The pandemic impact on malaria has revealed profound implications for public health, highlighting how COVID-19 disruptions have exacerbated the global disease burden. As healthcare resources dwindled during the height of the pandemic, malaria cases increased alarmingly, particularly among vulnerable populations such as children under five. The neglect experienced by tropical disease prevention efforts during COVID-19 has led to a concerning rise in both malaria-related morbidity and mortality rates. Furthermore, the mental health consequences of the pandemic, including rising incidences of anxiety and depression, have compounded the overall health crisis, leading to a dual burden on healthcare systems. It is crucial to address these interconnected challenges to rebuild resilient health infrastructures capable of withstanding future emergencies.
The repercussions of the global health crisis on malaria demonstrate a complex interplay between infectious diseases and mental well-being. Recent findings suggest that healthcare disruptions during the pandemic have surged malaria incidents, underscoring the urgency for targeted actions to combat this preventable disease. Alongside this, the escalating rates of psychological disorders signal a growing burden on healthcare services exacerbated by the stressors of COVID-19. This unprecedented increase in illness, both physically and mentally, necessitates a reevaluation of public health strategies to improve disease management and mitigation efforts. Through understanding the multifaceted impact of the pandemic, we can better prepare for and address future health challenges.
The Pandemic’s Impact on Malaria Cases
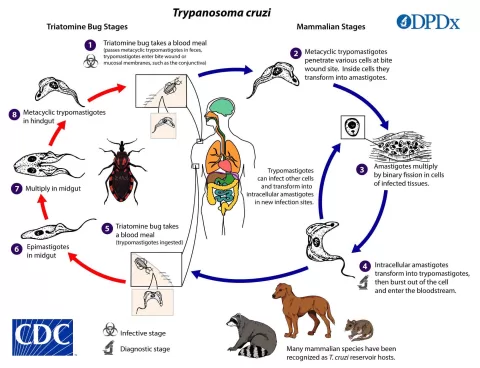
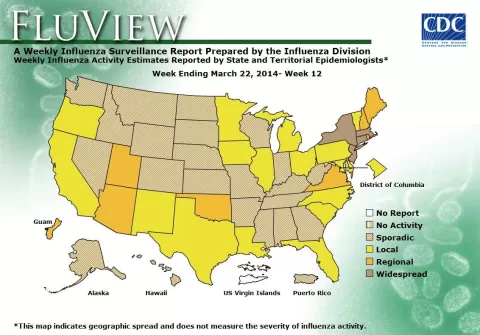
The COVID-19 pandemic has profoundly disrupted global health systems, contributing to an alarming rise in malaria cases. According to a recent study published in BMJ, the healthcare disruptions caused by the pandemic led to a substantial decline in routine immunizations and preventive healthcare services. This disruption was particularly detrimental in low-resource settings, where malaria prevention programs were scaled back, leading to missed opportunities for preventive treatments and control measures that are critical for reducing malaria transmission.
The data indicates that in the first year following the onset of the pandemic, cases of pediatric malaria surged significantly, reflecting both an increased disease burden and a lack of timely healthcare interventions. Children under five years are especially vulnerable to malaria; thus, the impact of the pandemic on healthcare availability inevitably exacerbated this situation. The increase in malaria cases can be viewed as part of a broader pattern of rising disease burdens associated with COVID-19 that highlights the interconnectedness of health crises.
Mental Health Crisis During and After the Pandemic
The COVID-19 pandemic has also precipitated a significant rise in mental health disorders alongside the surge in infectious diseases like malaria. Researchers found a staggering increase in depressive and anxiety disorders, with absolute rates jumping considerably during the pandemic. The impact of isolation, uncertainty, and socioeconomic disruptions triggered by COVID-19 contributed to a deterioration of mental health for many individuals, particularly for vulnerable populations such as women and young adults aged 15 to 49.
The mental health effects during the pandemic are severe, yet they may not have been fully assessed during the height of crisis management. The pandemic’s influence on mental health illustrates a syndemic model, where multiple health crises converge, compounding overall morbidity. As healthcare systems prioritized COVID-19 responses, mental health services often faced significant cuts, leading to underdiagnosed and undertreated mental health issues which could be long-lasting and deeply ingrained beyond the pandemic period.
