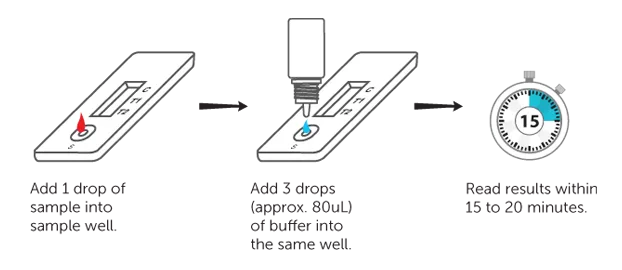
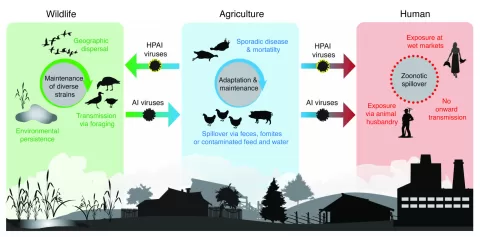
Malaria rapid diagnostic tests (RDTs) are revolutionizing fever management and malaria testing in Africa, particularly among vulnerable children under five. With the distribution of over 3.5 billion RDTs from 2010 to 2021, there has been a notable shift towards accurate malaria testing, improving patient outcomes in sub-Saharan countries where malaria remains a leading cause of mortality. Research indicates that these rapid tests not only enhance the targeting of antimalarial medications but also significantly influence antibiotic use among pediatric patients. This rise in malaria rapid diagnostic tests has prompted an urgent call for comprehensive strategies in fever management, especially given the complexities of antibiotic use in the face of prevailing infection patterns. As we explore the implications of RDTs for fever management in children, it is crucial to balance their benefits in malaria diagnosis with careful consideration of antibiotic stewardship to minimize potential risks.
The advent of rapid malaria testing tools has ushered in a new era for pediatric healthcare, especially in regions plagued by high rates of malaria. These diagnostic innovations facilitate timely identification of malaria and other febrile illnesses, which is essential for effective fever management in children. Not only do they improve access to essential antimalarial treatments, but they also raise questions about the rising trend of antibiotic prescriptions linked to enhanced testing capabilities. The interplay between malaria RDTs and pediatric healthcare provision exemplifies the need for integrated care solutions that address both malaria and non-malaria fever symptoms. In addressing these complexities, healthcare providers can optimize treatment paths that prioritize patient safety and efficacy.
The Role of Malaria Rapid Diagnostic Tests in Fever Management
Malaria rapid diagnostic tests (RDTs) have transformed the landscape of fever management, particularly in sub-Saharan Africa, where malaria remains a leading cause of morbidity and mortality among children. By providing quick and accurate diagnoses, these tests enable healthcare providers to differentiate between malaria and other causes of febrile illness. As reported in various studies, the widespread distribution of malaria RDTs has led to an increase in targeted treatment for malaria, subsequently aiding in better fever management among affected children.
The rise in malaria RDT use also correlates with a notable increase in blood testing rates, which in turn influences treatment protocols. Given that a considerable proportion of childhood fevers is nonspecific and could be due to viral infections, more refined diagnostic capabilities allow healthcare professionals to navigate the complexities of pediatric fever management effectively. However, the challenge remains to interpret these RDT results within the broader context of febrile illnesses, ensuring that treatment decisions align with the underlying causes, be it malaria or another illness.
Impact of Malaria RDT Distribution on Antimicrobial Use
The distribution of malaria RDTs across sub-Saharan Africa has notably affected the landscape of antibiotic use in pediatric treatment. The increase in effective malaria diagnostics has led to a modest rise in the usage of antimalarial medications, but it has simultaneously prompted a concerning rise in antibiotic prescriptions. As healthcare providers gain access to rapid testing results, they may resort to prescribing antibiotics more frequently, perceiving them as a safeguard against concomitant bacterial infections, even in cases where viral pathogens are responsible for febrile symptoms.
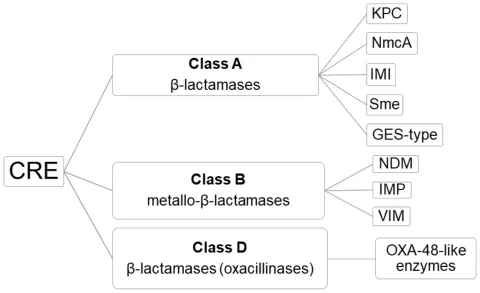
This shift towards antibiotics raises significant concerns regarding the management of fever in children. Increased antibiotic use can foster resistance, complicating the treatment of future infections. The correlation between rising antibiotic prescriptions and the availability of malaria RDTs underscores the necessity for a balanced approach to fever management that does not inadvertently contribute to antibiotic misuse. There is an urgent need for developing comprehensive treatment guidelines that integrate the insights gained from malaria RDTs while ensuring prudent antibiotic stewardship.
