Gonorrhea vaccination has emerged as a vital component in the fight against sexually transmitted infections (STIs) in the UK, with sexual health clinics gearing up to offer protective measures for high-risk individuals. The National Health Service (NHS) has initiated a program recommending the use of the meningococcal B vaccine specifically for gay and bisexual men who have had numerous sexual partners or bacterial STIs in the past year. This proactive step is crucial as gonorrhea treatment becomes increasingly challenging due to rising antibiotic-resistant strains. With nearly 85,000 reported cases of gonorrhea in 2023—a staggering increase from previous years—this vaccination initiative aims to mitigate further spread. By leveraging existing vaccines, the NHS hopes to bolster STI prevention efforts and ultimately enhance sexual health throughout the country, thereby safeguarding both individual and public health.
In recent months, the conversation surrounding gonorrhea vaccination has gained momentum as public health authorities seek innovative strategies to combat the surge in STIs. The initiative, which aligns with broader sexual wellness efforts in the UK, is particularly focused on protecting vulnerable populations such as sexually active men who engage with multiple partners. The introduction of the meningococcal B vaccine as a preventive measure against Neisseria gonorrhoeae exploits the potential cross-protective properties of existing vaccinations. As health departments emphasize the importance of early intervention and aggressive STI prevention practices, this program marks a notable advance in community health measures. As we delve deeper into the implications and benefits of this vaccination strategy, it’s essential to understand its role within the broader framework of sexual health clinics and national health initiatives.
Understanding Gonorrhea Vaccination
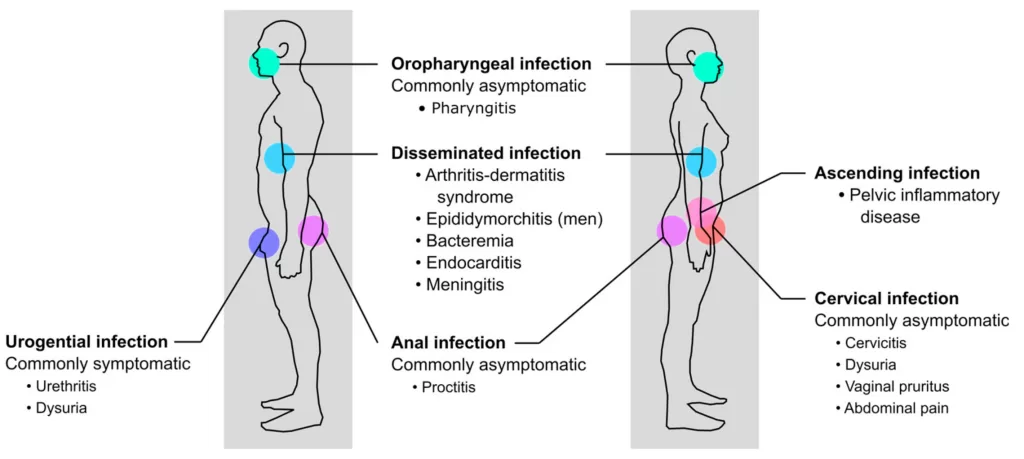
Gonorrhea vaccination is evolving as a crucial component in the fight against sexually transmitted infections (STIs), particularly in high-risk populations. Although a specific vaccine for Neisseria gonorrhoeae has not yet been developed, the 4CMenB vaccine has emerged as a viable alternative. This vaccine is currently recommended by the NHS for gay and bisexual men, especially those who have experienced multiple sexual partners or a bacterial STI in the last year. Through such initiatives, public health agencies aim to mitigate the alarming rise in gonorrhea cases across the United Kingdom, emphasizing the importance of vaccination as part of a comprehensive sexual health strategy.
Additionally, the deployment of the 4CMenB vaccine highlights the integration of existing vaccines into broader STI prevention efforts. Research indicates that this vaccine can provide moderate protection against gonorrhea, evidenced by effectiveness rates of 30% to 40%. By targeting individuals at the highest risk for gonorrhea, the NHS anticipates not only a reduction in infection rates but also significant financial savings for the healthcare system. This innovative approach represents a pivotal step toward enhancing sexual health and reducing the burden of STIs in the UK.
Impact of Gonorrhea on Public Health
The increasing prevalence of gonorrhea in the UK poses a significant public health challenge. In 2023, there were approximately 85,000 reported cases—triple the number from 2012 and the highest recorded since gonorrhea tracking began in 1918. Such alarming statistics underscore the urgent need for effective prevention strategies. As antibiotic resistance continues to rise, controlling the spread of gonorrhea becomes more critical; thus, vaccination could serve as a key tool in curtailing this trend. This proactive stance not only aims to protect individuals but also safeguards the entire community from the repercussions of untreated infections.
Furthermore, initiatives like the NHS gonorrhea vaccination program aim to break the cycle of transmission prevalent in high-risk communities. By focusing on those with higher incidences of STIs, the NHS is not only addressing the immediate health risks but also laying the groundwork for more sustainable sexual health practices. This comprehensive approach, coupled with educational campaigns in sexual health clinics across the UK, seeks to raise awareness about STIs and their prevention, ultimately fostering a healthier society.
