Lyme Disease Diagnosis Disparities pose a significant challenge in understanding how this widespread illness affects different populations. Emerging research highlights that racial and ethnic minorities often experience delays in diagnosis and more severe manifestations of Lyme disease, particularly within Medicaid and Medicare frameworks. This uneven distribution of health outcomes underscores the urgent need for improved diagnostic practices and targeted healthcare strategies. The long-term effects of Lyme disease can be devastating, yet these disparities often hinder access to timely treatment and support for affected individuals, particularly non-White populations. As such, investigating Lyme disease demographics is essential for developing equitable healthcare interventions that address these critical issues.
Exploring the complexities of Lyme disease diagnostic discrepancies reveals broader healthcare inequities that impact various groups disproportionately. Terms such as racial inequities in Lyme disease diagnosis highlight the persistent barriers faced by non-White patients, who are often underrepresented in primary care settings. This phenomenon not only affects immediate healthcare responses but also compounds the long-term effects of Lyme disease, especially among those relying on programs like Medicare and Medicaid. By examining the demographic characteristics of these populations, we can gain valuable insights into the systemic failures that contribute to poorer health outcomes and take informed steps toward advocating for better health equity.
Understanding Lyme Disease Disparities in Medicaid and Medicare
Lyme disease continues to be a growing concern in the United States, particularly among populations reliant on Medicaid and Medicare for healthcare coverage. Recent studies indicate that racial disparities play a considerable role in how Lyme disease is diagnosed and treated. Non-White individuals, especially those from Black and Hispanic communities, are often diagnosed at later stages of the disease due to systemic barriers in the healthcare system. This delayed diagnosis often leads to severe manifestations of Lyme disease, including long-term effects that could be mitigated with timely intervention.
The findings from the retrospective study covering the years 2016 to 2021 reveal a stark contrast in diagnosis rates and healthcare access among different racial groups within Medicaid and Medicare beneficiaries. For instance, older adults over 65 years on Medicare presented the highest incidence rates, but the disparities were evident as non-White patients were more likely to experience hospitalizations and receive diagnoses outside of standard care settings. These differences underscore the urgent need for tailored public health interventions that consider demographics and access to care.
Impact of Lyme Disease on Racial and Ethnic Minorities
The impact of Lyme disease is disproportionately felt among racial and ethnic minorities, particularly when one looks at the data from Medicaid beneficiaries. The study found that non-White populations exhibited a higher prevalence of advanced Lyme disease. These populations often face additional challenges, such as lack of access to preventive care and educational resources regarding Lyme disease symptoms and testing. Consequently, these factors contribute to both a higher incidence and severity of the disease among minorities.
Furthermore, the long-term effects of Lyme disease can significantly impair the quality of life for those affected, particularly in marginalized communities. Chronic Lyme disease symptoms, such as fatigue and joint pain, can lead to a higher burden on healthcare resources and increase the demand for Medicaid services. As such, addressing these disparities through increased funding for education and outreach initiatives is vital for improving health outcomes among these vulnerable populations.
Medicaid and Medicare: Addressing Lyme Disease Incidence Gaps
Medicare and Medicaid are crucial programs that provide necessary healthcare access to millions of Americans, yet studies reveal gaps in service delivery, particularly regarding Lyme disease diagnosis. Data show that there are significant underdiagnoses among minorities, partly due to a lack of training among healthcare providers in recognizing the symptoms of Lyme disease, particularly in demographics that are predominantly non-White. As Lyme disease becomes more prevalent, especially in certain geographical areas, it is essential that these programs improve their outreach and education efforts.
Efforts to bridge these gaps can include enhanced training for healthcare providers within Medicaid and Medicare networks to identify and treat Lyme disease symptoms accurately and promptly. Additionally, incorporating Lyme disease education into community health programs could promote awareness among minority populations. Such initiatives could ensure that beneficiaries understand their risks and have access to testing and treatment options, ultimately improving health outcomes for all.
