Mycoplasma phocimorsus stands out as a notable zoonotic agent linked to various musculoskeletal infections, including the challenging diagnosis of osteomyelitis. This pathogen often eludes standard cultures, complicating timely treatment and contributing to cases of septic arthritis. In a recent incident involving a hunter who sustained an injury while skinning a bear, initial treatments failed to confirm the infection, which could have benefited from doxycycline treatment upon exposure to a potential source. Given its zoonotic nature, awareness of Mycoplasma phocimorsus is crucial for clinicians dealing with patients post-exposure to seals, bears, or cats. Enhanced vigilance is essential, as early intervention could mitigate the risk of serious complications stemming from these infections.
Infectious agents like Mycoplasma phocimorsus represent a group of pathogens that can transition from animals to humans, leading to significant health issues such as osteomyelitis and septic arthritis. These organisms are often implicated in musculoskeletal disorders, making them a critical concern for medical professionals, especially when treating individuals who have experienced animal-related injuries. The potential for misdiagnosis due to their elusive nature under standard culture methods highlights the need for clinicians to consider alternative treatments, such as doxycycline or moxifloxacin, particularly after exposure incidents. Thus, understanding these zoonotic infections is vital for timely intervention and effective patient outcomes.
Understanding Mycoplasma phocimorsus and Its Zoonotic Implications
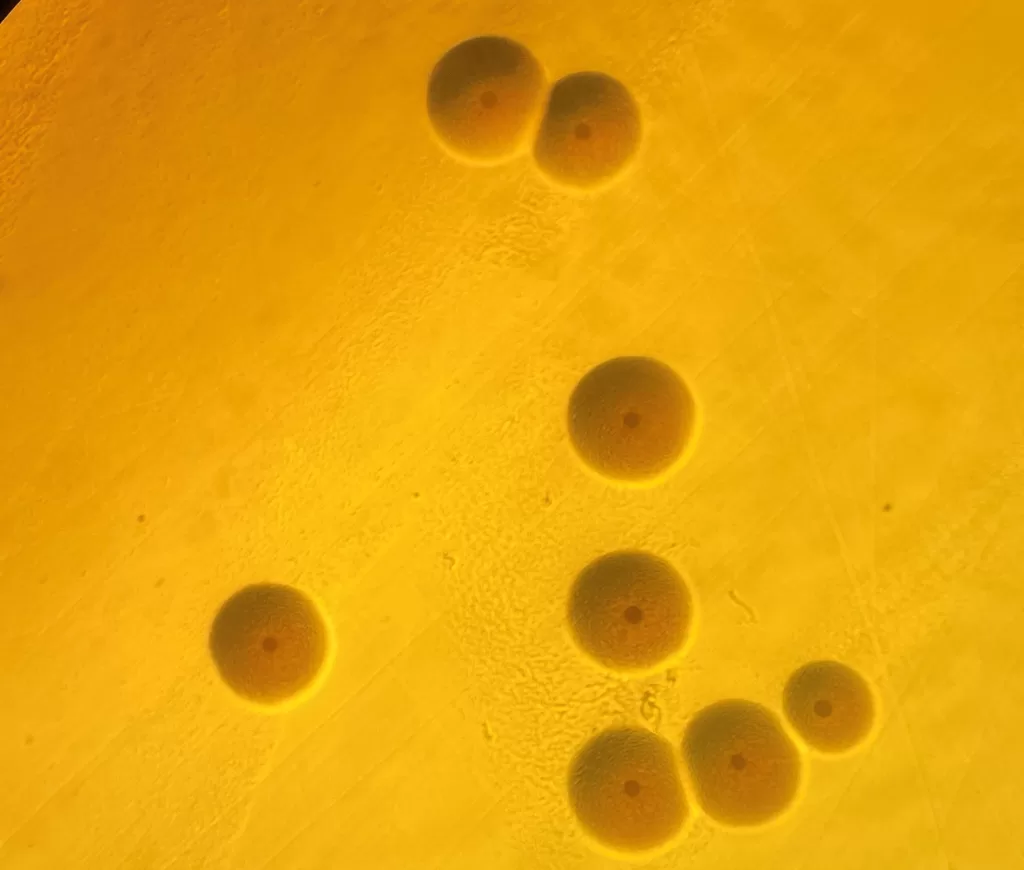
Mycoplasma phocimorsus is increasingly recognized as a pathogenic agent in zoonotic infections, particularly associated with exposure to marine mammals such as seals and bears. This bacterium presents unique challenges in clinical diagnosis and treatment due to its lack of a cell wall, making it resistant to several commonly used antibiotics. Infection often arises from direct contact with these animals, where injuries during handling can lead to the introduction of the pathogen into human tissue, resulting in musculoskeletal infections like septic arthritis and osteomyelitis.
