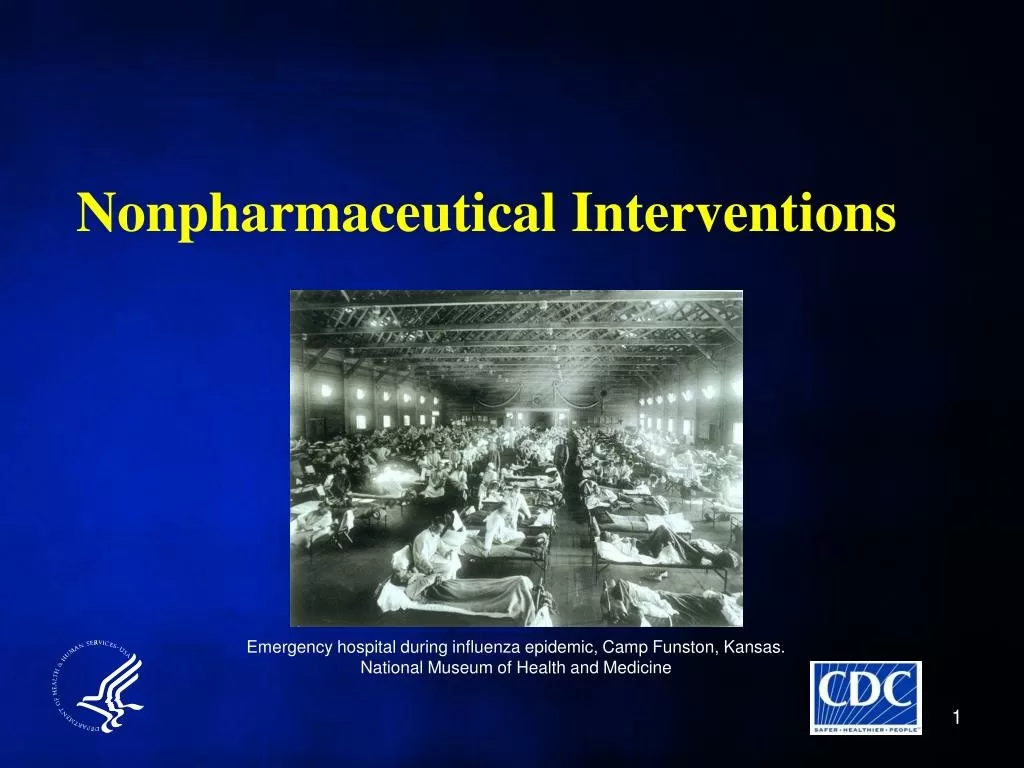
Nonpharmaceutical interventions (NPIs) played a crucial role during the 1918–1920 influenza pandemic, particularly in Alaska, where the spread of the virus posed significant threats to community health. As public health measures were implemented, various agencies worked tirelessly to protect the populace from infection through community health interventions such as quarantine, travel restrictions, and the closure of public spaces. These proactive strategies not only helped reduce the transmission of the virus but also mitigated severe mortality rates in the region, showcasing the effectiveness of NPIs in infectious disease management. By studying Alaska’s pandemic response, we can gain valuable insights into the vital importance of NPIs during health crises, highlighting their relevance in contemporary public health strategies. Understanding the past enables us to prepare better for future outbreaks, ensuring that we can implement effective NPIs to safeguard our communities.
In the context of public health, alternative strategies known as nonmedical interventions are critical for managing infectious disease outbreaks. These approaches encompass a range of actions designed to curb the spread of diseases without relying on pharmaceuticals, such as enforceable lockdowns, social distancing measures, and education campaigns. During historical crises like the Alaska response to the 1918 influenza epidemic, these interventions proved invaluable in preserving community health and preventing widespread morbidity. By leveraging community-based tactics and protective measures, we can draw lessons from the past to enhance our preparedness for future pandemics. Emphasizing the importance of these alternatives ensures a holistic approach to public health, particularly for vulnerable populations.
Understanding the Impact of Nonpharmaceutical Interventions
Nonpharmaceutical interventions (NPIs) played a crucial role in managing the 1918 influenza pandemic, particularly in Alaska, where remote communities faced unique challenges during this public health crisis. NPIs such as quarantines, travel restrictions, and the prohibition of public gatherings were implemented with the goal of minimizing virus transmission. These measures were vital in preventing the introduction and spread of influenza in small, isolated populations, who were more susceptible to severe outcomes due to limited healthcare resources and unique social dynamics.
Historical analysis reveals that communities which adhered to NPIs not only lowered their infection rates but also experienced reduced mortality from pneumonia and influenza. Case studies of Alaskan communities indicate that both voluntary and mandatory measures effectively shielded many Indigenous populations from the worst effects of the pandemic. By examining these strategies, it becomes evident that NPIs serve as a foundational element in public health responses to infectious disease outbreaks, especially in high-risk regions.
