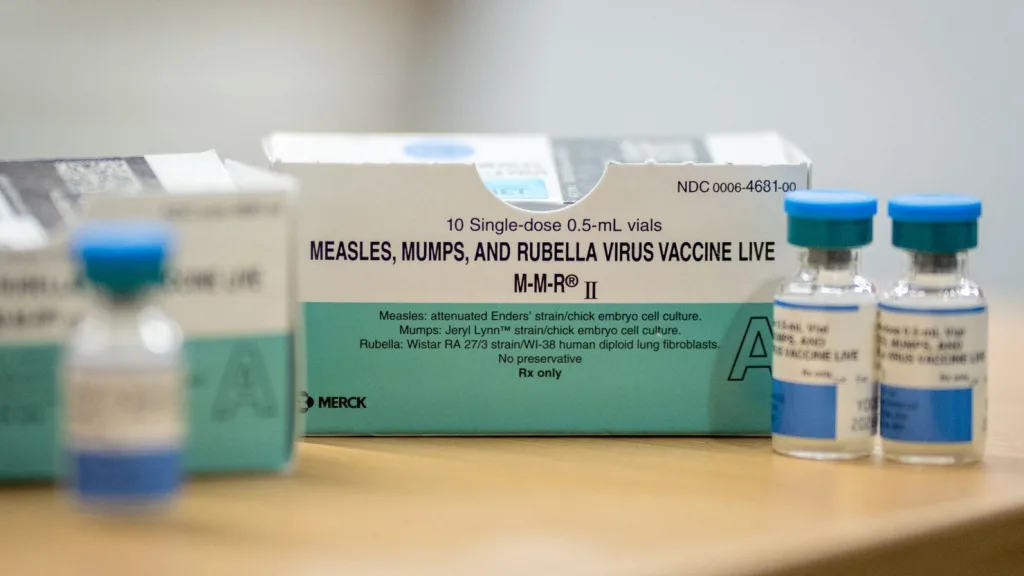
The measles vaccine is a crucial tool in preventing outbreaks of this highly infectious disease, yet recent data reveals troubling trends in vaccine coverage. In central Ohio, a region dramatically affected by a measles outbreak in late 2022, the rates of MMR vaccination remain significantly below the 93% threshold required for herd immunity. Despite increased awareness of the risks posed by measles, especially among vulnerable populations, the uptake of measles, mumps, and rubella vaccinations has not improved substantially since the outbreak. This situation underscores the importance of pediatric vaccination initiatives aimed at reassuring parents and communities about the safety and efficacy of the measles vaccine. With the ongoing challenges around vaccine coverage, it is imperative to address the barriers to vaccination that continue to leave children at risk of preventable diseases like measles.
The immunization against measles, often delivered as part of the MMR shot, plays a vital role in safeguarding public health. Unfortunately, discussions surrounding vaccine efficacy and community health are often overshadowed by rising rates of measles outbreaks across states. Recent statistics demonstrate that many children, particularly in certain demographic groups, are falling behind on their vaccinations, highlighting a public health crisis that demands immediate attention. As health advocates push for improved vaccine compliance within communities, the concept of herd immunity has never been more relevant, emphasizing the collective responsibility of individuals to protect their neighbors, especially in light of recent events. Addressing these challenges not only requires robust public education about vaccinations but also targeted strategies to enhance protective measures in high-risk areas.
The Importance of the Measles Vaccine in Public Health
The measles vaccine is a critical component of public health initiatives globally. By effectively preventing measles, a highly contagious viral disease, the vaccine plays a vital role in reducing the incidence of outbreaks and supporting community health. Vaccination not only protects individuals but also contributes to herd immunity. When the majority of a population is vaccinated, it creates a buffer that protects those who cannot be vaccinated—such as infants or those with certain medical conditions—thereby minimizing the spread of the disease.
The World Health Organization (WHO) has emphasized that achieving a minimum vaccination coverage of 93% is essential to maintain herd immunity against measles. Unfortunately, as observed in recent outbreaks, including the one in central Ohio, vaccine coverage can fall short, putting communities at risk. The continuous propagation of misinformation and vaccine hesitancy tends to exacerbate these issues, underlining the need for education and widespread outreach to underscore the vaccine’s significance.
Current Measles Vaccine Coverage and Trends
Recent studies reveal concerning trends in measles vaccine coverage, despite the heightened awareness following outbreaks. In central Ohio, for instance, measles, mumps, and rubella (MMR) vaccination rates for children have remained low, significantly under the herd immunity threshold. This is alarming, considering that even after an outbreak event, many parents did not increase their child’s vaccination uptake, which is crucial in preventing future emergencies. The statistics show that a substantial portion of children still lacks essential vaccine doses, leaving communities vulnerable.
The analysis of data from a large primary care network in central Ohio highlighted that timely MMR1 vaccinations did not change significantly over time. This indicates a persistent public health challenge, necessitating greater emphasis on pediatric vaccinations. Moreover, engagement with communities—particularly those disproportionately impacted, such as the Somali community—could facilitate improved vaccination coverage and combat misinformation surrounding the measles vaccine.
