Nosocomial malaria transmission is an emerging concern in healthcare settings, particularly highlighted by recent cases of Plasmodium falciparum malaria in Spain. A troubling incident involving inadequate disinfection practices during medical procedures has brought attention to the urgent need for improved malaria prevention strategies. Insufficient decontamination protocols not only threaten patient safety but also pose a risk of malaria transmission routes that can arise even in non-endemic countries. As Spain continues to monitor its malaria cases, including the 600 recorded imported instances in 2024, the implications for healthcare biosafety have never been clearer. Addressing the risks associated with nosocomial transmission is essential to safeguard public health and prevent potential outbreaks in medical facilities.
Healthcare-associated transmission of malaria, particularly attributed to the Plasmodium genus, is an issue that requires significant attention, especially in regions like Spain, where malaria was historically eradicated. Recent reports of infections acquired in clinical settings have raised alarms about the efficacy of current infection control practices. The transmission mechanisms, previously thought to be limited to vector bites, now include potential indirect routes stemming from unsafe medical procedures. With rising numbers of imported malaria cases, understanding the dynamics of disease spread within hospitals is critical for informing new malaria prevention tactics. Enhanced biosafety measures and rigorous cleaning protocols must be a priority to mitigate risks and protect both patients and healthcare workers.
Understanding Nosocomial Malaria Transmission
Nosocomial malaria transmission represents a significant health risk, particularly in non-endemic regions such as Spain. This phenomenon occurs when malaria is contracted within healthcare facilities, often due to inadequate biosafety measures or the improper handling of medical equipment that may carry pathogens. The recent reports from Spain highlight the importance of recognizing this transmission route, especially as healthcare settings strive to maintain high standards of infection control. With malaria caused by the Plasmodium falciparum parasite, understanding how it can spread nosocomially is crucial in preventing outbreaks.
In the case reported in 2024, a patient acquired P. falciparum malaria through an improperly disinfected medical device. The genomic analysis confirmed both patients shared infection strains, emphasizing how critical it is to enforce strict medical hygiene. Without robust biosafety protocols in place, healthcare facilities could inadvertently become hotspots for malaria transmission, leading to increased cases and placing vulnerable populations at risk. Thus, ongoing education about nosocomial malaria is paramount for healthcare providers in endemic and non-endemic areas alike.
The Role of Healthcare Biosafety in Malaria Prevention
Healthcare biosafety plays a pivotal role in malaria prevention, particularly in settings that do not regularly encounter malaria cases. It is essential for medical facilities to implement rigorous decontamination protocols to prevent the transmission of infectious diseases, including Plasmodium falciparum. Various strategies can enhance biosafety, such as thorough cleaning of reusable medical equipment and adherence to established medical guidelines to mitigate risks. This is especially important in light of increasing numbers of imported malaria cases in places like Spain, where the recent surge underlines the necessity for comprehensive biosafety measures.
An essential component of healthcare biosafety involves educating medical staff about malaria transmission routes and the importance of preventative measures. This includes proper sterilization techniques and monitoring of patients who may show atypical symptoms of malaria. Ensuring that all medical personnel are trained in biosafety practices will help mitigate risks associated with nosocomial infections. Consequently, strengthening these protocols can effectively reduce the chances of malaria transmission within healthcare settings, safeguarding both patients and healthcare workers from potential outbreaks.
