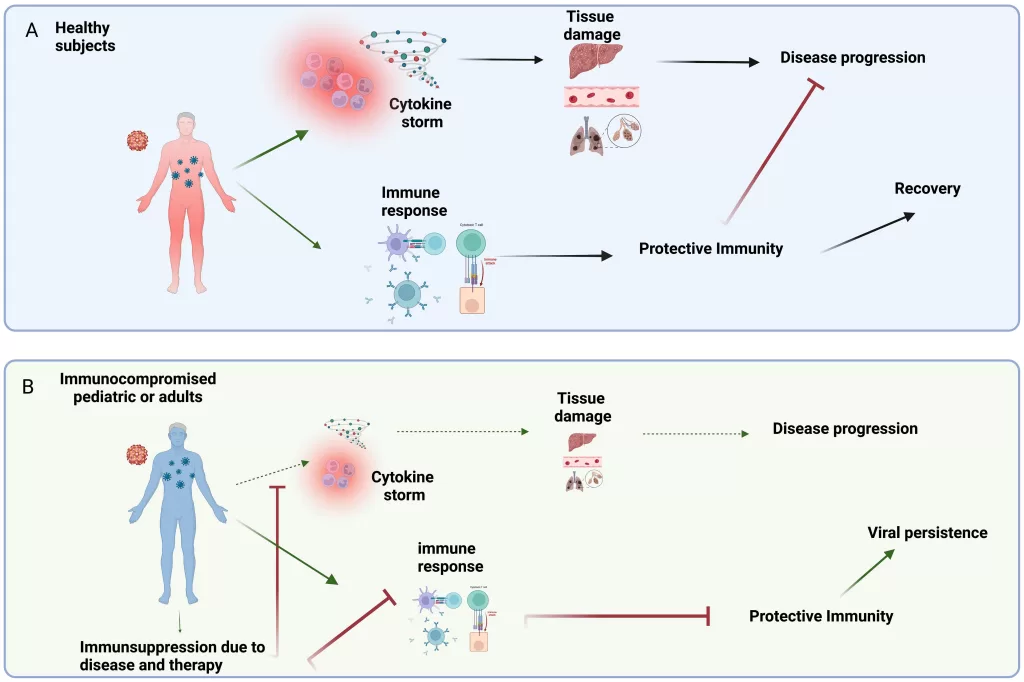
In recent research, the phenomenon known as immunologic study rebound viruses has gained significant attention, particularly in the aftermath of COVID-19. As pandemic health measures like masking and social distancing were lifted, a concerning resurgence of respiratory viruses emerged, impacting both children and adults alike. This study sheds light on how the restrictions not only curtailed COVID-19 spread but also inadvertently diminished immunity to other endemic viruses in young populations. With findings emerging from the NIH’s PREMISE program, researchers have begun to unravel the complex interplay between lifted health protocols and increased viral re-emergence. Understanding the COVID-19 impact on viruses is crucial for devising effective strategies to bolster immunity and manage public health in the post-pandemic landscape, especially as children’s immunity studies continue to highlight significant vulnerabilities within this demographic.
Exploring the aftermath of the COVID-19 pandemic reveals critical insights into the resurgence of various viral infections following the relaxation of public health guidelines. These rebound viruses, including commonly circulated respiratory pathogens, have surged as populations return to pre-pandemic behaviors. The comprehensive immunologic studies conducted have shown that the lack of exposure to these viruses during strict health measures has left many individuals, particularly children, with diminished immune defenses. As researchers analyze these trends, they are uncovering essential data that could inform future pandemic response strategies and promote herd immunity. Adequate understanding of these dynamics is not only vital for public health but also for developing innovative vaccine solutions in light of the ongoing evolution of respiratory viruses.
Understanding the Resurgence of Respiratory Viruses Post-COVID-19 Measures
The lifting of COVID-19 health measures has led to a noticeable increase in respiratory virus infections, particularly among children. With reduced social interactions and stringent masking protocols during the pandemic, many children were inadequately exposed to common respiratory pathogens. This absence of exposure resulted in a significant deficit in their immunity against these viruses. As families began to resume normal activities and restrictions were eased, health officials noted a corresponding resurgence of respiratory diseases, raising concerns about the long-term immunity of children and the potential for increased morbidity due to these infections.