As healthcare providers encounter more cases linked to wildlife exposure, understanding the clinical manifestations and treatment options for Mycoplasma phocimorsus infections becomes critical. Healthcare professionals should maintain a high index of suspicion for this pathogen among patients with a history of animal-related injuries. Early empirical treatment with effective antibiotics, such as doxycycline, is paramount to prevent severe outcomes and complications associated with these zoonotic infections.
Zoonotic Infections from Animal Encounters
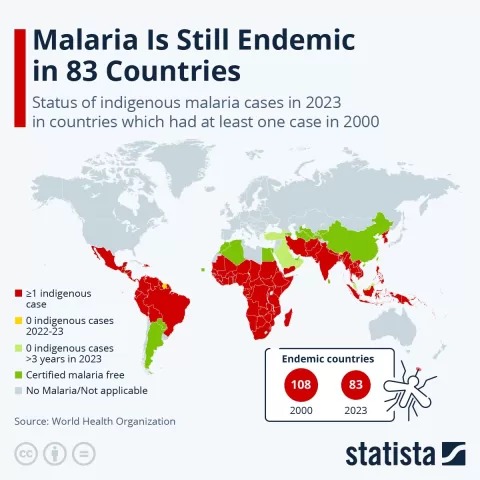
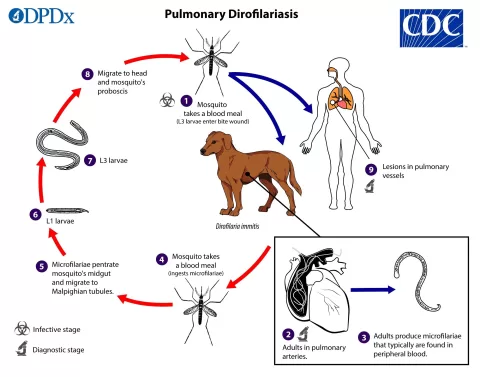
Zoonotic infections continue to rise globally, mainly due to increased human-wildlife interactions. Not only do these infections pose significant health risks, but they also highlight the importance of preventive measures when engaging with potentially zoonotic species. Patients injured by wild animals—whether through hunting, fishing, or recreational activities—should be educated about the risks of infections like Mycoplasma phocimorsus, particularly if they encounter seals, bears, or other marine mammals during these activities.
In cases of potential zoonotic exposure, clinicians should act promptly in assessing the risk for infections, and effective initial treatments must be administered without delay. This not only reduces the chances of severe illness but also helps to limit the spread of such infections to the broader community. Proper wound care, timely antibiotic administration, and thorough patient education can contribute significantly to mitigating the impact of zoonotic diseases.
Osteomyelitis and Septic Arthritis: The Impact of Mycoplasma Infections
Osteomyelitis and septic arthritis are serious conditions that can severely impact the musculoskeletal system, often stemming from infections like those caused by Mycoplasma phocimorsus. Cases, such as the one involving a hunter who suffered a finger injury while skinning a bear, demonstrate the hidden dangers associated with zoonotic pathogens. Such infections can sometimes be masked by initial treatments, leading to delayed diagnoses that allow conditions to worsen, necessitating surgical interventions and more aggressive treatment regimens.
Septic arthritis, particularly following exposure to zoonotic pathogens, can pose long-term challenges for patients, from pain management to potential loss of function. Recognizing the signs early—redness, swelling, fever—is crucial for effective management. Based on the case discussed, interdisciplinary approaches involving infectious disease specialists and orthopedic surgeons can optimize patient outcomes and reduce the risks of chronic sequelae following septic arthritis or osteomyelitis.