Investigating Malaria Transmission Routes
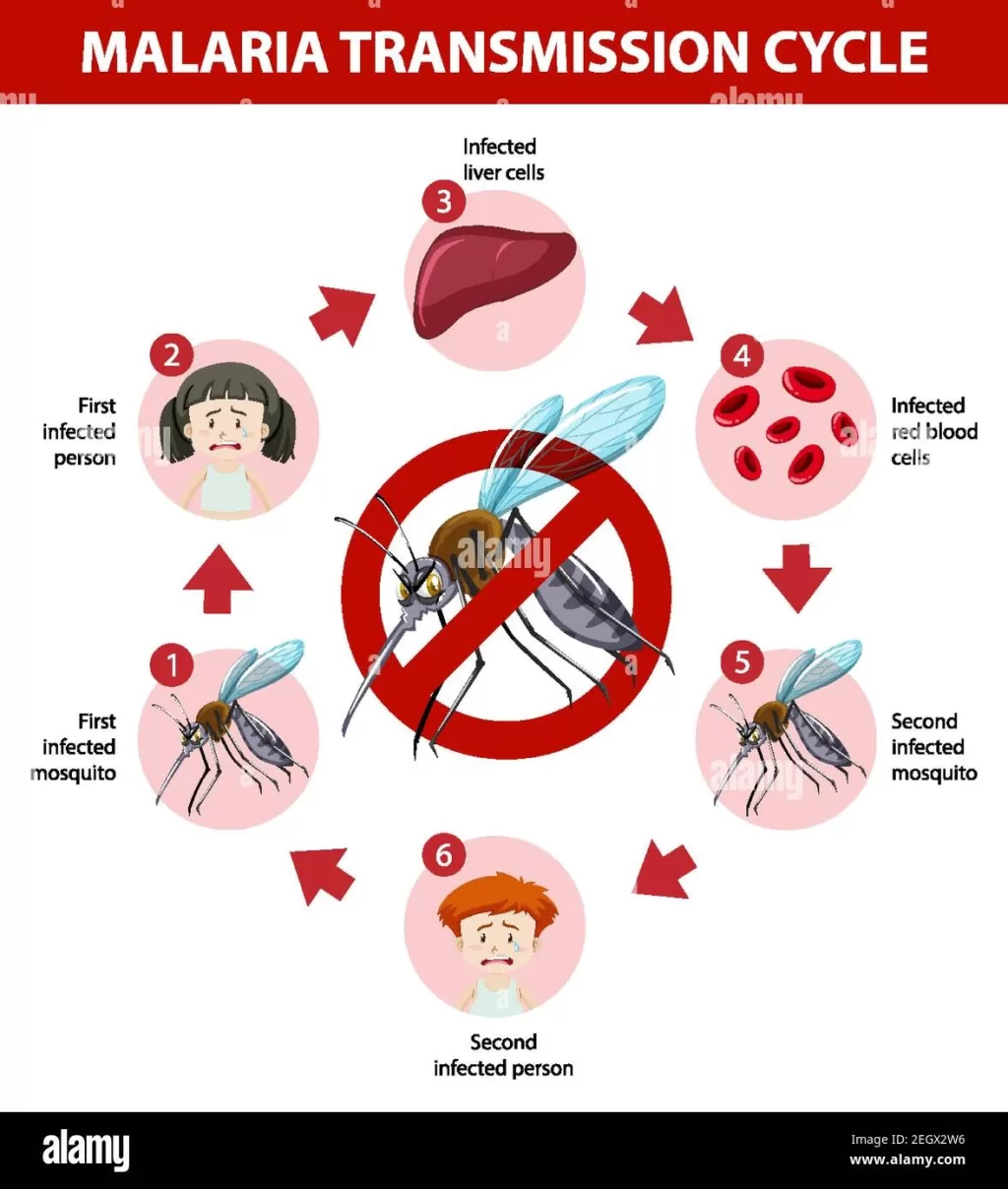
Understanding malaria transmission routes is vital for effectively controlling and preventing the spread of this parasitic disease. Primarily transmitted through the bites of infected Anopheles mosquitoes, malaria can also be acquired through blood products, organ transplants, and—most alarmingly—nosocomial routes as illustrated in Spain’s recent case study. By identifying these various routes, health authorities can implement targeted strategies to curb transmission and educate at-risk populations on preventive measures.
The emergence of nosocomial malaria cases stresses the need to investigate and understand all potential pathways of transmission, especially in areas where malaria had been practically eradicated. This includes thorough epidemiological investigations of new cases, which can reveal unexpected transmission chains. For example, the patient from the Spanish case had never traveled abroad or received blood transfusions, highlighting that non-vector transmission methods can also lead to new infections. Investigating these routes will support public health efforts in creating effective intervention strategies tailored to the unique challenges faced in different geographic regions.
Epidemiological Investigations in Malaria Case Studies
Epidemiological investigations play a crucial role in understanding malaria case dynamics, especially when nosocomial infections arise. In harvesting insights from recent cases in Spain, health officials can trace the origins of infections and assess the risk factors involved. The case of the 60-year-old female patient underscores the significance of thorough investigations. Through analyzing her medical history and recent procedures, healthcare professionals confirmed that her infection was contracted in a hospital setting, which emphasizes the need for vigilance in healthcare environments.