The Role of Demographics in Lyme Disease Diagnosis
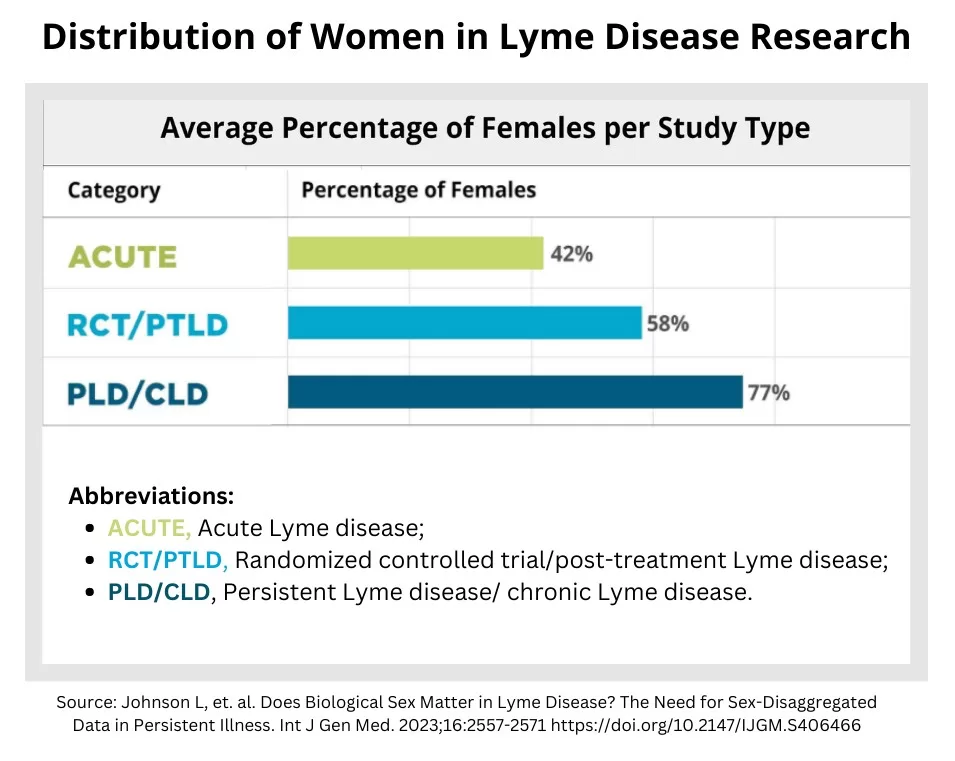
Demographics play a vital role in the diagnosis and treatment of Lyme disease, with significant implications for healthcare systems like Medicaid and Medicare. The data from the 2016-2021 study illustrates how age, gender, and racial factors can influence healthcare access and outcomes for Lyme disease patients. For instance, younger individuals under Medicaid faced more barriers to care, resulting in delayed diagnoses. Similarly, non-White populations were often diagnosed outside the typical peak periods for Lyme disease transmission, further complicating their treatment and recovery.
Addressing these demographic disparities requires a concerted effort to tailor healthcare responses to the needs of various groups. By understanding how demographics influence Lyme disease diagnosis and treatment, public health officials can implement more effective strategies for outreach and education. In particular, targeting interventions toward at-risk groups can enhance early detection and treatment, ultimately reducing the severity of the disease and its long-term effects.
Long-term Effects of Lyme Disease and Health Equity
The long-term effects of Lyme disease can be profound, particularly for those who experience delays in diagnosis and treatment. As the study highlights, non-White populations often face a higher burden of chronic symptoms that can impact daily functioning and overall health. These long-term complications are not merely medical issues; they also pose significant socioeconomic challenges, with individuals potentially facing increased healthcare costs, lost wages, and diminished quality of life.
To address these long-term effects, it is essential to promote health equity in Lyme disease management. Strategies may include improving access to continuous care and follow-up services, ensuring that all patients, regardless of racial or ethnic background, receive adequate support for medical and psychological needs post-diagnosis. Moreover, fostering partnerships between community organizations and healthcare providers can help raise awareness of long-term Lyme disease effects, thus empowering affected individuals to seek early intervention and comprehensive care.
Healthcare Utilization Patterns for Lyme Disease Across Demographics
The patterns of healthcare utilization in Lyme disease cases reveal stark discrepancies among different demographic groups. The study indicates that non-White beneficiaries of Medicare and Medicaid are less likely to seek care in a timely manner for Lyme disease symptoms, often presenting with more severe cases due to earlier misdiagnosis or lack of access to primary care providers. Understanding these patterns helps in analyzing the broader implications for public health systems and highlights the need for targeted interventions.
Furthermore, the differences in healthcare utilization also reflect systemic issues, such as socioeconomic status and geographic access to healthcare facilities. Bridging these gaps is crucial for ensuring that all patients receive proper care, regardless of their demographic background. By addressing these utilization patterns through tailored healthcare policies and outreach programs, Medicare and Medicaid can enhance their effectiveness in treating Lyme disease and reduce health disparities.
The Importance of Education and Prevention in Lyme Disease Management
Education and prevention strategies play a critical role in managing Lyme disease, especially within vulnerable populations served by Medicaid and Medicare. The CDC study emphasizes the need for targeted educational campaigns that address the unique challenges faced by racial and ethnic minorities. These campaigns should inform individuals about Lyme disease transmission, symptoms, and preventive measures, equipping them to seek timely treatment and reduce the likelihood of severe outcomes.
Moreover, preventive measures, including community-based interventions and awareness initiatives, can empower at-risk populations to take proactive steps toward their health. This approach not only enhances individual knowledge but also fosters community engagement to reduce Lyme disease incidences. A comprehensive public health strategy focusing on education and prevention can ultimately lead to improved health outcomes and equity in Lyme disease management.
Exploring Lyme Disease Medicare Coverage and Accessibility
Medicare coverage for Lyme disease reflects the necessity to ensure adequate care for patients experiencing long-term effects of the disease. The data suggests that beneficiaries over 65 years have the highest incidence rates of Lyme disease, yet disparities in access to care persist among various racial groups. Ensuring proper coverage for Lyme disease treatments under Medicare is vital for recovery and managing the disease’s long-term impacts.
