Maternal syphilis is a significant public health concern that poses serious risks during pregnancy and childbirth. Recent studies have shown that children exposed to maternal syphilis are not only at risk for congenital syphilis, but also have a higher likelihood of hospitalization and longer medical stays compared to their unexposed peers. The impact of syphilis exposure can lead to severe pregnancy complications and adverse birth outcomes, including stillbirth and low birth weight. As hospitalization rates for children with a maternal syphilis background continue to rise, the need for vigilance in monitoring these children becomes paramount. Understanding the risks associated with childbirth and syphilis is essential for improving maternal and child health outcomes and reducing the incidence of these troubling infections.
Maternal syphilis, often referred to as mother-to-child transmission of syphilis, can have dire consequences for both mothers and their infants. The condition encompasses a range of issues including congenital syphilis, which significantly increases the likelihood of medical intervention during early childhood. These syphilis-related complications can manifest as serious health concerns, leading to increased hospitalization rates among affected children. Properly addressing pregnancy complications linked to maternal syphilis is crucial for ensuring healthier births and reducing the long-term impacts of syphilis exposure. Recognizing these threats is vital for healthcare providers working to protect families and improve overall health outcomes.
Understanding Maternal Syphilis and Its Impact
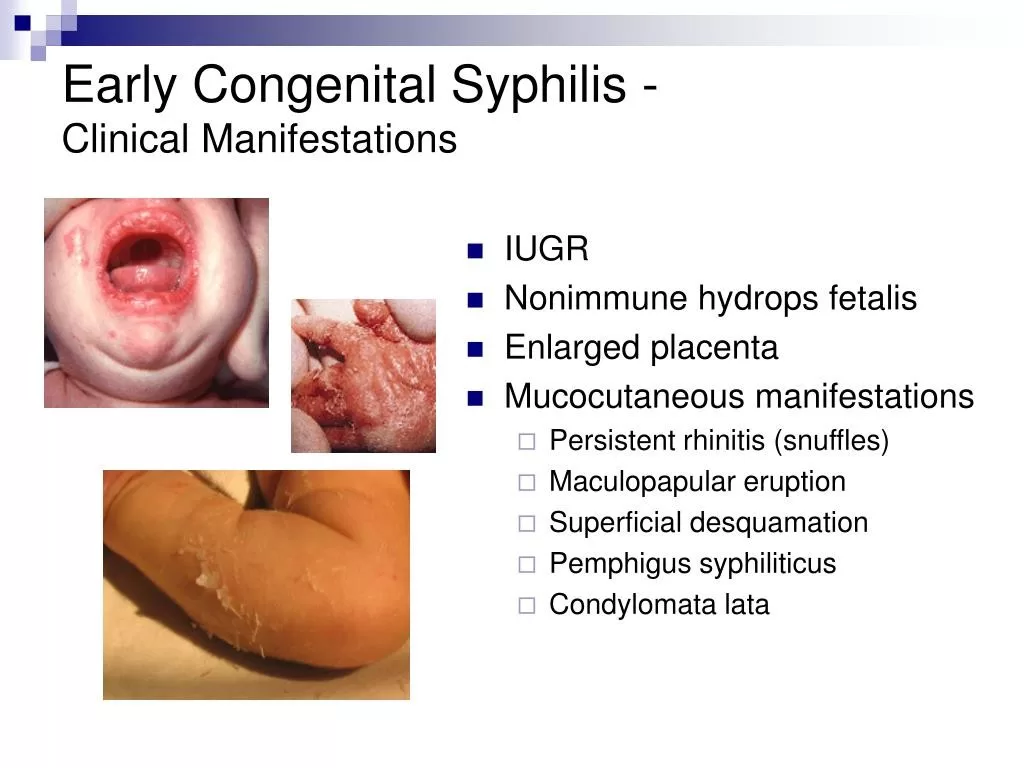
Maternal syphilis is a critical public health issue that significantly affects prenatal and postnatal outcomes. When a mother contracts syphilis during pregnancy, the disease can be transmitted to the fetus, leading to severe complications such as congenital syphilis. This condition is characterized by various serious health issues in newborns, including developmental delays, low birth weight, and even stillbirth. Research has shown that mothers with untreated syphilis face a risk of transmitting the infection, which can result in dire congenital complications for their children.
The rise in maternal syphilis cases is alarming, particularly in high-income countries, where the incidence has surged over 200% in recent years. This trend underscores the importance of early diagnosis and treatment for pregnant women. Addressing maternal syphilis not only protects the mother’s health but also significantly reduces the risks associated with childbirth syphilis. Awareness campaigns and routine screening during pregnancy can play instrumental roles in combating this growing public health crisis.
