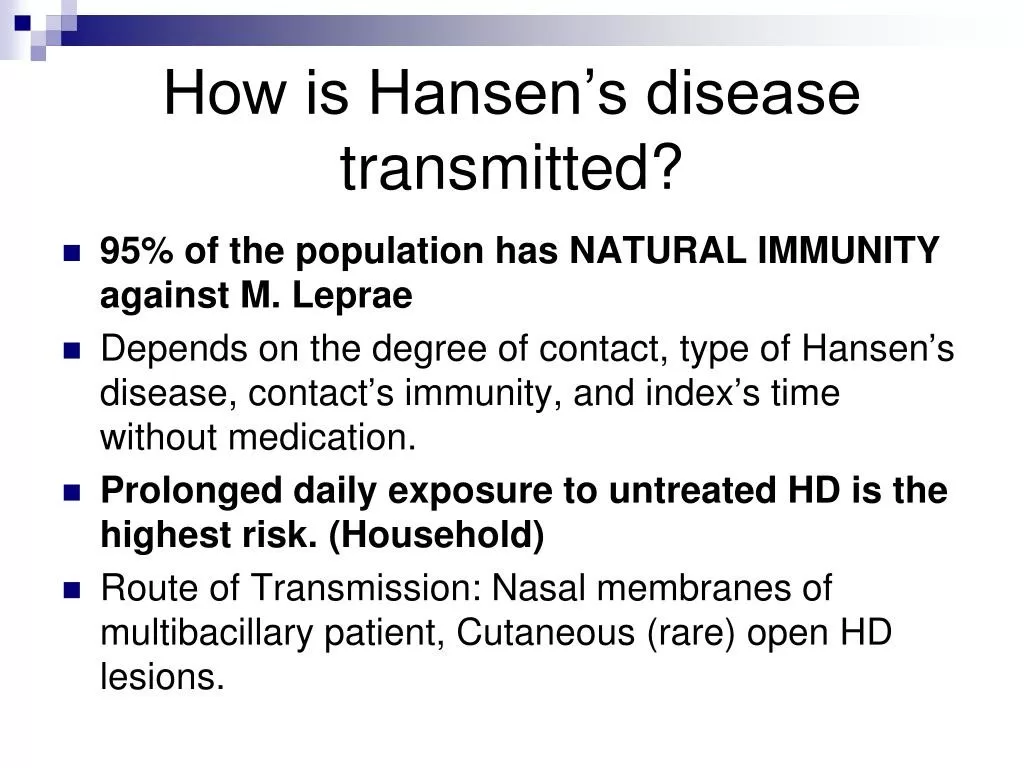
Hansen disease transmission is a vital topic as this condition, commonly known as leprosy, continues to affect hundreds of individuals across the United States each year. Transmitted primarily through prolonged contact with infected individuals or their respiratory droplets, the disease is closely associated with environmental exposures, particularly related to nine-banded armadillos. These unique creatures are considered a primary source of transmission in North America, raising significant public health awareness about leprosy causes and its potential spread. In the context of rising cases, especially in states like Florida and Georgia, understanding Hansen disease symptoms becomes crucial for early detection and treatment. This growing incidence underlines the importance of education and research on scenarios of Hansen disease to mitigate risks and protect at-risk populations.
The transmission of leprosy, scientifically known as Hansen’s disease, has garnered increased attention as its prevalence fluctuates in various regions. This chronic inflammatory condition, caused by the bacteria *Mycobacterium leprae*, can lead to severe nerve damage if not diagnosed early. An often overlooked factor in the spread of leprosy is the environmental contact with certain wildlife, particularly the nine-banded armadillo, which is known to harbor the bacteria. Raising awareness of the symptoms associated with leprosy and the potential risks associated with animal encounters is critical for effective public health interventions. As we explore the epidemiology and environmental factors influencing Hansen disease, we aim to enhance community understanding and promote proactive measures against this ancient ailment.
Understanding Hansen Disease: Causes and Symptoms
Hansen disease, also known as leprosy, is primarily caused by the slow-growing bacterium *Mycobacterium leprae*. This organism primarily affects the skin and peripheral nerves, leading to symptoms such as discolored patches on the skin, numbness, and in severe cases, deformities. While transmission can occur, the risk is relatively low because prolonged contact is often necessary for the disease to spread. Understanding the causes and presentation of Hansen disease is vital in recognizing its clinical manifestations and ensuring timely diagnosis and treatment.
The symptoms of Hansen disease can vary widely among individuals, making it essential to be aware of the different clinical presentations. Some might experience mild skin lesions while others may gradually lose the ability to feel pain or touch in affected areas. Since the bacterium has a long incubation period, sometimes lasting up to 20 years, many individuals might not associate their symptoms with leptospirosis until more significant damage has occurred. Recognizing these symptoms early can lead to effective intervention and management.