The Role of Sexual Health Clinics in STI Prevention
Sexual health clinics in the United Kingdom are pivotal in the efforts to prevent STIs, including gonorrhea. These clinics provide essential services, including testing, treatment, and education regarding sexual health, which are crucial as gonorrhea rates continue to escalate. By offering the 4CMenB vaccine alongside traditional treatments, these clinics expand their role in STI prevention, becoming frontline defenses against the rapidly spreading infections. The integration of vaccination into routine sexual health services illustrates a comprehensive approach to disease prevention.
Moreover, sexual health clinics serve as a safe space for individuals seeking help or information regarding their sexual health. They promote awareness about available treatments and preventative measures, encouraging patients to engage in responsible sexual practices. This holistic model aims to reduce stigma associated with STIs, promoting open conversations about sexual health, and improving overall community well-being. Such clinics form a crucial part of a national strategy that not only targets current infections but also aims to prevent future outbreaks.
NHS Gonorrhea Program: A New Milestone
The NHS gonorrhea program represents a significant milestone in combating the rising rates of this bacterial STI in the UK. Implemented in response to increasing case numbers, particularly among high-risk groups, this program advocates for the use of the meningococcal B vaccine as a means of cross-protection against gonorrhea. This groundbreaking recommendation, emerging from the UK’s Joint Committee on Vaccination and Immunisation, illustrates a proactive stance in managing public health concerns while leveraging existing vaccination frameworks.
In terms of financial implications, the program is expected to yield substantial savings for the NHS, with predictions that it could prevent over 100,000 gonorrhea cases and save the public health system millions over the next decade. By investing in vaccination for vulnerable populations, the NHS not only addresses immediate health concerns but also becomes a pioneer in public health innovation. Such programs highlight the importance of continual adaptation and responsiveness in public health strategies, ensuring that health authorities effectively tackle evolving infection challenges.
Cross-Protection: Meningococcal B Vaccine and Gonorrhea
The relationship between the meningococcal B vaccine and cross-protection against gonorrhea showcases the innovative strategies being explored in STI prevention. Studies indicate that the 4CMenB vaccine, originally formulated to protect against meningitis, also offers moderate protection against gonorrhea, with effectiveness ranging between 30% and 40%. This finding marks a scientific breakthrough, providing a new avenue for protecting vulnerable populations from gonorrhea without the immediate need for a dedicated vaccine.
Exploring cross-protection mechanisms reinforces the critical role of existing vaccines in public health strategies. Utilizing established vaccines to combat the rise of infections such as gonorrhea is a strategic move that not only maximizes the use of available resources but also optimizes patient health outcomes. The adoption of these strategies by sexual health clinics across the UK signifies a dedicated effort towards comprehensive STI prevention, melding science and public health policy for a healthier future.
Challenges in Gonorrhea Treatment and Prevention
Despite advanced treatment options for gonorrhea, challenges remain due to the emergence of antibiotic-resistant strains of the bacteria. As treatment regimens become less effective, the importance of prevention strategies, including vaccination, becomes increasingly evident. The NHS now faces the dual challenge of treating existing infections while innovatively preventing new cases, as antibiotic resistance poses a severe risk to effective gonorrhea management.
Moreover, public perception and awareness of gonorrhea prevention remain significant barriers. Many people still lack understanding about the seriousness of STIs and the need for regular testing and vaccination, which can hinder the effectiveness of STI prevention programs. Enhancing education around the risks associated with gonorrhea and the benefits of vaccination and other preventive measures is crucial not only for personal health but also for community health, significantly reducing the incidence of STIs across the population.
Importance of Education in Gonorrhea Prevention
Education plays a vital role in gonorrhea prevention, particularly regarding awareness of risk factors, symptoms, and the importance of vaccination. By providing information through sexual health clinics and educational initiatives, health authorities can empower individuals to take proactive steps in managing their sexual health. Understanding the significance of STI testing and the availability of vaccines can greatly affect behaviors and ultimately decrease transmission rates.
Furthermore, education on gonorrhea should encompass discussions about safe sexual practices and the importance of mutual responsibility among sexual partners. By encouraging open dialogue and reducing stigma associated with STIs, we can foster environments where individuals feel confident seeking help and information. An informed public is better equipped to make choices that protect not only their health but also the health of their partners, forming a strong foundation for effective STI prevention strategies.
Community Engagement and Gonorrhea Vaccination
Community engagement is essential to the success of public health initiatives, particularly with the rollout of the gonorrhea vaccination program. Involving community advocates and organizations in outreach efforts can significantly enhance awareness and acceptance of the meningococcal B vaccine among high-risk populations. By building trust and rapport within communities, public health campaigns can effectively disseminate information about the importance of STI prevention and vaccination, encouraging participation in programs aimed at reducing gonorrhea rates.
