressing broader public health issues like antibiotic resistance. Comprehensive vaccination programs could substantially lower the incidence of these infections and, as a result, reduce the reliance on antibiotics.
Impact of Outpatient Antibiotic Use in Children
Outpatient antibiotic use in children has reached alarming levels, with a significant proportion emerging from ARIs. During the decade reviewed, data showed that conditions like pneumonia, bronchiolitis, and acute otitis media led to increasing antibiotic prescriptions. This trend highlights a critical area for pediatric care improvement, as unwarranted use of antibiotics may contribute directly to the alarming rise in antibiotic resistance, posing a severe health risk to future generations.
Addressing this issue requires a multifaceted approach, including heightened awareness among healthcare providers regarding the implications of overprescribing antibiotics. By implementing educational initiatives that focus on proper diagnostic techniques and treatment guidelines, healthcare professionals can make informed decisions that prioritize patient safety while combating the threat of resistance. This is particularly vital in treating pediatric patients, who are more susceptible to infections and the resulting complications that may arise from incorrect antibiotic use.
Pediatric Respiratory Infections and Treatment Approaches
Pediatric respiratory infections, especially those caused by RSV and influenza, necessitate a careful consideration of treatment alternatives to antibiotics, particularly in light of their significant role in outpatient antibiotic prescribing. With many of these infections being viral, understanding how to manage symptoms without resorting to antibiotics can greatly alleviate unnecessary prescription rates. Health professionals need to focus on supportive care, such as hydration and rest, which often suffice for viral infections.
In addition, incorporating efficient diagnostic tools can further enhance treatment efficacy. For instance, rapid viral testing can help pediatricians identify whether an infection is bacterial or viral, informing whether antibiotics are necessary. This approach not only aids in better patient outcomes but also reduces the overall burden of antibiotic use among children, thereby limiting the risk of developing antibiotic-resistant strains.
The Importance of Vaccination Against Viral Infections
Vaccination plays a pivotal role in preventing not only severe respiratory illnesses like RSV and influenza but also in curtailing the associated antibiotic prescriptions in pediatric populations. Evidence suggests that vaccinations can significantly diminish the incidence and severity of these infections, which subsequently translates to fewer cases requiring antibiotics. The potential for immunization to reduce the burden of disease and the need for antibiotics provides a compelling reason for parents to ensure their children receive recommended vaccinations.
Moreover, the study’s authors assert that enhancing vaccination coverage could lead to long-term benefits in combating antibiotic resistance. Fewer infections would directly result in lower antibiotic consumption, helping to preserve the effectiveness of existing antibiotics for cases where they are truly necessary. Thus, increasing awareness of the importance of vaccination against RSV and influenza is crucial for pediatric public health.
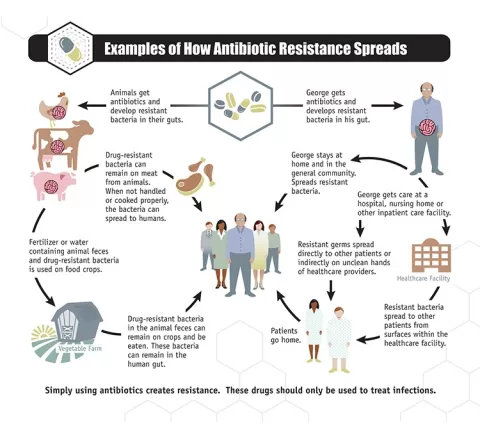
Challenges in Managing Antibiotic Resistance in Children
One of the foremost challenges in pediatric care today is managing antibiotic resistance, particularly in the context of outpatient antibiotic prescriptions for respiratory infections. The study shows that a significant slice of antibiotic prescriptions could be attributed to RSV and influenza, diseases that typically do not require antibacterial treatment. This persistent issue underscores the importance of implementing stewardship programs that educate parents and practitioners alike about appropriate antibiotic use.
Health organizations advocate for a proactive approach that encourages monitoring and adjusting prescription guidelines based on emerging evidence about viral infections. Such policies not only optimize treatment efficacy but are also vital in mitigating the risk of developing resistant strains. The goal is to foster a culture of responsible antibiotic use through better education, guidelines, and communication between healthcare providers and families.
Data Analysis of Antibiotic Prescriptions Over Time
A critical examination of antibiotic prescription data over the last ten years reveals valuable insights into prescribing trends and their correlations with viral outbreaks like RSV and influenza. The findings show considerable variability in prescribing practices year by year, demonstrating how external factors, such as seasonal peaks, can heavily influence outpatient antibiotic use. Identifying these trends is essential to develop targeted interventions aimed at reducing excessive antibiotic prescriptions in pediatrics.
Additionally, patterns of antibiotic prescribing may vary significantly between different demographic groups, including age and underlying health conditions. By analyzing these data, policymakers can better understand which demographics are most affected and tailor educational and preventive strategies accordingly. This nuanced approach allows healthcare providers to engage more effectively with families about the importance of judicious antibiotic use and vaccinations.