Congenital Syphilis: Risks and Hospitalization Rates
Congenital syphilis poses substantial health risks to infants and has been closely linked to increased hospitalization rates. In the study conducted by researchers at the London School of Hygiene and Tropical Medicine, it was reported that children with congenital syphilis had a staggering six times greater risk of hospitalization compared to their unexposed peers. The heightened risk highlights the vulnerabilities faced by these infants, necessitating vigilant monitoring and healthcare interventions for those diagnosed with this infection after birth.
Additionally, the exposure to maternal syphilis has been associated with prolonged hospital stays and increased likelihood of various health complications. Approximately 65.1% of children born with congenital syphilis were admitted at least once during their early years, underscoring the urgency for healthcare providers to implement comprehensive care strategies for affected children. Early identification of congenital syphilis can lead to timely treatments, ultimately curbing the adverse health outcomes that may follow.
Pregnancy Complications Related to Syphilis
The relationship between syphilis and various pregnancy complications cannot be overstated. Maternal syphilis increases the risk of serious adverse outcomes, including preterm birth, low birth weight, and neonatal deaths. These complications arise from the infection’s impact on fetal development and maternal health, complicating the pregnancy and delivery process. Therefore, pregnant women with syphilis require enhanced medical supervision and intervention to minimize potential risks.
Preventive measures, such as routine screening and timely treatment for syphilis during pregnancy, are critical in reducing the incidence of these complications. Ensuring that pregnant women have access to appropriate healthcare services can drastically lower the incidence rates of adverse pregnancy outcomes related to syphilis. Public health initiatives must continue to focus on education, prevention, and treatment options for maternal syphilis to safeguard both mothers and their unborn children.
The Rising Trend of Syphilis Exposure in Pregnant Women
Recent studies indicate a concerning rise in syphilis exposure among pregnant women, emphasizing the need for heightened awareness and preventive strategies. Factors contributing to this increase include inadequate access to healthcare, lack of education about the disease, and insufficient prenatal care. As women of childbearing age become more exposed to syphilis, the risk of complications during pregnancy escalates, adversely affecting both maternal and fetal health.
Preventing syphilis exposure in pregnancy is paramount in curbing potential risks associated with childbirth and infant health outcomes. Comprehensive education programs targeting reproductive health can empower women to seek early prenatal care and STI screening. By fostering a broad understanding of the implications of maternal syphilis, healthcare providers can better position themselves to manage and reduce the prevalence among pregnant populations.
Childbirth Risks Associated with Maternal and Congenital Syphilis
Childbirth risks associated with maternal and congenital syphilis are significant, as these infections can lead to severe consequences for both mother and child. During labor, complications such as stillbirth, premature delivery, and dissemination of the syphilis infection to the newborn can occur. Thus, it is essential for healthcare providers to screen for maternal syphilis during pregnancy, to inform delivery room practices, and to implement effective interventions post-delivery.
Moreover, children born with congenital syphilis are often at higher risk not just at birth, but also during their early years, requiring increased hospitalizations. The study referenced highlights that immediate postnatal care and continuous monitoring of these infants are crucial steps in reducing risks. This need for comprehensive care systems suggests that the healthcare infrastructure must adapt to address the complexities associated with childbirth risks linked to maternal syphilis.
Long-Term Healthcare Needs for Children Exposed to Syphilis
Children exposed to maternal syphilis and subsequently diagnosed with congenital syphilis require long-term healthcare considerations. The impacts of congenital syphilis can extend beyond the neonatal period, necessitating ongoing developmental evaluations and interventions. These children may face cognitive or physical challenges necessitating a multi-disciplinary approach to their healthcare that can adapt over time as their needs evolve.
Furthermore, healthcare providers must be proactive in creating tailored care plans that address the distinct needs of these children. By establishing robust support systems that guide families through diagnosis, treatment options, and rehabilitation services, healthcare professionals can significantly improve long-term health outcomes for children affected by maternal syphilis.
Preventing Maternal Syphilis: Strategies and Importance
The prevention of maternal syphilis is essential in tackling the associated risks and health complications for both mothers and their children. Effective strategies involve implementing routine screenings during prenatal visits, ensuring that all pregnant women have access to necessary testing and treatment. Educating women about the implications of syphilis, its transmission, and the importance of early detection is crucial in reducing the incidence of maternal syphilis.
Moreover, public health campaigns focusing on the significance of safe sex practices and STI awareness can empower women to take proactive steps in safeguarding their health. By fostering a culture of transparency and education around maternal syphilis, communities can help to diminish the stigma associated with STIs, thereby encouraging women to seek the care they need during pregnancy.