Strategies to Improve Vaccine Coverage in Underimmunized Communities
To effectively increase measles vaccine coverage, particularly in underimmunized communities, targeted strategies are essential. One approach involves community outreach programs designed to address specific barriers influencing vaccination rates. These barriers can be structural, cultural, or related to misinformation surrounding the measles vaccine. By engaging with community leaders and providing culturally relevant educational materials, these programs can foster trust and dispel fears regarding vaccination.
Additionally, improving access to vaccine administration through conveniently placed clinics, offering flexible hours, and integrating vaccination into pre-existing healthcare appointments can enhance compliance. Schools also serve as pivotal venues for vaccination campaigns—leveraging school-entry requirements can encourage parents to vaccinate their children promptly, thus positively impacting overall vaccination rates and contributing to herd immunity.
Understanding the Implications of Low Vaccine Coverage
The implications of low measles vaccine coverage extend beyond individual health risks. When vaccination rates dip below the herd immunity threshold, populations become susceptible to outbreaks, leading to a resurgence of preventable diseases like measles. In Ohio, the persistence of low MMR vaccination coverage poses a significant risk to community health, particularly for vulnerable groups. Children who have not received timely vaccinations are more likely to experience severe complications from measles, leading to unnecessary hospitalizations and, in extreme cases, fatalities.
Furthermore, low vaccine coverage can strain health resources and put additional pressure on healthcare systems already grappling with rising cases of vaccine-preventable diseases. Proactive measures must be taken to reverse these trends; otherwise, communities could face the real threat of systemic outbreaks similar to those seen in recent history.”}]} ,{
The Role of Herd Immunity in Combating Measles Outbreaks
Herd immunity plays a crucial role in preventing the spread of infectious diseases, especially measles. When a significant percentage of the population is immunized against measles, it creates an environment where the disease cannot easily circulate, protecting those who cannot be vaccinated. To effectively achieve herd immunity against measles, vaccination rates must meet or exceed the 93% threshold, as recommended by health experts. This is particularly important in the wake of outbreaks, as seen in central Ohio, where vaccination coverage failed to improve despite the alarming rise in cases.
The failure to reach the herd immunity threshold can lead to increased outbreaks, especially in highly interconnected communities. With measles being highly contagious, public health strategies must focus on raising awareness about the importance of the measles vaccine and ensuring that all community members, especially those in high-risk groups, are sufficiently protected. Health authorities should prioritize initiatives that not only aim to increase MMR vaccination rates but also instill a culture of vaccination in communities that have previously been hesitant.
Cultural and Structural Barriers to Measles Vaccination
Cultural and structural barriers significantly affect measles vaccination rates, particularly in specific community demographics. Studies have indicated that misinformation, language barriers, and lack of trust in medical systems contribute to lower vaccination uptakes. In areas such as central Ohio, engaging with minority populations, such as the Somali community, is vital to overcoming these barriers. Community leaders and healthcare practitioners must work collaboratively to ensure that reputable information regarding the benefits and safety of the measles vaccine is widely circulated.
Additionally, structural barriers, such as access to healthcare services and financial constraints, can hinder timely vaccinations. Ensuring that vaccinations are readily available and accessible to all populations is essential. Initiatives that provide free or low-cost vaccinations, mobile clinics, and partnerships with local organizations can bridge gaps in access and enable families to vaccinate their children promptly.
The Impact of Community Awareness on Vaccination Uptake
Community awareness plays a significant role in influencing vaccination rates, particularly for the measles vaccine. Following outbreaks, awareness campaigns aim to educate the public about the importance of vaccinations and the implications of low vaccine coverage. However, data from Ohio reveals that despite increased awareness, MMR vaccination rates remained stagnant, indicating a need for more targeted and effective communication strategies. Engaging the community through trusted local figures can enhance the credibility of the information distributed.
Moreover, public health campaigns should focus on dispelling myths surrounding vaccines, highlighting their safety and efficacy. Providing clear and transparent communication about vaccination schedules, potential side effects, and the dire consequences of measles can encourage parents to take proactive steps towards vaccinating their children. Active community engagement can cultivate a culture that champions immunization as vital to public health, thereby increasing overall uptake of the measles vaccine.
The Future of Pediatric Vaccination in Ohio
The future of pediatric vaccination in Ohio is contingent upon addressing the barriers currently preventing adequate MMR vaccine coverage. The data suggests that unless proactive measures are taken, we risk a continuous cycle of outbreaks and declining public health, particularly affecting children. Future strategies must prioritize increasing awareness and accessibility while tailoring interventions to meet the unique needs of diverse communities, including marginalized groups.