Effective Treatment Strategies for Mycoplasma phocimorsus Infections
Treatment of Mycoplasma phocimorsus infections primarily hinges on antibiotic therapy, with doxycycline being one of the preferred choices due to its efficacy against this pathogen. In cases where traditional cultures fail to identify the organism, healthcare providers must rely on molecular diagnostics as part of their treatment approach. This can be critical for guiding therapy and ensuring prompt treatment, especially in patients who have been recently exposed to relevant animals.
Additionally, the treatment regimen may need adjustments based on individual patient responses, which can vary significantly. If patients do not respond as expected to initial interventions, healthcare professionals might consider alternative antibiotics such as moxifloxacin, as highlighted in clinical guidance. The case of the hunter underscores how multi-faceted approaches can aid in efficiently managing infections caused by challenging zoonotic pathogens.
The Role of Doxycycline in Zoonotic Infection Management
Doxycycline remains a cornerstone of treatment for various zoonotic infections, including those caused by Mycoplasma phocimorsus. This tetracycline antibiotic is particularly advantageous due to its broad-spectrum coverage and ability to penetrate tissues effectively. In animal-related injuries, where the risk of Mycoplasma exposure exists, early initiation of doxycycline can provide a crucial window for preventing severe complications such as septic arthritis and osteomyelitis.
Clinical experience demonstrates that doxycycline is not only effective but also generally well-tolerated, making it an ideal choice for patients with musculoskeletal infections. Dosing strategies must be tailored to individual patient needs, as seen in the discussed case where prolonged treatment yielded significant improvements. Increased awareness and timely treatment based on doxycycline can enhance patient recovery and decrease long-term morbidity associated with zoonotic infections.
Understanding Musculoskeletal Infections: Key Considerations
Musculoskeletal infections represent a complex area of medical practice, particularly when influenced by zoonotic pathogens such as Mycoplasma phocimorsus. Clarity in understanding the pathways for these infections can guide clinicians in timely diagnosis and effective management. Symptoms of musculoskeletal infections can often overlap with non-infectious conditions, posing challenges in accurate assessments. Consequently, retaining a broad differential diagnosis when evaluating patients with orthopedic complaints is vital.
Correct clinical reasoning alongside advanced imaging techniques and lab investigations can significantly reduce the duration of undiagnosed infections. Knowledge of the patient’s exposure history provides essential insight and should factored into decision-making. With the rise of zoonotic infections, it becomes increasingly important for healthcare providers to stay informed about the potential risks and treatment options available.
Emerging Challenges in Diagnosing Zoonotic Infections
The diagnostic process for zoonotic infections such as those caused by Mycoplasma phocimorsus is fraught with challenges. Traditional culturing methods may not always identify these atypical pathogens, thus complicating the clinical presentation and potentially leading to delays in appropriate treatment. The case discussed illustrates how rapid diagnostic techniques, like broad-range PCR, can confirm the presence of difficult-to-cultivate organisms, providing clarity that guides therapeutic decisions.
These emerging diagnostic tools are critical, especially in light of expanding interactions between humans and wildlife. Given the complexity of zoonotic disease presentations, clinicians should adopt a proactive approach by utilizing advanced microbiological techniques coupled with thorough patient histories. Such an approach fosters a better understanding of the pathogen landscape, allowing healthcare providers to respond swiftly to zoonotic threats.
Preventive Measures Against Zoonotic Infections While Hunting
Preventing zoonotic infections requires a combination of education and preparedness for those who interact with wildlife, particularly hunters. Understanding the risks associated with skinning and processing animals is paramount, as injuries during these activities can introduce pathogens like Mycoplasma phocimorsus into the human body. Proper handling techniques, including the use of gloves and immediate wound care, are critical strategies that can limit exposure and transmission.
Moreover, awareness of the signs and symptoms of zoonotic infections can lead to quicker responses in case of injury, thereby reducing the risk of severe health complications. Hunters should also be encouraged to seek medical advice proactively after an animal encounter, especially if there are any wounds or signs of infection. Education campaigns tailored to at-risk populations can contribute significantly to reducing incidents of zoonotic infections.