Healthcare System Disruptions and Their Consequences
The increased burden of diseases such as malaria and mental health disorders during the pandemic underscores the critical vulnerabilities within our healthcare systems. The analysis of healthcare disruptions revealed that many preventive health services and treatments were deprioritized or completely halted. This shift in focus had a cascading effect on the ability to manage existing diseases, reflecting an important lesson on the necessity of resilience in health systems.
Addressing these issues calls for immediate action. Strengthening healthcare resilience through integrated disease surveillance and adaptable healthcare strategies will be crucial in preparing for future public health crises. The pandemic’s impact has highlighted the interconnected nature of various health issues and the need for a holistic approach to public health that prioritizes prevention, treatment, and mental health support alongside infectious disease control.
Integrating Mental Health and Infectious Disease Response
The COVID-19 pandemic has shown just how interconnected physical health and mental well-being can be, emphasizing the need for integrated response strategies. The simultaneous rise in malaria cases and mental health disorders necessitates a comprehensive public health approach that addresses both the physical and mental health needs of communities. By integrating mental health services into infectious disease response plans, healthcare providers can ensure that patients receive comprehensive care that addresses both their physical and psychological health.
Such integration could include training healthcare professionals to identify and manage mental health issues among malaria patients or ensuring access to mental health resources during malaria treatment protocols. This will not only improve individual patient outcomes but also enhance community health as a whole. As we move forward, the dual impact of COVID-19 on both malaria and mental health signifies an urgent call to evolve our healthcare systems and strategies.
Long-Term Public Health Implications of the Pandemic
The long-term implications of the COVID-19 pandemic on public health are yet to be fully understood. However, preliminary studies indicate potential lasting consequences, such as increased disability-adjusted life years (DALYs) for diseases like malaria and mental disorders. As disruptions continue to unfold, it is essential to conduct ongoing research to assess how the pandemic has shifted disease trends and healthcare needs over time.
The increase in morbidity from malaria and mental health conditions indicates a growing burden that health systems must learn to manage effectively. The findings underscore the importance of maintaining a balanced focus on both infectious diseases and non-communicable conditions to address the dual threats facing public health today. Future health emergencies will demand a resilient infrastructure that can adapt to simultaneous health challenges.
The Importance of Preventive Healthcare in Crisis
One of the key lessons learned from the COVID-19 pandemic is the importance of preventive healthcare. The decline in routine immunizations and health services during the pandemic contributed significantly to increases in malaria and mental health disorders. Failing to prioritize preventive measures can lead to catastrophic increases in disease burden, showcasing the vital role that prevention plays in maintaining public health.
Going forward, health systems must bolster their preventive care strategies and ensure that all aspects of health are addressed, especially in times of crisis. By prioritizing preventive healthcare in policy decisions, we can better prepare to mitigate the effects of future pandemics and sustain the overall health of populations globally.
Strengthening Global Health Systems for Future Challenges
The disruptions caused by the COVID-19 pandemic have illuminated critical gaps in global health systems that must be addressed to effectively respond to future health challenges. Strengthening health systems not only involves improving the scalability of responses to common infectious diseases like malaria but also preparing for the complexities of managing mental health during public health emergencies.
Investment in health infrastructure, training, and resources that promote both physical and mental health aspects can help create a more resilient global health environment. Adopting syndemic-informed strategies and enhancing comprehensive health initiatives will be crucial in minimizing the impact of future pandemics and improving health outcomes across populations.
Raising Public Awareness and Education
Public awareness and education are integral components in addressing both malaria and mental health within the context of pandemic recovery. As communities emerge from the COVID-19 crisis, educational campaigns that inform individuals about the dangers of malaria combined with mental health resources can pave the way for healthier outcomes. Knowledge empowers individuals to seek appropriate care and preventive measures, ultimately reducing infection rates and supporting mental well-being.
Multidisciplinary approaches that weave together information on malaria prevention and mental health strategies can be particularly effective. Targeting vulnerable populations, such as parents and caregivers of young children, with education about malaria symptoms, transmission, and mental health support systems can encourage proactive health-seeking behaviors. Empowering communities through education is essential for mitigating the long-term effects of the pandemic on public health.