The study conducted under the PREMISE program highlighted data that suggested the immunity gaps in children corresponded directly with their lack of exposure during strict COVID protocols. Researchers analyzed serological data from blood samples to determine immunity levels against 16 different respiratory viruses. The significant rebound of viruses, such as influenza and Respiratory Syncytial Virus (RSV), following the lifting of restrictions underscores the necessity for enhanced public health strategies to monitor and manage these emerging threats, particularly as kids return to schools and social environments.
Immunologic Study on Rebound Viruses: Insights and Implications
The immunologic study detailing the rebound of other viruses provided critical insights into how pandemic health measures have inadvertently affected children’s immunity. According to the findings, many children lacked antibodies for respiratory viruses before the lifting of COVID-19 restrictions. Once normal activities resumed, many of these children experienced a sudden surge in respiratory infections likely due to the previously mentioned lack of exposure. This creates a unique scenario where the collective immunity of a young population is insufficient to handle the rapid influx of viruses, thus affecting overall public health.
Furthermore, the researchers emphasized that the immunologic study’s findings could be pivotal in predicting future viral outbreaks. They noted that the patterns observed could allow public health officials to prepare for potential spikes in infections similar to those recorded with enterovirus D68, which has been linked to acute flaccid myelitis. By understanding these dynamics, health agencies can develop targeted vaccination programs and public health campaigns aimed at bolstering immunity in children, ensuring that they are better equipped to face resurgent respiratory viruses.
The Role of Children Immunity Studies in Future Pandemic Preparedness
Children’s immunity studies play a pivotal role in shaping the future of public health strategies, especially in light of the COVID-19 pandemic. These studies offer valuable data that can help identify immune deficiencies and susceptibility patterns in the pediatric population, which have emerged as key factors during respiratory virus surges. By examining how pandemic health measures have impacted immunity levels in children, researchers can develop tailored interventions to mitigate severe outcomes from respiratory virus infections.
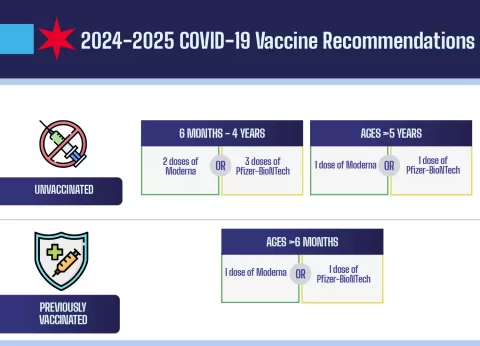
Moreover, the data gathered from ongoing studies, such as the PREMISE program, can guide future vaccine development and health policy decisions. Understanding the effects of public health measures on viral exposure rates is essential for improving epidemic preparedness. As these studies continue to evolve, they may lead to enhanced strategies for monitoring children’s health, increasing vaccine uptake, and ultimately preventing outbreaks of respiratory diseases in the post-pandemic era.
Effects of Pandemic Health Measures on Virus Dynamics
The COVID-19 pandemic dramatically altered the landscape of viral transmission dynamics. The enforcement of health measures such as social distancing, closures, and masking drastically reduced the prevalence of respiratory viruses for an extended period. However, this led to unforeseen consequences: a significant portion of the population, particularly children, emerged with little to no immunity against common respiratory pathogens once these measures were lifted. This reveals a complex interaction between public health strategies and viral ecology.
Research shows that while these measures were essential for curbing the spread of COVID-19, they inadvertently increased the susceptibility of children to other respiratory viruses post-pandemic. As preventive measures were relaxed, the resulting wave of infections illustrates the potential risk of outbreaks as immunity gaps widen. Thus, ongoing studies into the dynamics of these viruses are crucial to inform future health responses and ensure a balanced approach to public health that considers both viral infections and population immunity.