Sub-Saharan Africa: A Focus on Pediatric Malaria Control
Sub-Saharan Africa is at the forefront of the battle against malaria, particularly concerning the health of children under five. With the region accounting for 82% of the global malaria burden, effective strategies are imperative for reducing morbidity and mortality rates among this vulnerable population. The deployment of malaria RDTs represents a crucial advancement in the fight against malaria, allowing health workers to confirm diagnoses accurately before initiating treatment.
Despite the progress made through the utilization of these diagnostic tests, challenges remain in ensuring that all febrile illnesses are appropriately managed. While malaria RDTs enhance the capability to diagnose and treat malaria, they must be integrated into a broader healthcare framework that emphasizes holistic fever management. This includes identifying other potential causes of fever that may require different treatment approaches, such as the increasing debates on antibiotic reliance amidst viral infections in children.
Challenges in Pediatric Fever Management
Managing fevers in children encompasses numerous challenges, particularly in regions with high disease prevalence. In sub-Saharan Africa, healthcare providers confront the dual task of tackling malaria while recognizing the reality that many febrile illnesses are viral. The reliance on malaria RDTs should not eclipse the need for vigilance regarding other potential causes of fever, including respiratory and gastrointestinal illnesses.
The complexity involved in pediatric fever management highlights the importance of establishing clear clinical algorithms and point-of-care tests that differentiate malaria from other febrile illnesses. These tools can help in guiding appropriate treatments while minimizing unnecessary referrals to antibiotics, especially given the implications of antibiotic resistance. The push for refined diagnostic tools must also consider the educational component for healthcare providers, ensuring that they are equipped to navigate this challenging landscape effectively.
Antibiotic Use in Children: Trends and Considerations
The rising trend of antibiotic prescriptions among children, particularly in setting where rapid malaria testing is prevalent, poses significant public health concerns. Prescribing antibiotics for non-bacterial infections, a practice that may be inadvertently encouraged by the availability of rapid diagnostic tests for malaria, can lead to unintended consequences, such as antibiotic resistance. In Africa, where infectious diseases are prevalent, this could exacerbate health issues rather than alleviate them.
To counteract these trends, healthcare systems must adopt a comprehensive approach that prioritizes accurate diagnoses and thoughtful treatment plans. Health professionals must be educated about the distinctions between malaria and other febrile illnesses to avoid unnecessary antibiotic courses. Establishing guidelines that embrace the utility of rapid diagnostic tests while advocating for judicious antibiotic use is essential for improving outcomes in pediatric care and preserving the effectiveness of antibiotics.
The Importance of Holistic Fever Management Strategies
In light of the complexities surrounding febrile illnesses in young children, holistic fever management strategies are essential for ensuring that they receive the appropriate care and treatment. While malaria RDTs serve as a critical tool in confirming malaria diagnoses, a broader approach is necessary to tackle the spectrum of illnesses presenting with fever symptoms. This means developing integrated care pathways that consider the full range of potential diagnoses rather than focusing solely on malaria.
Implementing comprehensive fever management plans can lead to improved patient outcomes and reduced complications associated with misdiagnosis. By integrating RDTs into a multi-faceted diagnostic strategy, healthcare providers can appropriately identify and treat conditions that may contribute to pediatric fever, ultimately fostering better health in children across sub-Saharan Africa.
Future Directions for Malaria Testing in Africa
Looking ahead, the future of malaria testing in Africa hinges on innovation and the pursuit of improved diagnostic methodologies. Advancements in point-of-care testing technologies can enhance the speed and reliability of diagnosing malaria and other febrile illnesses, supporting better clinical decision-making. The goal is to develop diagnostics that are not only rapid but also able to differentiate between malaria and other prevalent conditions affecting children in these regions.
Further research and investment in malaria RDTs will be crucial to sustaining progress made in fever management. This includes exploring novel biomarkers and technologies that could complement existing RDTs, offering a more comprehensive understanding of pediatric febrile illnesses. As healthcare systems optimize their approaches to malaria control and fever management, a commitment to integrating these advancements into routine practice will be vital.
Educating Healthcare Providers on Test Utilization
Education plays a pivotal role in maximizing the benefits of malaria rapid diagnostic tests and ensuring their proper utilization in pediatric care. Healthcare providers must be equipped with the knowledge and skills to interpret RDT results effectively and make informed treatment decisions. This includes understanding the implications of a positive test result and how to proceed with care in light of other non-malarial causes of fever.
Regular training programs and workshops can reinforce the importance of using malaria RDTs appropriately within the context of holistic fever management. Encouraging collaboration among healthcare professionals allows for the sharing of best practices and the establishment of treatment protocols that prioritize effective patient care while minimizing the excessive use of antibiotics, which can be detrimental in the long term.