Research and Data Collection: A Call to Action
A critical component of addressing the multifaceted health challenges brought on by the pandemic lies in robust research and data collection. As the pandemic revealed, data gaps for diseases like malaria and emerging mental health trends need to be filled to formulate effective public health strategies. The Global Burden of Disease Study 2021 has set a framework for understanding the interplay between various health issues, but continued efforts are necessary for accurate assessment.
Future research should focus on longitudinal studies that track disease burden and health outcomes post-pandemic, providing necessary insights for policymakers. By committing to ongoing research initiatives and facilitating data sharing among countries and agencies, we can enhance our understanding of health challenges and apply learned knowledge to better respond to global health threats.
Frequently Asked Questions
How has the COVID-19 pandemic impacted malaria cases globally?
The COVID-19 pandemic significantly disrupted healthcare systems worldwide, leading to an increase in malaria cases. Routine immunizations and treatment for malaria faced severe setbacks, contributing to a 12.2% rise in disability-adjusted life years (DALYs) related to malaria in 2020-2021. Vulnerable populations, particularly children under five, were the most affected.
What is the relationship between the pandemic and increased mental illness related to malaria?
The COVID-19 pandemic’s impact on healthcare has led to rising mental health issues, particularly anxiety and depression, alongside the burden of malaria. The disruption in medical services and decreased access to malaria treatment exacerbated the stress and mental health challenges faced by individuals living with or at risk for malaria.
What are the consequences of the pandemic impact on healthcare for malaria prevention?
The pandemic resulted in reduced funding and resources for tropical disease prevention, including malaria. With decreased healthcare access, routine treatments and preventative measures were delayed, culminating in a significant rise in malaria cases and related complications.
Why are children under five disproportionately affected by malaria during the pandemic?
Children under five have a higher vulnerability to malaria due to their developing immune systems. The COVID-19 pandemic disrupted essential healthcare services, including routine malaria treatment and preventive measures like immunizations, which are crucial for this age group. Consequently, there was a marked increase in malaria cases among young children.
What strategies can mitigate the pandemic impact on malaria-related health outcomes?
To mitigate the pandemic’s impact on malaria, it is essential to strengthen health system resilience, enhance integrated surveillance, and adopt syndemic-informed strategies. These approaches will facilitate a more comprehensive public health response and improve preparedness for future health emergencies.
What do researchers indicate about the overall disease burden during the COVID-19 pandemic?
Researchers indicate that the COVID-19 pandemic led to significant increases in the disease burden for malaria and other conditions, including mental health disorders. The models demonstrated that the combined burdens of these diseases necessitate improved health strategies to support populations affected during pandemics.
How did funding changes during the pandemic affect malaria interventions?
During the COVID-19 pandemic, funding for malaria interventions decreased significantly, hindering ongoing prevention and treatment efforts. This reduction in financial support for healthcare impacted malaria control programs, leading to an increase in malaria cases and worsening health outcomes among affected individuals.
| Key Points | Details |
|---|---|
| COVID-19 Healthcare Disruptions | Pandemic led to increases in illnesses including mental disorders and malaria cases. |
| Impact on Medical Care | Drop in routine immunizations and cancer screenings during pandemic. |
| Funding Cuts | Investment in tropical-disease prevention shrank during the early pandemic. |
| Increase in Malaria Cases | Malaria DALYs increased by 12.2% post-pandemic, especially in children under five. |
| Mental Health Burden | Depressive and anxiety disorders increased by 14.3% and 15.4%, affecting women and young adults. |
| Need for Health System Resilience | Urgent need to strengthen health systems and strategies for future public health emergencies. |
Summary
The pandemic impact on malaria has highlighted critical vulnerabilities within healthcare systems as disruptions during COVID-19 have led to significantly increased cases of malaria and other health issues. The decline in medical services, including routine vaccinations that are vital for disease control, exacerbated malaria incidence, particularly among young children. The alarming rise in malaria-related disability-adjusted life years reflects the cascading effects of the pandemic on public health and stresses the urgent need for comprehensive strategies to reinforce healthcare resilience and preparedness for future health crises.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.