The exploration of Medicare accessibility is vital in ensuring that minorities have equal opportunities to receive necessary care for Lyme disease. Strategies to enhance services include streamlining the claims process for Lyme-related treatments and ensuring that educational materials are available in multiple languages to reach diverse populations. By improving accessibility and awareness of Medicare benefits related to Lyme disease, healthcare providers can contribute to reducing health disparities.
Analyzing Lyme Disease Cases Among Minority Groups
Analyzing the data concerning Lyme disease cases among racial and ethnic minorities highlights a critical insight into health disparities in the U.S. The study indicates that non-White individuals experience higher incidence rates and worse outcomes, emphasizing the need for targeted research on the social determinants of health that may contribute to these disparities. Understanding the demographic factors influencing Lyme disease presentations can drive more effective public health strategies.
Additionally, establishing robust tracking mechanisms for Lyme disease cases among minority populations can help healthcare providers and policymakers better allocate resources and develop targeted interventions. Increased focus on these demographic analyses is paramount in creating a fair healthcare system that proactively addresses the unique challenges faced by affected groups. Through ongoing research and vigilant monitoring, the public health community can mitigate the adverse impacts of Lyme disease among minorities.
Frequently Asked Questions
What are the key findings regarding Lyme disease diagnosis disparities among Medicaid and Medicare beneficiaries?
The study highlights significant racial and ethnic disparities in Lyme disease diagnosis among Medicaid and Medicare beneficiaries. Non-White individuals were more frequently hospitalized at diagnosis, diagnosed outside of primary care, and faced diagnoses during non-peak transmission periods compared to White individuals, underscoring a need for targeted healthcare interventions.
How do racial disparities in Lyme disease diagnosis affect treatment outcomes for patients?
Racial disparities in Lyme disease diagnosis can lead to poorer treatment outcomes. Non-White patients, particularly Black/African American beneficiaries, showed a higher prevalence of disseminated Lyme disease, which may result in more severe symptoms and complications if not addressed promptly.
What demographic trends were observed in Lyme disease diagnoses among Medicare and Medicaid populations?
The study revealed that among Medicaid beneficiaries, Lyme disease was more commonly diagnosed in individuals under 18 and over 19 years old, while Medicare recipients over 65 had the highest incidence. These demographics indicate the importance of focused screening and preventive measures tailored to specific age and racial groups.
What roles do Medicare and Medicaid play in addressing Lyme disease diagnosis disparities?
Medicare and Medicaid are crucial in providing healthcare access to vulnerable populations affected by Lyme disease. By analyzing patient data, the study emphasizes the need for improved educational outreach and preventive strategies to address racial disparities in diagnosis and treatment within these programs.
What are the long-term effects of Lyme disease observed in different demographic groups?
Long-term effects of Lyme disease vary significantly across demographic groups. The study indicates that non-White individuals experience more severe and disseminated forms of the disease, which could lead to chronic health issues if left untreated, thereby highlighting the importance of early diagnosis and equitable healthcare access.
How can healthcare practices improve Lyme disease diagnosis among affected demographics?
Healthcare practices can improve Lyme disease diagnosis by enhancing awareness of the disease among healthcare providers, particularly in underserved communities. Implementing routine screenings, encouraging primary care visits, and providing educational resources tailored to racial and ethnic minority groups can help address diagnosis disparities effectively.
What preventive measures are recommended to address Lyme disease diagnosis disparities?
Preventive measures include increasing public awareness about Lyme disease symptoms and transmission among at-risk populations, improving access to healthcare, and ensuring equitable insurance coverage for diagnostic services under Medicare and Medicaid. Additionally, targeted community outreach programs can help educate and empower individuals in minority groups.
What are the implications of the study’s findings on Lyme disease demographics for future research?
The study’s findings underscore the need for future research to focus on understanding the root causes of racial disparities in Lyme disease diagnosis and outcomes. Research should explore barriers to care, healthcare provider biases, and the effectiveness of interventions tailored to mitigate these disparities among different demographic groups.
| Population Group | Cases Identified | Key Findings |
|---|---|---|
| Medicaid Beneficiaries (Under 18) | 33,776 | Higher likelihood of severe disease among non-White individuals. |
| Medicaid Beneficiaries (Over 19) | 30,935 | Increased hospitalization rates for non-White compared to White beneficiaries. |
| Medicare Beneficiaries (Under 65) | 12,911 | Disparities are noted in diagnosis timing and healthcare access. |
| Medicare Beneficiaries (Over 65) | 90,913 | Highest incidence noted, particularly for non-White individuals. |
Summary
Lyme Disease Diagnosis Disparities are a significant concern in the U.S., revealing critical differences in how the disease is diagnosed among diverse racial and ethnic groups. This study highlights that non-White individuals, particularly Black/African American beneficiaries, face more severe implications of Lyme disease, including increased hospitalizations and misdiagnoses. Addressing these disparities is essential to ensure equitable healthcare access and improved outcomes for all individuals affected by Lyme disease.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.