Monitoring and Evaluating Malaria Control Measures
Continuous monitoring and evaluation of malaria control measures are essential for assessing the effectiveness of interventions within sub-Saharan Africa. The complexities of managing pediatric fever require robust data collection and analysis to determine the impact of RDT distribution on health outcomes effectively. This includes tracking not only the rates of malaria diagnoses but also the broader implications for antibiotic use and overall child health.
By establishing strong surveillance systems, countries can identify trends and areas for improvement in malaria control strategies. This allows for timely adjustments to policies and practices that govern the management of febrile illnesses in children, ensuring that interventions remain effective and aligned with current health needs. Through pooling data and insights from various stakeholders, it is possible to fortify the fight against malaria and enhance pediatric health outcomes across the region.
Frequently Asked Questions
How do malaria rapid diagnostic tests improve fever management in African children?
Malaria rapid diagnostic tests (RDTs) significantly enhance fever management in African children by providing quick and accurate diagnosis of malaria. This leads to timely and appropriate antimalarial treatment, reducing the reliance on presumptive treatments and allowing for better-targeted medication use. Consequently, children are less likely to receive unnecessary treatments, resulting in improved health outcomes.
What is the relationship between malaria rapid diagnostic tests and antibiotic use in children?
Studies indicate that the increase in malaria rapid diagnostic tests (RDTs) has coincided with a rise in antibiotic use among children with fever in sub-Saharan Africa. While malaria RDTs help clarify fever causes, they have also led to a shift in treatment towards antibiotics, as many febrile illnesses, especially viral infections, are often mismanaged. This situation raises concerns about potential overuse of antibiotics and highlights the need for balanced treatment approaches.
Why are malaria rapid diagnostic tests crucial in sub-Saharan malaria control efforts?
Malaria rapid diagnostic tests (RDTs) are crucial in sub-Saharan malaria control efforts because they allow for accurate, timely diagnoses that can significantly reduce child mortality rates. The extensive distribution of RDTs has improved health outcomes by ensuring that antimalarial treatments are administered based on confirmed cases of malaria, rather than presumptive treatment based solely on fever symptoms.
What evidence supports the use of malaria rapid diagnostic tests in children under five?
Research supports the use of malaria rapid diagnostic tests (RDTs) in children under five by illustrating that increased RDT distribution correlates with better management of fever and lower child mortality rates. For each additional RDT distributed, there was a documented reduction in mortality rates among children, highlighting the importance of accurate malaria testing in improving pediatric health outcomes.
How can health systems better integrate malaria rapid diagnostic tests into pediatric fever management?
Health systems can improve integration of malaria rapid diagnostic tests (RDTs) into pediatric fever management by developing comprehensive guidelines that include RDT results in treatment algorithms for febrile illnesses. This can involve training healthcare workers to interpret test results effectively and implement appropriate treatment protocols that minimize unnecessary antibiotic usage, thereby fostering responsible healthcare practices.
What are the long-term implications of increased antibiotic use linked to malaria rapid diagnostic tests?
The long-term implications of increased antibiotic use linked to malaria rapid diagnostic tests (RDTs) include the potential development of antibiotic resistance, complicating treatment for other common infections. Ensuring judicious use of antibiotics in conjunction with RDTs is vital to prevent resistance while maintaining effective management of fever in children. Continuous monitoring and refinement of treatment approaches are necessary for sustainable healthcare improvements.
| Key Points | Details |
|---|---|
| Objective of Study | To assess the impact of malaria rapid diagnostic tests (RDTs) on fever management and mortality in children under five in sub-Saharan Africa. |
| Malaria RDT Distribution | From 2010 to 2021, 82% of 3.5 billion malaria RDTs sold were distributed in sub-Saharan Africa. |
| Improved Targeted Treatment | Increased use of RDTs leads to better-targeted antimalarial drug usage. |
| Increased Antibiotic Usage | Antibiotic use increased by 0.4 percentage points for each additional RDT distributed, raising concerns about overuse. |
| Reduction in Child Mortality | Each additional RDT distributed was associated with a decrease of 0.34 deaths per 1,000 child-years. |
| Regional Variations | Survival improvements were noted primarily in high malaria prevalence areas; low prevalence areas saw a shift toward antibiotics. |
| Need for Comprehensive Management | The study highlights the need for better management strategies for pediatric febrile illnesses to ensure appropriate antibiotic use. |
| Importance of Integration | Experts stress the importance of integrating malaria RDTs into broader febrile illness management frameworks to mitigate risks. |
Summary
Malaria rapid diagnostic tests have been shown to significantly improve fever management and reduce child mortality rates in sub-Saharan Africa. This advancement is crucial as malaria remains a leading cause of death among children in the region. However, while the use of these tests has led to better-targeted antimalarial treatments, there has been a concerning increase in antibiotic prescriptions, highlighting the need for a balanced approach in treating febrile illnesses. Future strategies should focus on integrating RDT findings into comprehensive care plans to optimize treatment and minimize the risk of antibiotic overuse.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.