Lyme disease testing plays a crucial role in understanding the impact of this tick-borne illness in areas like Wisconsin, where Lyme disease prevalence has drawn significant attention. With an uptick in Lyme disease surveillance, reliable testing methods, including serologic testing for Lyme disease, are indispensable for accurate diagnosis and case reporting. The recent data reveals that a notable percentage of individuals continue to test positive for Lyme disease, influencing public health strategies. By examining Wisconsin health statistics and trends from 2016 to 2019, we can gain insights into patient demographics and testing behaviors. This understanding not only helps in managing the disease but also in adapting preventive measures against potential outbreaks in the affected regions.
When addressing Lyme disease diagnostics, it’s essential to explore the various methods used to assess this prevalent tick-borne illness. In recent years, enhanced Lyme disease testing practices have come to the forefront, particularly in states with reported high incidences like Wisconsin. Understanding the dynamics of serologic evaluations contributes to the broader narrative of Lyme disease management and surveillance. Evaluating previous Lyme disease testing episodes sheds light on patterns of seropositivity which may skew public health metrics. As the conversation around Lyme disease intensifies, refining our approach to testing and surveillance becomes imperative for effective disease control.
Understanding Lyme Disease Surveillance in Wisconsin
In Wisconsin, Lyme disease surveillance plays a crucial role in public health management and informing community awareness. The state has historically reported significant Lyme disease prevalence, particularly in areas with dense tick populations. Health authorities utilize lab data and patient demographics to monitor infection rates, which helps guide prevention strategies. Understanding the dynamics of Lyme disease transmission is essential to address the public health challenges posed by this tick-borne illness.
The findings from the laboratory data between 2016 and 2019 underline the importance of continual surveillance as repeat testing can skew statistics on Lyme disease prevalence. This data suggests that certain demographics, particularly older adults, may have higher rates of seropositivity due to their previous exposures and immune responses. If health statistics do not accurately reflect new infections, it could delay necessary interventions and public health responses to control Lyme disease spread.
The Role of Serologic Testing in Lyme Disease Diagnosis
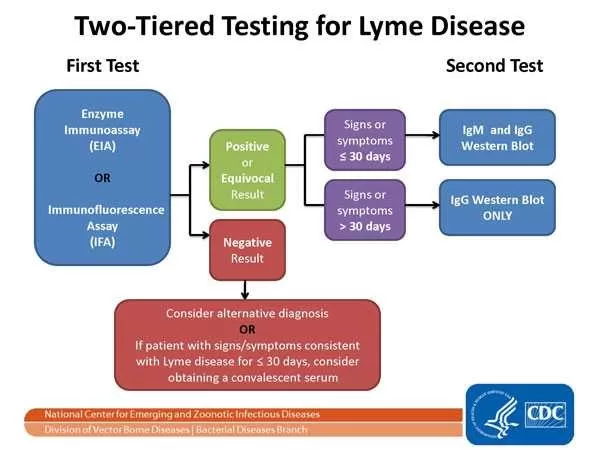
Serologic testing for Lyme disease remains a cornerstone in diagnosing and managing the tick-borne illness caused by *Borrelia burgdorferi*. These tests are conducted using standard two-tier testing (STTT) protocols, which help confirm active infections based on antibody production. The methodology allows healthcare providers to better understand a patient’s exposure history and immune response, influencing treatment decisions. In regions like Wisconsin, where Lyme disease incidence is notably high, serologic testing becomes even more critical.
Despite the reliability of serologic tests, the repeat testing trend observed among certain patients raises concerns over interpreting positive results. For example, individuals with previous Lyme disease infections are more likely to test positive again, not necessarily indicating a new infection but rather a persisted antibody response. This phenomenon underscores the need for interpretive caution and further research to clarify results in the context of Lyme disease epidemiology.
Demographics of Lyme Disease Testing in Wisconsin
The demographics of Lyme disease testing in Wisconsin indicate a disproportionate impact on older adults and females, as identified in the study that analyzed patients between 2016 and 2019. Among the tested population, a significant number of tests were conducted on individuals aged 50-69 years, suggesting that age-related factors may contribute to both heightened risk and testing behavior. Understanding these demographics can inform tailored educational programs and preventive measures targeting at-risk groups.
