Neonatal gonococcal conjunctivitis is a serious condition affecting newborns that can result from infection with Neisseria gonorrhoeae, particularly strains resistant to fluoroquinolone antibiotics. This infection highlights significant public health challenges, including the rising threats of antimicrobial resistance and the imperative need for effective ophthalmic prophylaxis during delivery. Maternal screening for sexually transmitted infections (STIs) like gonorrhea remains crucial, especially considering the recent cases indicating failures in prevention strategies. The emergence of fluoroquinolone-resistant strains underscores the potential dangers of inadequate treatment protocols in neonates, necessitating a reassessment of existing guidelines for neonatal conjunctivitis. With this awareness, healthcare professionals must prioritize advances in prevention and treatment to safeguard neonatal health against gonococcal infections.
Gonococcal conjunctivitis in infants, often referred to as neonatal conjunctivitis, can pose severe risks if not promptly addressed. This infection occurs when newborns are exposed to Neisseria gonorrhoeae during childbirth, particularly when maternal screening for STIs is lacking. The rise of fluoroquinolone-resistant Neisseria gonorrhoeae strains complicates treatment options, emphasizing the urgency for effective ophthalmic strategies. Additionally, understanding the dynamics of antimicrobial resistance will aid in improving care protocols for affected neonates. By focusing on comprehensive maternal screening and robust prophylactic measures, we can substantially mitigate the impact of neonatal gonococcal conjunctivitis.
Understanding Neonatal Gonococcal Conjunctivitis
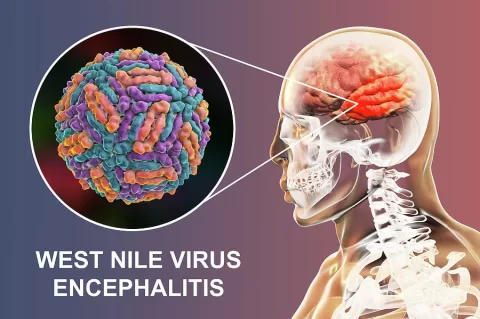
Neonatal gonococcal conjunctivitis is an infection that occurs in newborns, usually transmitted during childbirth from an infected mother. This condition can lead to severe ocular complications if not treated promptly. The condition’s primary causative agent is Neisseria gonorrhoeae, a bacterium known for causing gonorrhea in adults. The case discussed in this research letter highlights the emergence of fluoroquinolone-resistant strains of N. gonorrhoeae, which have raised significant concerns about treatment efficacy and the potential for increased morbidity in newborns.
The incidence of this condition has significantly decreased since the introduction of prophylactic treatments developed by Carl Credé. However, the rise of antimicrobial resistance, particularly with fluoroquinolone-resistant strains, poses a potential threat to the progress made in neonatal care. This calls for a reevaluation of existing prophylaxis strategies in healthcare systems to ensure that they are effective against evolving bacterial resistance patterns.
Frequently Asked Questions
What is Neonatal Gonococcal Conjunctivitis and how is it caused?
Neonatal Gonococcal Conjunctivitis is an eye infection in newborns caused by the bacteria Neisseria gonorrhoeae, which can lead to severe eye damage if untreated. It typically occurs when the bacteria are transmitted from an infected mother during childbirth.
How does fluoroquinolone-resistant Neisseria gonorrhoeae affect the treatment of Neonatal Gonococcal Conjunctivitis?
Fluoroquinolone-resistant Neisseria gonorrhoeae poses a significant challenge in treating Neonatal Gonococcal Conjunctivitis, as conventional treatments using fluoroquinolone-based ophthalmic solutions may be ineffective. Alternative antibiotics, such as cephalosporins, may be required for effective treatment.
What role does ophthalmic prophylaxis play in preventing Neonatal Gonococcal Conjunctivitis?
Ophthalmic prophylaxis, typically administered to newborns shortly after birth, aims to prevent infections like Neonatal Gonococcal Conjunctivitis. Despite its use, cases can still occur, especially if resistant strains of Neisseria gonorrhoeae are present in the mother.
Why is maternal screening for STIs important in preventing Neonatal Gonococcal Conjunctivitis?
Maternal screening for STIs, including Neisseria gonorrhoeae, is crucial in preventing Neonatal Gonococcal Conjunctivitis. Identifying and treating infections in pregnant women reduces the risk of vertical transmission to the infant during delivery.
What are the implications of antimicrobial resistance in the treatment of Neonatal Gonococcal Conjunctivitis?
The rise of antimicrobial resistance, such as fluoroquinolone-resistant Neisseria gonorrhoeae, complicates the treatment of Neonatal Gonococcal Conjunctivitis. It necessitates the development of new treatment protocols and highlights the importance of robust maternal screening and timely interventions.
What symptoms should prompt a medical evaluation for Neonatal Gonococcal Conjunctivitis?
Symptoms of Neonatal Gonococcal Conjunctivitis include purulent ocular discharge, swelling of the eyelids, and redness of the conjunctiva. Any infant showing these signs should receive immediate medical evaluation to prevent complications.
What is the historical significance of prophylactic solutions in preventing Neonatal Gonococcal Conjunctivitis?
Prophylactic solutions, such as the ones first introduced by Carl Credé in 1881, have significantly reduced the incidence of Neonatal Gonococcal Conjunctivitis. However, ongoing cases highlight the need for modern strategies that include enhanced maternal STI screening and effective treatments.
How can healthcare providers improve prevention strategies for Neonatal Gonococcal Conjunctivitis?
Healthcare providers can improve prevention strategies for Neonatal Gonococcal Conjunctivitis by implementing comprehensive maternal screening for STIs during pregnancy, particularly for Neisseria gonorrhoeae, and ensuring effective treatment protocols are in place that address antimicrobial resistance.
| Key Points | Details |
|---|---|
| Breakthrough Case | Neonatal gonococcal conjunctivitis case in a 12-day-old female infant in Japan due to fluoroquinolone-resistant Neisseria gonorrhoeae. |
| Mixed Infection | Coinfection with Chlamydia trachomatis was also present. |
| Prophylaxis History | Shifts in prophylaxis agents over the years, with issues arising after the discontinuation of erythromycin and the shift to fluoroquinolones. |
| Infection Management | Treatment included immediate prophylactic levofloxacin, admission for intravenous cefotaxime, and eventual treatment with azithromycin after a positive PCR test. |
| Resistance Findings | Resistance to levofloxacin and reduced susceptibility to other antibiotics were identified in the cultured strain. |
| Call for Screening | Emphasis on the need for maternal screening for gonococcal infections to prevent neonatal transmission. |
Summary
Neonatal Gonococcal Conjunctivitis is a significant concern that arises from resistant strains of bacteria, as evidenced by a case in Japan involving a fluoroquinolone-resistant Neisseria gonorrhoeae. This condition highlights the urgent need to reassess current prophylactic measures and maternal screening for sexually transmitted infections during pregnancy. The abandonment of traditional prophylactic agents like erythromycin has led to increased reliance on fluoroquinolones, which may not effectively prevent infections due to emerging resistance. A comprehensive maternal screening strategy is critical to enhance preventive measures and safeguard newborn health against this serious infection.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.