The Role of Healthcare Providers in Managing Maternal Syphilis
Healthcare providers play a vital role in managing maternal syphilis and mitigating its effects on pregnancy outcomes. They are responsible for ensuring that pregnant patients undergo routine STI screenings and receive timely treatment if diagnosed with syphilis. In addition, healthcare professionals must be equipped with the necessary knowledge to address both the medical and emotional needs of women facing a diagnosis of maternal syphilis.
Furthermore, by creating supportive environments, healthcare providers can foster open discussions with expectant mothers, thereby increasing the likelihood of early intervention. Continuous education for healthcare staff about the latest research and treatment protocols for syphilis can help in improving patient care and ultimately reducing the incidence of congenital syphilis.
Policy Implications and Future Directions in Syphilis Management
The rising rates of maternal syphilis call for urgent policy implications that focus on enhancing testing and treatment protocols. National health organizations must prioritize the development and dissemination of guidelines that ensure prenatal care includes comprehensive STI screenings, education, and accessibility to treatment. Establishing clear frameworks for managing maternal syphilis will enable healthcare systems to provide better outcomes for mothers and their children.
Future directions in the management of syphilis must also address the social determinants contributing to the rise in maternal infections. By tackling issues such as healthcare accessibility, education disparities, and stigma associated with STIs, policymakers can create comprehensive strategies aimed at preventing maternal syphilis and improving maternal and child health outcomes globally. These initiatives will require collaboration among public health authorities, healthcare providers, and community organizations to ensure effective implementation.
Frequently Asked Questions
What is maternal syphilis and how does it affect pregnancy?
Maternal syphilis refers to a syphilis infection contracted by a pregnant woman, which can lead to severe pregnancy complications. If untreated, maternal syphilis can result in adverse outcomes such as stillbirth, preterm birth, low birth weight, and congenital syphilis in the infant. Preventing maternal syphilis is crucial for ensuring both the mother’s health and the healthy development of the fetus.
What are the risks of congenital syphilis in newborns?
Congenital syphilis occurs when syphilis is transmitted from the mother to her baby during pregnancy. Newborns with congenital syphilis face significant health risks, including higher hospitalization rates and long-term developmental issues. According to recent studies, children exposed to maternal syphilis and diagnosed with congenital syphilis are at six times greater risk of hospitalization compared to unexposed children.
How common is hospitalization among children exposed to maternal syphilis?
Children exposed to maternal syphilis are more likely to be hospitalized than those who were not exposed. Research has shown that 65.1% of children with congenital syphilis and 31.3% with maternal syphilis were hospitalized at least once. This highlights the importance of monitoring children born to mothers with syphilis to address any health complications early.
What are the long-term health implications of maternal syphilis for children?
Children exposed to maternal syphilis are at risk for long-term health issues, including prolonged hospitalization and potential developmental delays. The first month of life carries the highest risk for these children, indicating the necessity for ongoing medical care and monitoring. Early intervention is crucial to mitigate the risks associated with congenital syphilis.
What steps can be taken to prevent maternal syphilis during pregnancy?
Preventing maternal syphilis involves routine screening and treatment for syphilis in women of childbearing age, ensuring that they receive appropriate care and education about sexually transmitted infections (STIs). Access to healthcare and prenatal care is also essential to reduce the risks of pregnancy complications related to maternal syphilis.
What is the impact of maternal syphilis on the healthcare system?
The rise in maternal syphilis notably increases healthcare costs due to higher hospitalization rates among affected children. With children exposed to maternal syphilis facing longer hospital stays and frequent medical interventions, addressing this public health issue is critical to reduce the burden on the healthcare system. Effective prevention strategies can diminish the long-term health impacts and associated costs.
| Key Point | Details |
|---|---|
| Study Overview | Conducted in Brazil, involving data from 8.3 million births between 2011 and 2015. |
| Findings on Hospitalization | 65.1% of children with congenital syphilis were hospitalized, compared to 31.3% with maternal syphilis and 19.0% unexposed. |
| Relative Risks | Children with congenital syphilis had a 6-fold risk (HR 6.19); those with maternal syphilis had nearly double the risk (HR 1.90) for hospitalization. |
| Critical Monitoring | The highest risk of hospitalization was during the first month of life for congenital cases (HR 11.53). Children remained at higher hospitalization rates until 36 months. |
| Importance of Prevention | Highlights the need for close monitoring of children exposed to syphilis and the importance of syphilis prevention in pregnant women. |
Summary
Maternal syphilis significantly increases the risk of hospitalization for infants exposed in utero. A recent study revealed that children with maternal syphilis or congenital syphilis are more likely to require medical care, emphasizing the critical need for early detection and prevention strategies. Given the rising incidence of maternal syphilis, it is vital to prioritize maternal health and implement effective syphilis screening and treatment protocols to protect both mothers and their children.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.