Moreover, testing patterns revealed that children and males had the highest rates of positive results, particularly during warmer months when outdoor activities increase exposure to tick bites. This highlights the necessity for comprehensive community outreach programs aimed at educating families about tick prevention strategies and the importance of prompt testing following potential exposures. As the prevalence of Lyme disease rises, especially during peak seasons, these efforts could significantly minimize infection rates.
Repeat Testing Patterns and Their Implications
The trend of repeat testing for Lyme disease is noteworthy, especially among individuals with prior positive test results. In the examined data, more than 11% of patients who initially tested negative returned for additional testing within the following year. Among these retests, a striking 95% maintained negative results, yet a few individuals exhibited positive outcomes. This raises questions about the clinical reasoning behind repeat testing and its implications for public health statistics regarding Lyme disease.
From a surveillance standpoint, frequent repeat testing may lead to inflated Lyme disease case reports if not correctly interpreted. This could inadvertently shift focus away from addressing new infections and impact the allocation of resources dedicated to managing Lyme disease at both state and national levels. Public health officials must carefully analyze testing trends and outcomes to optimize response strategies and accurately reflect the true prevalence of Lyme disease within the community.
The Importance of Accurate Lyme Disease Case Reporting
Accurate case reporting of Lyme disease is vital for effective public health responses and resource allocation. As highlighted in this study, a considerable proportion of reported cases appear to stem from older positives rather than indicating new infections. Such discrepancies can result from the persistence of antibodies among individuals who have previously battled the illness, thus complicating the landscape of Lyme disease epidemiology. It is critical for health agencies to adjust their reporting systems to differentiate between new cases and historical positives effectively.
Misinterpretation of Lyme disease data could hinder public health initiatives, such as vaccination trials or awareness campaigns. By emphasizing the importance of precise data collection methods that distinguish repeat positives from new cases, health officials can ensure a more informed approach to tackling Lyme disease. Implementing clearer guidelines will not only enhance Lyme disease surveillance but also improve patient management strategies across Wisconsin.
Strategies for Public Health Education on Lyme Disease
Educating the public about Lyme disease prevention and recognition is key to mitigating its impact, especially in high-incidence areas like Wisconsin. Community outreach initiatives should focus on equipping residents with knowledge about prevention strategies, such as using insect repellent, wearing protective clothing, and performing thorough tick checks after outdoor activities. Increased awareness can empower community members to take proactive measures against tick bites, potentially leading to a decrease in Lyme disease cases.
Additionally, education programs should target at-risk communities, such as outdoor enthusiasts, hikers, and families. By providing tailored resources, including workshops and informational pamphlets, these initiatives can raise awareness regarding the signs and symptoms of Lyme disease and the importance of early testing. Engaging local schools and organizations could also further disseminate crucial information, forming a collective effort to combat the spread of tick-borne illnesses within the state.
The Economic Impact of Lyme Disease on Wisconsin Communities
The economic burden of Lyme disease on Wisconsin communities is significant, impacting healthcare costs as well as productivity loss among affected individuals. With widespread Lyme disease prevalence, healthcare resources are increasingly directed towards diagnosis and treatment, stressing the local health systems. Moreover, individuals suffering from Lyme disease often incur substantial medical bills and may experience diminished work capacity, further straining both household finances and the state’s economy.
Public health funding aimed at Lyme disease prevention and education can be an effective method of mitigating these economic impacts. Investing in prevention campaigns and early intervention strategies not only benefits public health but can also save money in the long run by reducing the overall incidence of the disease. Emphasizing the economic advantages of proactive Lyme disease strategies is essential for securing continued funding and support from local and state government agencies.
Research Needs for Lyme Disease Management
Further research is required to enhance Lyme disease management within Wisconsin and beyond. Understanding the factors contributing to high testing rates alongside low positivity in specific demographics can unveil critical insights for effective interventions. In-depth studies focusing on patient history, tick biology, and environmental changes can provide a comprehensive view of Lyme disease dynamics, paving the way for better public health strategies.
Additionally, exploring the long-term effects of Lyme disease and the persistence of antibodies following infection can inform healthcare practices and guidelines. By prioritizing research in these areas, stakeholders can work collaboratively to develop effective frameworks for monitoring, diagnosing, and treating Lyme disease cases. Advanced studies promoting interdisciplinary approaches will ultimately lead to improved health outcomes and clearer Lyme disease surveillance practices.