Hansen Disease Transmission: The Role of Armadillo Exposure
Recent research highlights that one significant route of Hansen disease transmission is through direct contact with nine-banded armadillos. These animals are recognized as the only known natural reservoir of *M. leprae* in North America, primarily in southern regions like the Gulf states. Studies have shown that individuals who frequently engage in outdoor activities, particularly those that involve handling armadillos or living near their habitats, have a higher likelihood of contracting the disease. This underscores the importance of understanding the ecological dynamics and behaviors of these animals as they relate to human health.
In many scenarios of Hansen disease transmission, the direct physical contact with armadillos plays a crucial role. The findings from various studies indicate that over 70% of patients who contracted the disease had some interaction with armadillos or their bodily fluids. This form of exposure raises awareness on the importance of public health education regarding avoiding armadillo contact and recognizing potential environmental risks. As further research unfolds, exploring the transmission mechanism will help develop effective preventive strategies.
Hansen Disease in the United States: An Overview of Recent Trends
Hansen disease has been diagnosed in roughly 150 to 200 individuals each year in the United States, although the latest statistics signal an upward trend, with 225 cases reported in 2023 alone. This increase in diagnosed cases, particularly in states like Florida and Georgia, suggests that more people are encountering the conditions conducive to the disease’s transmission. Public awareness and understanding of this disease are critical as it moves out of the historical shadows into a context where health officials can better address and manage its effects.
The recent uptick in Hansen disease highlights the importance of localized epidemiological studies that can shed light on potential sources and transmission routes. The prevalence of cases among US-born individuals also suggests a changing landscape that public health officials must address. With specific environmental exposures identified, including those linked to armadillo contact, future public health campaigns can be tailored to inform communities about the risks and necessary precautions to prevent the spread of this historically stigmatized condition.
Environmental Factors Influencing Hansen Disease Incidence
Environmental exposures play a significant role in the transmission and incidence of Hansen disease. Factors such as geographic location, climate, and local wildlife, particularly the nine-banded armadillo, increase the risk of exposure and infection. Studies indicate that specific regions in the southern United States have a higher prevalence of Hansen disease, likely due to the habitat of the armadillos and the human activities in those areas. Understanding these environmental influences is key to controlling the spread of Hansen disease and informing public health decisions.
Moreover, the interactions between human populations and their environment underscore the necessity for comprehensive epidemiological surveillance. Unique landscapes, combined with outdoor lifestyles prevalent in the southeastern United States, facilitate increased armadillo-human contact. Proactively investigating these environmental interactions can lead to targeted interventions, promoting public education and effective preventive measures to reduce the risk of Hansen disease transmission within at-risk communities.
Detecting Hansen Disease: The Importance of Early Diagnosis
Early diagnosis of Hansen disease is crucial for effective treatment and reducing the risk of complications such as nerve damage. The prolonged incubation period of the disease challenges health care providers as symptoms may not be immediately evident. Therefore, raising awareness about the risk factors and symptoms of Hansen disease is vital for early detection. Health care providers must also consider a patient’s environmental exposures—like armadillo contact—when assessing potential Hansen disease cases.
Additionally, educational campaigns targeting both the medical community and the general public can foster better understanding of the disease’s signs and symptoms. Encouraging individuals to seek medical support promptly when experiencing unusual skin lesions or sensory loss could drastically improve outcomes. Timely treatment not only mitigates the individual’s suffering but also helps prevent further transmission of the disease, particularly in areas known for higher incidence rates.
Public Health Implications of Hansen Disease
The rise in Hansen disease cases has significant public health implications that require immediate attention. As infections of *M. leprae* rise, understanding the epidemiological trends can help health officials allocate resources more effectively and implement strategic public health policies. Education regarding the risks associated with armadillo exposure is essential for communities where these animals are prevalent. Public health initiatives could include outreach programs, community engagement, and educational resources targeted toward populations at risk.
Moreover, comprehensive research into the demographics and social aspects surrounding Hansen disease cases can assist in tailoring interventions that meet community needs. By fostering collaboration among public health experts, researchers, and community leaders, state and federal agencies can effectively address the implications of Hansen disease as it re-emerges in North America, ensuring that preventative measures and health resources are accessible and well-informed.
The Path Forward: Future Research Needs in Hansen Disease
The findings on the rising incidence of Hansen disease in specific areas of the United States point to a pressing need for future research. Understanding the dynamics of transmission, the ecological role of the nine-banded armadillo, and environmental conditions that foster the disease’s spread are all vital areas for investigative studies. This research can uncover why certain populations are more susceptible and lead to targeted prevention strategies that could mitigate risks.