Lessons Learned from the 1918 Influenza Pandemic
The 1918 influenza pandemic offers invaluable lessons regarding infectious disease management that remain applicable today. One major takeaway is the importance of timely and decisive public health measures. For Alaska, early responses such as quarantine regulations significantly reduced the likelihood of widespread contagion. These strategies highlight how proactive approaches to public health not only protect populations but also foster community resilience in the face of emerging health threats.
Moreover, this pandemic underscored the critical role of community health interventions. Local decision-makers, responding to guidance from state authorities, implemented tailored NPIs based on the unique circumstances of their regions. This local adaptability proved essential as different areas faced varying levels of exposure risk. In retrospect, the ability to pivot and adjust health interventions reinforces the concept that local contexts should dictate public health strategies in combating infectious diseases.
The Role of Public Health Measures in Alaskan Communities
During the 1918-1920 influenza pandemic, Alaskan communities utilized a variety of public health measures to safeguard their population. The territorial government, understanding the grave risk posed by the virus, enacted comprehensive regulations that mandated isolation, school closures, and the banning of public gatherings. These measures were critical in mitigating the outbreak’s impact and exemplified an organized approach to disease management rooted in community cooperation.
In particular, Indigenous communities that adopted NPIs often found themselves at an advantage during the pandemic. Many used a combination of traditional practices and modern public health recommendations to fortify their defenses against the influenza virus. This melding of cultural insights with formal health measures highlights the effectiveness of culturally relevant interventions in public health initiatives, paving the way for more effective responses in future pandemics.
Community Health Interventions and Their Effectiveness
Community health interventions implemented during the 1918-1920 influenza pandemic, particularly in Alaska, were a vital component of the response and control efforts. Through the identification of high-risk activities and environments, communities were able to tailor strategies that effectively reduced transmission. For instance, public awareness campaigns helped educate residents on the importance of hygiene and social distancing, which were crucial in an era lacking widespread medical interventions.
The success of these community interventions emerged not only from their flexibility but also from the local engagement they fostered. Stakeholders within the communities, from leaders to health workers, collaborated to disseminate information and enforce regulations, ensuring that residents understood the reasoning behind these measures. This community-driven approach resulted in a more cohesive effort against the pandemic and highlighted the necessity of local involvement in public health initiatives.
Indigenous Communities and Pandemic Resilience
Indigenous communities in Alaska exhibited remarkable resilience during the 1918 influenza pandemic, largely attributed to their swift implementation of NPIs. Many of these communities used their understanding of traditional practices alongside government directives to create an effective barrier against the spread of the virus. Voluntary isolation, avoidance of large gatherings, and the enforcement of hygiene protocols were critical strategies that allowed some Indigenous groups to minimize their exposure to influenza.
Furthermore, the adaptability of Indigenous health practices served as a model for effective pandemic response. These communities relied on collective decision-making and historical knowledge of past outbreaks to navigate the crisis. This resilience underscores the importance of integrating community wisdom into contemporary public health planning, especially as we confront modern infectious disease threats.
Quarantine Protocols: A Historical Overview
Quarantine protocols emerged as a fundamental component of Alaskan public health responses during the 1918 influenza pandemic. In an era characterized by limited medical knowledge and scarce resources, the establishment of quarantines aimed to safeguard the health of communities at risk. These protocols restricted movement into and from affected areas, effectively curtailing the spread of influenza and limiting exposure to the virus.
Historical records show that adherence to these quarantine measures correlated with lower mortality rates in various regions across Alaska. The strict application of isolation and travel restrictions provided critical insights into the efficacy of NPIs. Understanding the dynamics of quarantine from the 1918 pandemic emphasizes the importance of maintaining such strategies in modern infectious disease management.
The Importance of Travel Restrictions During the Pandemic
Travel restrictions played an essential role in curbing the spread of the influenza virus during the 1918-1920 pandemic, particularly in the under-resourced regions of Alaska. By limiting the movement of individuals across regions, public health officials aimed to prevent the introduction of influenza into areas that had yet to experience outbreaks. Historical data indicate that communities that imposed strict travel bans were able to slow the transmission of the virus considerably.
In addition to protecting uninfected communities, travel restrictions helped public health authorities manage the logistics of response efforts more effectively. With fewer individuals moving between regions, officials could concentrate resources such as medical supplies and personnel on areas where outbreaks were occurring. This focused approach not only facilitated better resource management but also underscored the efficacy of travel restrictions in managing infectious disease spread.
Analyzing Mortality Rates in Relation to Public Health Measures
The correlation between public health measures and mortality rates during the 1918 influenza pandemic reveals critical insights into effective response strategies. In Alaska, areas that implemented NPIs such as social distancing, school closures, and public gathering bans reported substantially lower mortality rates. This correlation suggests that proactive public health measures can significantly alter the trajectory of disease outbreaks and their fatal consequences.