Lessons Learned from Lyme Disease Data Analysis
The analysis of Lyme disease testing data from Wisconsin offers valuable lessons for the future of disease monitoring and public health responses. One key takeaway is the critical role of age and demographics in interpreting testing results and understanding epidemiological trends. Recognizing how different populations respond to Lyme disease will help tailor health interventions and resource allocation to best meet community needs.
Another lesson is the necessity for ongoing evaluation and adjustment of surveillance methods to ensure accuracy. As the patterns of Lyme disease evolve, so too must the reporting protocols used by health agencies. Regularly revisiting and refining these methods will be essential to maintain up-to-date statistics and strengthen responses to Lyme disease, thereby safeguarding public health in Wisconsin and other affected regions.
Frequently Asked Questions
What is Lyme disease testing and why is it important for Lyme disease surveillance?
Lyme disease testing involves diagnosing the presence of antibodies against the *Borrelia burgdorferi* bacteria, which causes Lyme disease, a tick-borne illness. Accurate testing is crucial for Lyme disease surveillance, helping health officials track disease prevalence and identify high-risk populations. This data can inform public health responses and preventive measures.
How prevalent is Lyme disease in Wisconsin and how does this affect Lyme disease testing?
Lyme disease prevalence in Wisconsin is notably high, making Lyme disease testing a vital component of local health initiatives. Between 2016 and 2019, high testing rates were recorded in north-central Wisconsin, where understanding the local prevalence helps health authorities manage and respond to tick-borne illnesses effectively.
What types of Lyme disease testing are commonly used for serologic testing?
Common types of Lyme disease testing include standard two-tier testing (STTT), which typically involves an initial enzyme immunoassay followed by a Western blot test if the first is positive. These methods are used for serologic testing to confirm the presence of Lyme disease after potential exposure to tick-borne illnesses.
What are the demographics of patients undergoing Lyme disease testing in Wisconsin?
In Wisconsin, the majority of individuals undergoing Lyme disease testing are aged between 50-69 years old, with a significant proportion being female. Interestingly, positive test results are more frequently seen among children and males, particularly during the summer when tick exposure is highest.
How does repeat testing influence Lyme disease surveillance data?
Repeat testing can significantly affect Lyme disease surveillance data. In Wisconsin, studies indicate that a percentage of individuals tested positive multiple times over the years. This may lead to inflated Lyme disease statistics as repeat positives do not necessarily indicate new infections, particularly in older demographics where antibody persistence is common.
What conclusions can we draw about Lyme disease testing practices based on the findings from 2016 to 2019?
The findings suggest that while Lyme disease testing is crucial for understanding the epidemiology of tick-borne illnesses, discrepancies in positive test results, especially among older adults, require careful interpretation. Public health policies must account for the possibility of repeat positives when evaluating Lyme disease prevalence and implementing disease prevention strategies.
How can understanding Lyme disease testing outcomes improve public health responses in Wisconsin?
By analyzing outcomes from Lyme disease testing, public health officials in Wisconsin can better identify trends in Lyme disease prevalence and develop targeted prevention campaigns. This understanding can lead to more effective communication strategies and resource allocation, ultimately reducing the risk of Lyme disease transmission.
What role does serologic testing play in diagnosing Lyme disease?
Serologic testing plays a fundamental role in diagnosing Lyme disease, as it detects the antibodies produced in response to *Borrelia burgdorferi*. Accurate diagnosis through serologic testing is vital for initiating appropriate treatment and informing Lyme disease surveillance efforts.
| Key Point | Details |
|---|---|
| Study Period | 2016–2019, focusing on north-central Wisconsin. |
| Testing Population | 42,077 standard two-tier testing episodes among 36,984 unique patients. |
| Demographics | 51.5% of tests were on females, highest demographic aged 50-69. |
| Positive Rates | 6.1% tested positive overall, with higher rates in children and males during summer. |
| Repeat Testing | 88.4% had only one testing episode; 11.3% of negatives underwent repeat testing. |
| Implications for Surveillance | Repeating positives may inflate Lyme disease statistics, especially among older adults. |
Summary
Lyme disease testing is essential for understanding the incidence and prevalence of this tick-borne illness. This study highlights critical insights into Lyme disease testing practices in Wisconsin from 2016 to 2019, revealing significant patterns in demographics, positivity rates, and the implications of repeat testing on surveillance data. Recognizing that a considerable fraction of reported cases might stem from repeat positives rather than new infections is crucial for accurate public health reporting and efficient management of Lyme disease.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.