Furthermore, interdisciplinary collaborations between environmental scientists, public health officials, and epidemiologists can forge a more holistic approach to Hansen disease research. As we seek to understand the complex interplay between humans, wildlife, and disease, innovative methodologies will be necessary. The integration of epidemiological studies and public health initiatives will be critical in addressing and controlling the transmission of Hansen disease in the years ahead.
Addressing Stigma Surrounding Hansen Disease
Despite advances in understanding Hansen disease, stigma continues to surround the condition, often hindering prevention and treatment efforts. Many individuals associate the disease with its historical connotations and myths, leading to social isolation and discrimination against those diagnosed. Addressing these societal perceptions is crucial to encourage more individuals to seek medical help without fear of stigma.
Public awareness campaigns focused on demystifying Hansen disease and educating communities about its causes, symptoms, and transmission can help combat stigma. Community involvement in these educational programs provides opportunities for those affected to share their experiences, fostering empathy and understanding. Reducing stigma not only helps individuals feel more comfortable seeking care but also encourages open dialogue about Hansen disease at societal levels.
The Role of Community Engagement in Hansen Disease Awareness
Engaging the community plays a vital role in dispersing information about Hansen disease effectively. Local outreach programs can bridge the gap between health officials and at-risk populations, ensuring that accurate information about transmission methods, especially regarding armadillo exposure, reaches those who need it most. Community health workers can facilitate discussions, distribute educational materials, and provide support for individuals who may have been affected by the disease.
Moreover, partnerships with local organizations and stakeholders can enhance the reach of educational initiatives and create a supportive environment for discussions about Hansen disease. By fostering trust within communities, health initiatives can empower individuals to take proactive measures for their health and encourage proactive responses to symptoms. Community involvement is indispensable in creating a culture of awareness and action against Hansen disease transmission.
Frequently Asked Questions
What is the primary mode of Hansen disease transmission in the United States?
Hansen disease, also known as leprosy, is primarily transmitted through prolonged contact with an infected individual. However, the nine-banded armadillo has been identified as a significant source of transmission in the southern United States, particularly for locally acquired cases.
Can you contract Hansen disease from armadillo exposure?
Yes, exposure to the nine-banded armadillo is considered a potential source of Hansen disease transmission. Individuals who come into direct contact with armadillos or their bodily fluids are at higher risk of contracting *Mycobacterium leprae*, the bacteria that causes leprosy.
What are the common symptoms of Hansen disease?
Common symptoms of Hansen disease include skin lesions, numbness, and nerve damage, particularly in the hands and feet. If untreated, Hansen disease can lead to significant health issues over time, making early diagnosis and treatment critical.
How does armadillo exposure relate to local outbreaks of Hansen disease?
Research indicates that local outbreaks of Hansen disease in the United States are often linked to armadillo exposure. Many patients diagnosed with locally acquired Hansen disease report direct contact with armadillos, emphasizing the need for awareness in regions where these animals are prevalent.
What preventative measures can reduce the risk of Hansen disease related to environmental exposures?
To reduce the risk of Hansen disease transmission, especially in areas where armadillos are common, individuals should avoid direct contact with these animals, maintain good hygiene, and report any skin lesions or unusual symptoms to a healthcare professional promptly.
Are there any environmental factors that influence Hansen disease transmission?
Yes, environmental factors, such as proximity to areas inhabited by armadillos and soil conditions where *Mycobacterium leprae* can survive, play a crucial role in the transmission of Hansen disease in certain regions, particularly in the southeastern and Gulf states of the United States.
What should I do if I think I’ve been exposed to Hansen disease?
If you believe you have been exposed to Hansen disease, particularly through contact with armadillos or individuals diagnosed with leprosy, it is important to consult a healthcare provider for evaluation and possible testing to ensure timely diagnosis and treatment.
| Aspect | Details |
|---|---|
| Transmission Sources | Nine-banded armadillos (*Dasypus novemcinctus*) and potentially free-living amoebae in soil. |
| Hansen Disease Overview | Commonly known as leprosy, caused by *Mycobacterium leprae*. |
| Prevalence in the U.S. | Approximately 150–200 cases annually, with a peak of 225 cases in 2023. |
| Local vs. Immigrant Cases | The study included 55 patients: 13 presumed local and 42 immigrants. |
| Outdoor Activities | Frequent outdoor activities and close contact with armadillos identified as key exposure factors. |
| Demographics | Rising incidence noted particularly among US-born patients. |
| Research Need | Further research required to understand the epidemiology and environmental factors of transmission. |
Summary
Hansen disease transmission primarily occurs through contact with nine-banded armadillos, which serve as a key reservoir for the disease in the southern United States. The findings indicate that outdoor activities and armadillo exposure significantly contribute to the risk of acquiring Hansen disease. With increasing case numbers, particularly in regions like Florida, it is crucial to enhance our understanding of the transmission dynamics and advocate for public health measures to mitigate the risks associated with this disease.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.