By analyzing the demographics and infection rates across different Alaskan communities, it’s evident that those which adhered strictly to public health guidance experienced fewer severe outcomes. This historical precedent carries profound implications for contemporary public health strategies, emphasizing the necessity of swift action and the implementation of NPIs to safeguard vulnerable populations during infectious disease crises.
Future Preparedness: Building on the 1918 Experience
Looking ahead, the lessons learned from the 1918 influenza pandemic provide a vital framework for future preparedness initiatives. As infectious diseases continue to pose threats globally, it is crucial for public health agencies to draw from historical successes and failures. Incorporating NPIs and community-driven strategies into pandemic response plans could significantly enhance resilience in the face of emerging health crises.
Moreover, utilizing digitized historical records and data from past pandemics can offer insights into effective health interventions and allow for improved forecasting and planning. By embracing a comprehensive approach that combines historical understanding with contemporary public health methodologies, communities can better prepare for the challenges of future pandemics, ensuring protected populations, particularly those most vulnerable to infectious diseases.
Frequently Asked Questions
What are nonpharmaceutical interventions (NPIs) and how were they applied during the 1918 influenza pandemic?
Nonpharmaceutical interventions (NPIs) are actions taken to prevent the spread of infectious diseases without the use of medications. During the 1918 influenza pandemic, NPIs included travel restrictions, quarantine, isolation of infected individuals, banning public gatherings, and school closures. These measures played a crucial role in slowing the spread of the virus, particularly in Alaska, where communities that implemented NPIs experienced lower mortality rates.
How did nonpharmaceutical interventions influence the community health response in Alaska during the 1918 pandemic?
In Alaska during the 1918 pandemic, NPIs significantly influenced public health measures by allowing communities to control virus transmission. Local units that adopted NPIs, such as isolation and public gathering bans, effectively managed to either prevent outbreaks or reduce the spread after infection introduction. This strategic community health response proved crucial in protecting vulnerable populations, particularly Indigenous communities.
What lessons can be learned from Alaska’s use of nonpharmaceutical interventions in the management of infectious diseases?
Alaska’s experience with NPIs during the 1918 influenza pandemic offers vital lessons for future infectious disease management. Proactive measures, such as early quarantine and travel restrictions, were effective in mitigating disease impact. The success observed in Alaskan communities highlights the importance of preparedness and swift implementation of public health measures to protect at-risk populations in future pandemics.
What types of nonpharmaceutical interventions were most effective in reducing influenza transmission during the 1918–1920 pandemic?
During the 1918–1920 influenza pandemic, nonpharmaceutical interventions such as quarantine, school closures, and restrictions on public gatherings were notably effective in reducing transmission. In Alaska, communities that adhered to these NPIs reported significantly lower rates of pneumonia and influenza deaths, underscoring their effectiveness in infectious disease management.
How do nonpharmaceutical interventions compare to pharmaceutical measures in controlling infectious diseases?
Nonpharmaceutical interventions (NPIs) are complementary to pharmaceutical measures, particularly in infectious disease management. While vaccines and antiviral medications are critical, NPIs like social distancing, masking, and hand hygiene can be implemented quickly to control outbreaks when pharmaceuticals are not available. The 1918 influenza pandemic demonstrated that NPIs could significantly alter disease trajectories, especially in isolated regions like Alaska.
Why are nonpharmaceutical interventions critical in today’s public health measures?
Nonpharmaceutical interventions remain critical in today’s public health measures as they provide immediate, practical strategies to combat infectious diseases, especially in the absence of vaccines or treatments. The historical context, such as the effectiveness of NPIs during the 1918 influenza pandemic in Alaska, shows their value in reducing transmission and protecting vulnerable populations, highlighting the need for continued emphasis on these strategies in modern health responses.
| Key Point | Details |
|---|---|
| Background and Goals | Limited understanding of NPIs during the 1918-1920 influenza pandemic; study aims to overview agency efforts. |
| Methods | Mixed-method assessment of digitized newspapers and archival materials from 14 local units implementing NPIs. |
| Results | Quarantine and various NPIs (travel restrictions, isolation, etc.) helped control the outbreak. |
| Discussion | Highlights the need for NPIs in future pandemics to protect vulnerable populations. |
Summary
Nonpharmaceutical interventions (NPIs) played a crucial role during the 1918–1920 influenza pandemic, particularly in Alaska, where communities faced unique challenges. The effectiveness of NPIs such as quarantine, travel restrictions, and school closures significantly lowered mortality rates and controlled the virus’s spread. The study underscores the importance of preparing for future pandemics by implementing similar proactive measures to protect vulnerable communities effectively.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.