Additionally, community leaders can play a crucial role in combating misinformation and addressing concerns related to vaccination. By working collaboratively, public health institutions and community groups can create targeted messaging that resonates with the specific demographics they aim to reach. This cooperative effort not only promotes vaccine uptake but also strengthens community resilience against STIs, fostering a proactive approach to sexual health that benefits everyone.
Future Directions in Gonorrhea Prevention
As the landscape of gonorrhea infections continues to evolve, future directions in prevention will require a multifaceted approach. Continued research and development of effective vaccines against Neisseria gonorrhoeae are paramount, but existing strategies must also be optimized. The integration of vaccination with comprehensive treatment, education, and regular screenings will be vital in curbing the spread of this resilient infection, ensuring that public health measures evolve in tandem with changing patterns of STIs.
Moreover, the collaboration between healthcare providers, researchers, and communities will be essential in shaping the future of gonorrhea prevention. By focusing on data-driven approaches that evaluate the effectiveness of vaccination programs and treatment interventions, stakeholders can adapt their strategies to meet the ongoing challenges presented by STIs. This forward-thinking mindset will ultimately enhance public health responses and develop robust frameworks for managing and preventing gonorrhea, ensuring a healthier future for all.
Frequently Asked Questions
What is the gonorrhea vaccination program offered by sexual health clinics in the UK?
The gonorrhea vaccination program in the UK involves administering the meningococcal B vaccine (4CMenB) to high-risk individuals, such as gay and bisexual men with recent histories of multiple sexual partners or bacterial STIs. This program aims to reduce the spread of gonorrhea and combat rising antibiotic resistance.
How effective is the meningococcal B vaccine in preventing gonorrhea?
The meningococcal B vaccine (4CMenB) provides moderate cross-protection against gonorrhea, with studies showing effectiveness ranging from 30% to 40%. It helps prevent infection and is part of the National Health Service’s strategy for STI prevention.
Who is eligible for the gonorrhea vaccination in the UK?
Eligible candidates for the gonorrhea vaccination include gay and bisexual men who have had multiple sexual partners or a bacterial STI in the past 12 months, as identified in the NHS gonorrhea program.
Why is the gonorrhea vaccination important for sexual health?
The gonorrhea vaccination is crucial for sexual health as it aims to curb infections that have surged in the UK, with cases reported in 2023 reaching an all-time high. Vaccination helps reduce the transmission of gonorrhea and the prevalence of antibiotic-resistant strains.
How does the UK’s gonorrhea vaccination program fit into wider STI prevention efforts?
The gonorrhea vaccination program is part of broader STI prevention initiatives in the UK, including access to sexual health clinics and education on safe practices. It complements existing treatments and supports efforts to reduce the rising rates of STIs.
What are the expected outcomes of the gonorrhea vaccination rollout?
The rollout of the gonorrhea vaccination is expected to significantly reduce the incidence of gonorrhea, potentially preventing over 100,000 cases within a decade and saving the NHS considerable healthcare costs associated with STIs.
What role do sexual health clinics play in the gonorrhea vaccination program?
Sexual health clinics play a vital role in the gonorrhea vaccination program by offering the meningococcal B vaccine to high-risk populations, thereby facilitating STI prevention and control efforts in their communities.
Can the meningococcal B vaccine replace traditional gonorrhea treatment?
No, the meningococcal B vaccine cannot replace traditional gonorrhea treatment; it offers additional protection but should be used in conjunction with standard STI treatments and preventive measures.
What public health strategies are supporting the gonorrhea vaccination initiative?
Public health strategies supporting the gonorrhea vaccination initiative include increased access to sexual health clinics, public awareness campaigns, and ongoing research to monitor the effectiveness of the vaccination program in the community.
What has the response been from health officials regarding the gonorrhea vaccination initiative?
Health officials, including Amanda Doyle, NHS national director for primary care, and Ashley Dalton, UK Minister for Public Health, have positively endorsed the gonorrhea vaccination initiative as a significant breakthrough in controlling STI infections.
| Key Point | Details |
|---|---|
| NHS Gonorrhea Vaccination Program | Sexual health clinics in the UK are now offering vaccination for gonorrhea, particularly for at-risk individuals. |
| 4CMenB Vaccine | Although there is no gonorrhea-specific vaccine, the 4CMenB vaccine is recommended for gay and bisexual men with certain health risks. |
| Vaccine Effectiveness | The 4CMenB vaccine provides moderate cross-protection against gonorrhea, with effectiveness reported between 30% and 40%. |
| Projected Impact | Vaccination could prevent over 100,000 gonorrhea cases and save the NHS around £7.9 million in ten years. |
| Rising Gonorrhea Rates | Gonorrhea cases in the UK have tripled since 2012, reaching the highest levels since 1918. |
Summary
Gonorrhea vaccination is becoming a crucial step in combating the rise of gonorrhea infections in the UK. With the introduction of the 4CMenB vaccine targeting high-risk individuals, health authorities aim to mitigate the increasing prevalence of this STI. The initiative not only focuses on protecting individual health but also addresses the broader public health crisis associated with rising antibiotic resistance. As health organizations continue to implement this vaccination program, it is vital for at-risk populations to take advantage of this preventive measure.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.