In conclusion, a collaborative approach involving healthcare professionals, community leaders, and families will be essential to improve vaccination rates and bolster herd immunity. Continuous monitoring and evaluation of vaccination strategies will be vital to ensure the effectiveness of these initiatives, ultimately working towards a healthier future for the pediatric population in Ohio.
Frequently Asked Questions
What is the importance of the measles vaccine in preventing outbreaks?
The measles vaccine, particularly the MMR vaccination, is crucial in preventing outbreaks as it helps achieve herd immunity. A vaccination coverage of at least 93% is necessary to protect the wider community, especially vulnerable populations who cannot be vaccinated.
How does the measles vaccine impact herd immunity?
The measles vaccine significantly contributes to herd immunity by reducing the overall transmission of the virus. High vaccine coverage rates, achieved through MMR vaccinations, protect those who cannot be vaccinated and help prevent potential outbreaks.
Why has measles vaccine coverage remained low in central Ohio post-outbreak?
Despite a measles outbreak in central Ohio, measles vaccine coverage remains low, with rates not reaching the necessary herd immunity threshold. Factors such as cultural barriers and misinformation may contribute to the limited uptake of the MMR vaccination in the community.
What gaps exist in pediatric vaccination rates for the measles vaccine?
The study indicated significant gaps in pediatric vaccination rates for the measles vaccine, especially among Somali children. Timely MMR vaccination rates were notably lower compared to non-Somali children, revealing disparities that need to be addressed to improve overall vaccine coverage.
How does the measles vaccination rate affect future outbreak risks?
Low measles vaccination rates increase the risk of future outbreaks. The sustained low coverage in central Ohio highlights the vulnerability of the pediatric population, emphasizing the need for increased efforts to raise MMR vaccination rates to ensure community protection.
What are the recommendations for improving measles vaccine coverage?
To improve measles vaccine coverage, targeted outreach and education focusing on the importance of the MMR vaccination are essential. Addressing structural and cultural barriers can help enhance awareness and increase vaccination compliance within the community.
How does the measles outbreak in central Ohio reflect national vaccination trends?
The measles outbreak in central Ohio mirrors national trends of declining vaccine coverage. With increasing cases of measles in underimmunized areas, it underscores the urgent need for improved vaccination strategies, particularly for the MMR vaccination.
What role do catch-up vaccinations play in measles vaccine rates?
Catch-up vaccinations are critical in improving measles vaccine rates, especially for MMR2. These vaccinations help bridge gaps for children who missed earlier doses, ensuring they meet the requirements for school-entry and reducing outbreak risks.
Why is early administration of the measles vaccine vital?
Early administration of the measles vaccine is vital because it ensures timely protection for children against severe complications from measles. This is particularly important in preventing outbreaks and maintaining high vaccine coverage within communities.
What can communities do to support measles vaccine uptake?
Communities can support measles vaccine uptake by providing accessible vaccination clinics, fostering partnerships with local health organizations, and disseminating accurate information regarding the MMR vaccination benefits to counter misinformation.
| Key Point | Detail |
|---|---|
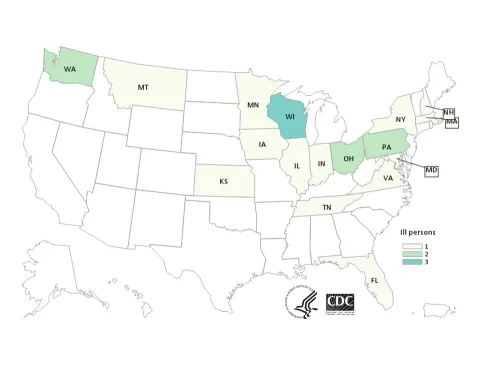
| Measles Outbreak in Central Ohio | An outbreak began in October 2022 with 90 cases, predominantly among children under 15, particularly affecting the Somali community. |
| MMR Vaccine Coverage | 12 and 20 months post-outbreak, MMR coverage remained below the 93% herd immunity threshold. |
| Study Population | 149,092 children from a primary care network, with 8.6% being of Somali descent. |
| MMR1 Vaccination Rates | Remained stagnant at 53.6% over the study period, showing no improvement. |
| MMR2 Vaccination Rates | Increased from 57.9% to 60.2% over 20 months, indicating some improvement. |
| Disparity in Vaccination Rates | Significant gap in timely MMR1 between Somali (35.7%) and non-Somali children (55.4%). |
| Lower Coverage Risks | Vaccination rates remain significantly below the 93% needed for herd immunity, posing risks for future outbreaks. |
| Call to Action | Urgent need for proactive surveillance and outreach, especially in underimmunized communities. |
Summary
The measles vaccine is crucial for preventing outbreaks, as highlighted by the recent situation in central Ohio where coverage remains low. Despite an outbreak and heightened awareness, MMR vaccination rates did not increase significantly, staying below the necessary threshold for herd immunity. This emphasizes the need for targeted outreach and proactive measures to ensure all children, especially in vulnerable communities, receive their vaccinations timely to prevent future measles outbreaks.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.