Expanding epidemiological research beyond traditional malaria hotspots is essential in developing a comprehensive understanding of how malaria spreads. By documenting and analyzing each newly reported case, health authorities can better evaluate the effectiveness of current preventive measures and adapt public health strategies accordingly. Such investigations will be instrumental in establishing a proactive stance in combating malaria, particularly in Europe, where the recent increase in cases, including those categorized as imported and nosocomial, prompts a reevaluation of current approaches to healthcare biosafety and disease prevention.
Challenges of Malaria Prevention in Non-Endemic Regions
Preventing malaria in non-endemic regions poses unique challenges that require innovative solutions. With increasing global travel and migration patterns, imported malaria cases have become more common, complicating traditional approaches to malaria prevention. Countries like Spain, which once eradicated endemic malaria, now encounter new cases primarily linked to travelers returning from regions where Plasmodium falciparum is endemic. This resurgence highlights the importance of preparing healthcare systems to manage unexpected infections effectively.
Moreover, the challenges of nosocomial malaria transmission further complicate prevention efforts. In non-endemic areas, healthcare professionals may not be as familiar with the signs and symptoms of malaria, leading to underdiagnosis or misdiagnosis. This lack of familiarity can delay necessary treatment for patients, potentially resulting in severe complications or outbreaks. Therefore, continuous education and awareness campaigns focusing on malaria symptoms, transmission routes, and preventive measures are critical to empowering healthcare professionals and safeguarding public health.
Importance of Rapid Diagnostics in Malaria Cases
Rapid diagnostics are vital for timely malaria detection and treatment, especially in non-endemic settings where healthcare providers may have limited experience with the disease. In the context of increasing nosocomial malaria cases, implementing rapid diagnostic tests can help quickly identify infections caused by Plasmodium falciparum and initiate appropriate treatment. This quick turnaround not only aids in individual patient recovery but also helps prevent further transmission within healthcare facilities.
By incorporating rapid diagnostic tools into routine healthcare practices, medical professionals are better equipped to respond to suspected malaria cases effectively. This practice can significantly reduce hospitalization times and improve clinical outcomes for patients, ultimately leading to a decrease in nosocomial transmission. Moreover, enhancing diagnostic capacities allows for better data collection, which is crucial for understanding malaria epidemiology and developing targeted public health strategies.
Educational Initiatives for Healthcare Providers
Educational initiatives targeting healthcare providers are essential for enhancing the understanding of malaria prevention and the risk of nosocomial infections in non-endemic regions. Ongoing training programs can equip medical staff with necessary knowledge about pathogens, infection control measures, and the specific risks associated with procedures that could lead to malaria transmission, such as blood transfusions and surgeries. These initiatives can serve to bridge knowledge gaps and foster an environment of proactive disease prevention.
Additionally, creating comprehensive educational resources, such as online courses, workshops, and informational brochures, can help spread awareness of malaria’s transmission mechanisms, symptoms, and treatment protocols. Equipping healthcare professionals with updated information is critical for detecting malaria cases quickly and accurately, especially in settings where the disease may not be commonly recognized. Such proactive educational efforts can significantly lower the likelihood of nosocomial malaria transmission and bolster the overall effectiveness of malaria prevention strategies.
The Role of Public Health Policies in Malaria Control
Public health policies play a critical role in controlling malaria and preventing its spread in non-endemic areas. Policymakers must recognize the unique challenges posed by imported cases and nosocomial transmission routes, which can lead to outbreaks in otherwise malaria-free regions. By developing and implementing robust public health strategies and guidelines that account for these challenges, authorities can better safeguard the health of their populations against this infectious disease.
Additionally, fostering collaboration between public health agencies, healthcare providers, and the community can enhance the effectiveness of malaria control measures. Establishing clear communication channels and frameworks for information sharing can ensure that everyone involved is informed about potential risks and best practices for prevention. Consequently, creating a comprehensive approach to malaria control will significantly reduce the risk of transmission—particularly in the context of healthcare settings where the risk of nosocomial infection is heightened.
Future Directions in Malaria Research and Prevention
As malaria remains a global health concern, future research and prevention efforts must adapt to the changing patterns of infection. With the emergence of nosocomial malaria cases in previously unaffected regions, it is critical for scientists and healthcare professionals to investigate new methodologies for disease control and prevention. Innovations in diagnostic technology, treatment options, and public health initiatives will be crucial in addressing the multifaceted challenges posed by malaria.