Community Awareness and Education on Pediatric Antibiotics
Raising community awareness about the implications of pediatric antibiotic use is essential for reducing unnecessary prescriptions and addressing antibiotic resistance. Parents, guardians, and caregivers must be informed about the common viral illnesses that affect children and understand the circumstances under which antibiotics should be used. Educational initiatives can empower families to consult healthcare professionals effectively while advocating for appropriate treatment options.
Furthermore, local health departments and practices should collaborate to disseminate information regarding the latest research on pediatric respiratory infections and antibiotic stewardship. Public health campaigns can enhance understanding of how to manage common illnesses without depending on antibiotics, promoting a culture of informed health choices within communities. This collective effort can ultimately lead to a decrease in pediatric antibiotic prescriptions, benefiting child health and mitigating the looming threat of antibiotic resistance.
Future Directions in Pediatric Antibiotic Use
The future of pediatric antibiotic prescribing will likely be shaped by ongoing research and innovations in healthcare strategies. As more data accumulates, healthcare systems can leverage information to refine antibiotic prescribing practices further and develop more effective Outpatient Antibiotic Stewardship Programs. By focusing on evidence-based guidelines and increasing access to diagnostic tests, practitioners can significantly enhance their ability to make informed choices when treating children.
In addition, continual investment in vaccine development and education initiatives surrounding childhood immunizations will play a crucial part in shaping antibiotic use. As vaccines improve and become more widely adopted, the incidence of RSV and influenza will likely decrease, thereby directly influencing antibiotic consumption trends. Moving forward, a collaborative approach involving healthcare providers, public health officials, and families will be integral to cultivating a future where antibiotic use is aligned with best practices and preserves the efficacy of these vital medications.
Frequently Asked Questions
What are pediatric antibiotic prescriptions linked to RSV and influenza?
Pediatric antibiotic prescriptions linked to RSV (respiratory syncytial virus) and influenza represent a significant portion of outpatient antibiotic use. A recent study indicates that 6.3% of antibiotics prescribed to children were associated with RSV and 3.4% with influenza. This highlights the need for careful diagnosis and consideration of viral causes before prescribing antibiotics.
How do pediatric respiratory infections influence antibiotic prescribing rates?
Pediatric respiratory infections, particularly RSV and influenza, greatly influence antibiotic prescribing rates. Research shows that about two-thirds of outpatient antibiotic prescriptions for children are related to acute respiratory infections. This indicates the importance of appropriate treatment strategies to avoid unnecessary antibiotic use.
What role does antibiotic resistance play in pediatric antibiotic prescriptions?
Antibiotic resistance in children is a growing concern and is exacerbated by inappropriate antibiotic prescriptions for viral infections like RSV and influenza. Vaccination and preventive measures can help reduce the incidence of these viruses, potentially decreasing unnecessary antibiotic use and combating antibiotic resistance.
How can vaccination impact pediatric antibiotic prescriptions for respiratory infections?
Vaccination against RSV and influenza may significantly impact pediatric antibiotic prescriptions. By reducing the incidence of these infections, vaccinations can lower the associated antibiotic prescribing rates, thereby contributing to efforts to combat antibiotic resistance in children.
What trends have been observed in outpatient antibiotic use among children?
Trends in outpatient antibiotic use among children show that a large proportion, specifically 66.8%, are linked to respiratory infections like RSV and influenza. This data reveals a need for improved awareness among healthcare providers regarding antibiotic stewardship, particularly in pediatric populations.
What specific age group is most affected by RSV-associated antibiotic prescriptions?
The age group most affected by RSV-associated antibiotic prescriptions consists of children aged 5 years and under. This demographic shows higher rates of antibiotic prescriptions due to complications like pneumonia, bronchiolitis, and acute otitis media.
Are pediatric antibiotic prescriptions for flu higher in specific age groups?
Yes, pediatric antibiotic prescriptions associated with influenza are more prevalent in children over 5 years old. These prescriptions are often linked to viral upper respiratory infections and bronchitis, emphasizing the varying impact of influenza across different age groups.
| Key Points |
|---|
| A study analyzed US pediatric outpatient prescriptions over 10 years for children aged 0-17 years. |
| Flu and RSV significantly contribute to pediatric antibiotic prescriptions, especially during peak seasons. |
| Over 21.5 million outpatient antibiotic prescriptions were dispensed, with 66.8% linked to acute respiratory infections. |
| 6.3% of prescriptions were associated with RSV, and 3.4% with influenza, translating to 72.6 and 40.0 prescriptions per 1,000 children annually, respectively. |
| RSV prescriptions were more common in children under 5, linked to pneumonia and bronchiolitis; flu prescriptions were more common in older children. |
| Findings support vaccination to reduce debt burden from RSV and influenza and potentially reduce antibiotic prescriptions. |
Summary
Pediatric antibiotic prescriptions are significantly influenced by the incidence of respiratory viruses such as RSV and influenza. A recent study highlighted that these viruses account for a notable percentage of antibiotic use in children, particularly during peak infection seasons. By supporting vaccination efforts against these pathogens, we can reduce both the disease burden and the reliance on antibiotics, which is crucial for combating antibiotic resistance. Mitigating unnecessary prescription rates not only benefits children’s health but also has broader implications for public health.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.