Implications of Immunologic Research for Public Health Policies
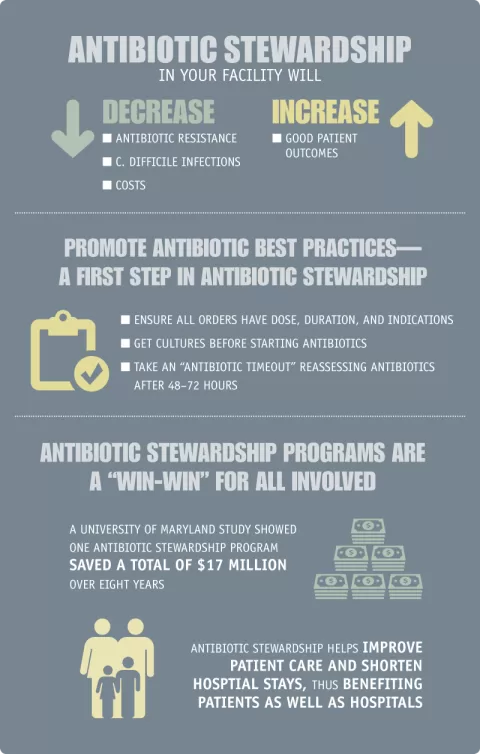
The findings from immunologic research, particularly regarding rebound viruses after the relaxation of COVID-19 restrictions, necessitate a re-evaluation of current public health policies. Understanding how different pathogens interact and influence each other is vital for creating effective response frameworks that can be adapted to emerging threats. Policymakers must consider integrating insights from studies like the PREMISE program into future health guidelines to better prepare for subsequent waves of respiratory viruses.
Moreover, these research findings underscore the need for a collaborative approach in addressing the public health implications of respiratory virus outbreaks. By leveraging insights garnered from children’s immunity studies and other immunologic research, health agencies can develop comprehensive surveillance systems that not only track viral infections but also assess population immunity. This strategic approach will enable health authorities to proactively respond to potential spikes in infections and safeguard community health.
Forecasting Future Respiratory Virus Surges Through Data Analysis
Data analysis has become a cornerstone of predicting respiratory virus surges in the wake of COVID-19. Researchers are now leveraging insights from serological studies to develop accurate models that forecast potential outbreaks based on immunity data. By identifying trends and patterns in children’s immunity and exposure levels, health officials can strategically prepare for and mitigate the impact of future respiratory virus resurgences. For instance, the recognition of increased levels of viral transmission following the resumption of normal activities highlights the importance of timely data collection and analysis.
Through advanced forecasting models that integrate findings from studies like the PREMISE program, public health experts can anticipate viral trends and implement timely interventions. This proactive approach not only enhances the accuracy of emergency responses but also improves stakeholder and community communications, providing transparency and preparedness as seasons of heightened respiratory activity approach.
Enhancing Predictions of Virus Transmission Dynamics
The insights gained from immunologic studies are pivotal in enhancing predictions of virus transmission dynamics within populations. By understanding the immune landscape among children post-pandemic, researchers are better equipped to model how respiratory viruses may spread under varying conditions. This is particularly important in light of the recent resurgence of conditions such as RSV and influenza, which have historically impacted pediatric populations severely during seasonal outbreaks.
Incorporating serological data into transmission models allows for a more nuanced understanding of how immunity levels fluctuate with changing public health measures. As such, these blended models can help predict not only the spread of respiratory viruses but also the potential severity of outbreaks, enabling more targeted public health interventions and resource allocation.
Need for Continuous Surveillance Post-Pandemic
The dramatic changes in viral dynamics due to the COVID-19 pandemic underscore the necessity for continuous surveillance of respiratory viruses. Ongoing monitoring can provide insights into the re-emergence and spread of viruses among populations, particularly vulnerable groups such as children who may have insufficient immunity. As previous health measures were relaxed, the surveillance showed an uptick in respiratory viruses, emphasizing the urgency of rigorous data collection frameworks to gauge shifts in public health.
By establishing a robust surveillance system that integrates findings from immunologic studies and response data, health agencies can better preempt and respond to emerging viral threats. This proactive stance is crucial in crafting guidelines that inform the public and health professionals alike, highlighting potential risks and necessary actions to protect population health effectively.
The Importance of Multi-Pathogen Studies in Public Health Research
Multi-pathogen studies are increasingly recognized for their role in shaping effective public health responses. This focus on understanding the interactions between various respiratory viruses provides comprehensive insights into not just individual pathogens, but also how they collectively affect population health dynamics. The findings from the immunologic studies conducted during and post-COVID-19 underscore the interconnectedness of respiratory viruses, revealing the need for extensive surveillance and research into overlapping impacts.
As evidenced from the study that monitored children during the pandemic, multi-pathogen research can enhance knowledge of immunity gaps that have developed over time. This knowledge not only aids in crafting more effective medical countermeasures but also helps refine public health strategies that can be tailored to address diverse viral threats comprehensively. The integration of such research into standard public health protocols will be instrumental in developing more resilient health systems capable of managing future epidemics.