Moreover, fostering international collaboration in malaria research can enhance understanding and response strategies to this complex disease. By sharing data on malaria transmission mechanisms, particularly in healthcare settings, researchers can develop evidence-based guidelines for disease management and prevention. As the world continues to grapple with malaria, a focus on integrating research findings into practical applications will be essential in mitigating the risk of both endemic and non-endemic malaria transmission.
Frequently Asked Questions
What is nosocomial malaria transmission and how does it relate to Plasmodium falciparum?
Nosocomial malaria transmission refers to the spread of malaria within healthcare settings, often due to inadequate biosafety measures. This transmission is particularly linked to Plasmodium falciparum, the most severe malaria-causing protozoan, which can be contracted through contaminated medical equipment or from asymptomatic patients. In Spain, recent cases highlighted the risks associated with insufficiently disinfected devices in hospitals.
How can healthcare biosafety prevent nosocomial malaria transmission?
Healthcare biosafety protocols are crucial in preventing nosocomial malaria transmission. This includes strict disinfection of medical equipment, proper usage of protective gear, and monitoring of patients for any malaria-related symptoms, particularly in regions like Spain where malaria is rare but can occur. By implementing robust cleaning protocols and ensuring thorough training of staff, healthcare facilities can significantly reduce the risk of malaria transmission.
What recent cases of malaria transmission have been reported in Spain related to nosocomial infection?
In 2024, Spain reported several nosocomial cases of malaria, specifically involving Plasmodium falciparum. Among the 600 imported cases, two cases were acquired within a hospital setting. Investigations revealed that these infections were likely contracted during medical procedures involving improperly disinfected equipment, emphasizing the importance of strict healthcare protocols.
What are the implications of nosocomial malaria transmission for malaria prevention strategies?
The implications of nosocomial malaria transmission for malaria prevention strategies are significant. Healthcare facilities must focus on improving biosafety measures and infection control protocols to prevent the spread of infections like Plasmodium falciparum in non-endemic regions. This includes enhancing cleaning procedures for reusable medical instruments and ensuring that staff are trained to identify and mitigate potential risks.
Why is it important to understand malaria transmission routes in a non-endemic country like Spain?
Understanding malaria transmission routes in non-endemic countries like Spain is critical for public health and safety. It helps in identifying potential reservoirs of infection and implementing necessary biosafety measures to prevent nosocomial transmission. Enhanced awareness of how Plasmodium falciparum can spread in healthcare settings enables timely interventions to protect patients and healthcare workers.
How does genetic analysis contribute to understanding nosocomial malaria transmission?
Genetic analysis plays a vital role in understanding nosocomial malaria transmission by establishing the similarity between infection isolates from patients. In the case reported in Spain, genomic studies confirmed that the infections were closely related, confirming the likelihood of transmission within the hospital. This kind of analysis strengthens epidemiological investigations and aids in creating effective containment strategies.
| Key Point | Details |
|---|---|
| Nosocomial Malaria Transmission | Plasmodium falciparum malaria was transmitted in a Spanish hospital setting. |
| Syringe Contamination | Insufficiently disinfected reusable syringe lead shielding was identified as the cause of transmission during thyroid scintigraphy. |
| Genomic Analysis | High similarity was found between isolates from the index and source cases, confirming nosocomial transmission. |
| Case Overview | A 60-year-old female patient contracted malaria after undergoing thyroid scintigraphy, without travel history or blood transfusions. |
| Epidemiological Importance | Frequent nosocomial acquisitions were noted along with increased imported cases, emphasizing the need for vigilance in healthcare settings. |
| Biosafety Recommendations | Enhanced decontamination protocols and strict adherence to biosafety measures are essential to prevent nosocomial malaria transmission. |
Summary
Nosocomial malaria transmission is a critical concern for healthcare facilities, particularly in non-endemic regions like Spain. This case highlights the urgent need for enhanced biosafety protocols and rigorous cleaning procedures to prevent similar occurrences in the future. Ensuring the safe use of medical equipment, especially in environments where malaria is not commonly found, is vital to mitigate potential health risks associated with these infections.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.