The Importance of Raising Awareness Among Clinicians
Raising awareness among healthcare providers about Mycoplasma phocimorsus and other zoonotic infections is vital in the pursuit of timely and effective patient care. Given the specific animal exposures that can lead to these infections, skills in patient history-taking must emphasize recent wildlife encounters. Such proactive approaches may result in faster diagnosis and treatment regimens, reducing the likelihood of severe complications associated with untreated infections.
Continuing medical education should incorporate case studies highlighting zoonotic infections and strategies for early identification. By equipping clinicians with updated knowledge on zoonotic diseases, they can maintain a vigilant approach in recognizing potential cases and implementing appropriate treatment measures promptly. This is especially critical in regions with high interaction levels between humans and wildlife, thereby improving overall public health outcomes.
Frequently Asked Questions
What is Mycoplasma phocimorsus and how is it related to zoonotic infections?
Mycoplasma phocimorsus is a recognized zoonotic pathogen primarily linked to musculoskeletal infections in humans. It can be transmitted during encounters with infected animals, such as seals and bears, leading to complications like osteomyelitis and septic arthritis.
How does Mycoplasma phocimorsus cause osteomyelitis?
Mycoplasma phocimorsus can lead to osteomyelitis when a person sustains an injury while handling infected animals, resulting in the pathogen entering the bloodstream or local tissue, which then prompts an inflammatory response that may go unnoticed initially.
What are the treatment options for Mycoplasma phocimorsus infections?
Doxycycline is commonly recommended as a treatment option for Mycoplasma phocimorsus infections, especially for osteomyelitis and septic arthritis resulting from zoonotic exposure. Moxifloxacin may also be considered for resistant cases while awaiting molecular diagnostic results.
Can Mycoplasma phocimorsus lead to septic arthritis?
Yes, Mycoplasma phocimorsus can lead to septic arthritis, particularly when there is a significant injury or exposure to infected animals. It can cause inflammation and infection in joints, often requiring surgical intervention for proper diagnosis and treatment.
Why is doxycycline effective for treating Mycoplasma phocimorsus?
Doxycycline is effective against Mycoplasma phocimorsus due to its broad-spectrum activity against various bacteria, including atypical pathogens. It helps control the infection in musculoskeletal infections and improves recovery outcomes in infected patients.
What steps should clinicians take when they suspect Mycoplasma phocimorsus infection?
Clinicians should maintain a high suspicion for Mycoplasma phocimorsus infection in patients with relevant animal exposure, especially after injuries. Prompt initiation of empirical treatment, including doxycycline, is critical while awaiting confirmatory diagnostic testing.
How can Mycoplasma phocimorsus be diagnosed in cases of musculoskeletal infections?
Diagnosis of Mycoplasma phocimorsus in musculoskeletal infections can be challenging. Traditional cultures may fail to identify the pathogen; however, advanced molecular methods such as broad-range 16S rDNA PCR can confirm its presence.
What animal exposures are most commonly associated with Mycoplasma phocimorsus infections?
Mycoplasma phocimorsus infections are most commonly associated with exposures to seals, cats, and bears. These zoonotic connections highlight the risks of handling these animals or being in close contact with them.
| Key Point | Details |
|---|---|
| Zoonotic Agent | Mycoplasma phocimorsus is recognized as a zoonotic agent, highlighting its potential to infect humans. |
| Incident Description | A 29-year-old hunter injured his finger while skinning a bear, leading to complications. |
| Initial Treatment | Initial treatments included trimethoprim/sulfamethoxazole and mupirocin, which were ineffective. |
| Complications | The patient developed fever, tachycardia, and significant swelling, requiring hospital admission. |
| Diagnosis Challenges | Repeated cultures failed to identify the pathogen, delaying diagnosis. |
| Confirmation | 16S rDNA PCR confirmed Mycoplasma phocimorsus after conventional cultures failed. |
| Treatment Regimen | The patient was treated with doxycycline for 42 days, leading to improvement. |
| Clinical Recommendations | Clinicians should consider doxycycline or moxifloxacin for similar cases after relevant exposure. |
Summary
Mycoplasma phocimorsus is an important zoonotic pathogen that can lead to severe musculoskeletal infections. The case of a 29-year-old hunter highlights the challenges in diagnosing this infection, especially following specific animal encounters. Effective treatment options such as doxycycline should be considered promptly to address these infections, emphasizing the significance of awareness and rapid intervention in similar cases.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.