Frequently Asked Questions
What does the immunologic study reveal about rebound viruses after COVID-19 measures?
The recent immunologic study highlights that the lifting of COVID-19 pandemic health measures, such as masking and social distancing, has contributed to a resurgence of respiratory viruses. These safeguards initially diminished the circulation of other viruses, leaving many children without adequate immunity. The study, part of the NIH’s PREMISE program, analyzed blood samples from children and found that the removal of these measures correlated with increased immunity and a spike in infections from various endemic respiratory viruses.
How do pandemic health measures affect children’s immunity to respiratory viruses?
Pandemic health measures during COVID-19 significantly impacted children’s exposure to respiratory viruses, resulting in a notable lack of immunity among young children. The study demonstrated that children under the age of 10, monitored over 2022 to 2023, showed reduced exposure to viruses like influenza and RSV due to COVID prevention measures. As these measures eased, a rebound in respiratory diseases was observed, indicating a need for enhanced understanding of children’s immunity in relation to infectious diseases.
What viruses did the immunologic study focus on during the COVID-19 pandemic?
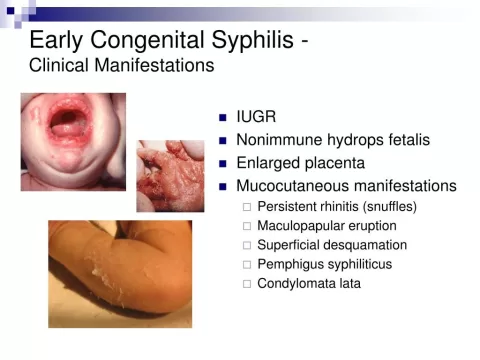
The immunologic study monitored immunity against 16 different endemic respiratory viruses, with a primary focus on enterovirus D68 (EV-D68). Additionally, the research covered other notable viruses such as influenza, respiratory syncytial virus (RSV), parainfluenza virus, metapneumovirus, and rhinovirus. This comprehensive approach helps detail the immune landscape of children in the context of respiratory illnesses post-pandemic.
Why is the PREMISE program significant for future pandemics and respiratory virus monitoring?
The PREMISE program is crucial as it provides in-depth insights into the population dynamics of emerging and re-emerging infections, particularly respiratory viruses. By utilizing data from serological sampling, researchers can better understand immunity and predict future outbreaks. This initiative aids in developing medical countermeasures, like vaccines and antibody treatments, ensuring preparedness against future pandemics based on empirical evidence gathered during this study.
What are the potential implications of respiratory viruses resurgence as indicated by the immunologic study?
The surge in respiratory viruses following the removal of COVID-19 measures suggests significant public health implications. The findings underscore the importance of routine serological surveillance to enhance our understanding of viral dynamics and predict future trends. As children lacked exposure to common respiratory viruses, health agencies may need to reconsider vaccination strategies and public health policies to better protect populations, especially vulnerable groups like children.
How can the findings of the immunologic study inform public health policy?
Findings from the immunologic study provide valuable data for shaping public health policies regarding infectious disease management. By evidencing the effects of pandemic health measures on immunity and the resurgence of respiratory viruses, health officials can create targeted interventions. Policymakers may also consider integrating routine serological testing into existing surveillance systems to better monitor virus transmission and immunity levels, preparing communities for potential future health crises.
| Key Points |
|---|
| The lifting of COVID-19 measures led to increased circulation of respiratory viruses, notably among children. |
| The study monitored 174 children under 10 years across four medical centers for a year to assess immunity levels. |
| 16 different respiratory viruses were screened, revealing low immunity levels in children during the pandemic. |
| After the lifting of COVID measures, immunity levels for respiratory viruses increased, correlating with a rise in infections. |
| Findings can help predict future viral outbreaks, particularly for EV-D68, which can lead to severe illness. |
| The study advocates for improved serological surveillance to better understand and predict virus spread. |
Summary
Immunologic study rebound viruses are emerging as a critical area of focus following the lifting of COVID-19 prevention measures. A recent study highlights how the removal of these restrictions has led to a resurgence of respiratory viruses, particularly impacting children who have built little immunity during the pandemic. By analyzing blood and respiratory samples from young children, researchers found a significant increase in immunity levels aligned with the increased circulation of various pathogens. This study not only sheds light on the dynamics of viral infections post-COVID but also stresses the necessity for ongoing serological surveillance to anticipate and mitigate future outbreaks effectively.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.