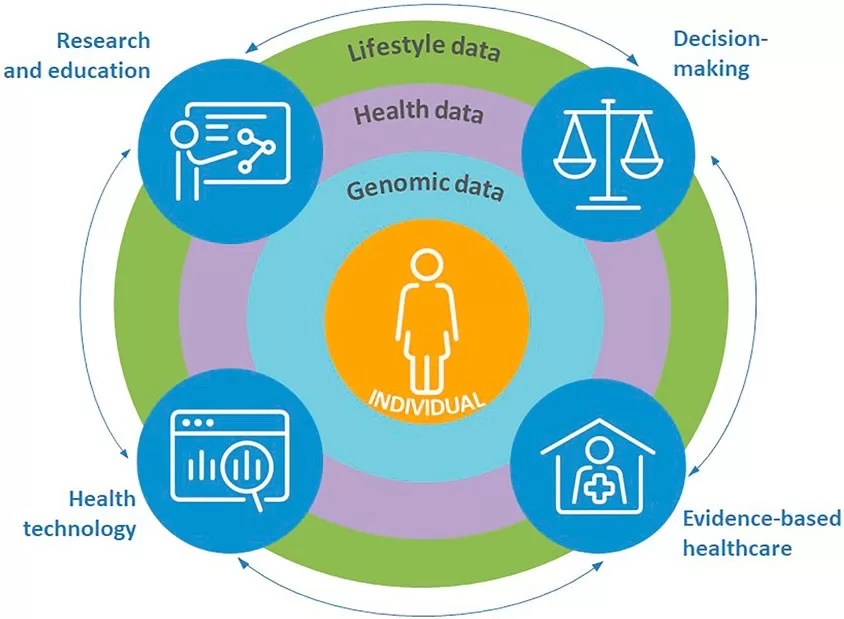
Genomic data in public health is revolutionizing our approach to combating antimicrobial resistance (AMR) and safeguarding effective medical treatments. As multidrug-resistant organisms (MDROs), such as carbapenemase-producing organisms (CPOs), continue to pose significant threats to human health, the necessity for advanced genomic surveillance methods becomes ever more pressing. With whole-genome sequencing (WGS) technology, public health agencies can analyze genetic sequencing data to better understand the transmission dynamics of these pathogens. This innovative approach not only enhances the identification of outbreaks but also informs strategic responses to mitigate AMR spread. By harnessing genomic insights, we are paving the way for a more effective public health response against the rising tide of antimicrobial resistance, a crucial element in protecting public health and ensuring patient safety.
Infectious disease management faces an unprecedented challenge with the rise of drug-resistant infections, which is why leveraging genomic information in public health is vital. The term “genomic epidemiology” is increasingly relevant in discussions around antimicrobial resistance, encompassing the study of genetic variations in pathogens that cause disease outbreaks. This approach allows for a more nuanced understanding of the spread of multidrug-resistant organisms by integrating genomic data with traditional epidemiological methods. Furthermore, genomic surveillance technologies are essential for tracking the evolution and transmission of carbapenemase-producing organisms, ensuring timely public health interventions. By adopting these cutting-edge methods, public health sectors can enhance their ability to respond to emerging threats posed by resistant bacteria.
The Importance of Genomic Surveillance in Combating Antimicrobial Resistance
Genomic surveillance plays a critical role in the fight against antimicrobial resistance (AMR) by providing health officials with the tools needed to trace and manage multidrug-resistant organisms (MDROs). By employing whole-genome sequencing (WGS), public health authorities can decipher the genetic makeup of pathogens, enabling them to distinguish between strains and track their evolution and spread. This level of detail is particularly vital for understanding the transmission dynamics of carbapenemase-producing organisms (CPOs), which are known for their resilience against many antibiotics, thus posing a grave risk to modern medical practices.
The collaborative nature of genomic surveillance enhances the efficiency of AMR monitoring. By integrating genomic data with epidemiological investigations, health departments can identify outbreaks more swiftly and accurately. This synergy minimizes the reliance on traditional methods which may overlook critical connections between cases, especially in complex healthcare environments. Ultimately, the integration of genomic data ensures that public health responses are not only more informed but also more timely, allowing for targeted interventions that can prevent further spread of MDROs.
Combining Epidemiological and Genomic Data for Effective Surveillance
The integration of genomic data into traditional epidemiological frameworks is transforming how health authorities approach AMR outbreaks. For instance, during recent investigations in Washington, genomic analyses revealed clusters of infections that aligned with epidemiologically defined outbreaks, highlighting the efficacy of this approach. The findings emphasize that overlapping genomic sequences can indicate not only transmission pathways but also potential reservoirs for CPOs in healthcare settings, allowing for more effective containment strategies to be implemented.
Moreover, the use of genomic surveillance facilitates a more nuanced understanding of how MDROs proliferate across different settings. By examining the genetic relationships between isolated strains, health officials can identify transmission routes across healthcare facilities and communities. This insight is invaluable, as it allows agencies to deploy resources strategically and tailor public health messages to target both healthcare providers and the public, ultimately curbing the spread of antibiotic-resistant infections.
Genomic Data in Public Health: A New Frontier for AMR Management
The utilization of genomic data in public health is emerging as a transformative approach to manage and mitigate antimicrobial resistance, particularly in the context of multidrug-resistant organisms. As demonstrated in Washington State, genomic surveillance offers insights that are crucial for not only identifying outbreaks but also understanding the complex genetic mechanisms behind resistance. With the global rise of CPOs, the integration of genomic data allows public health officials to establish more effective surveillance systems that can quickly respond to emerging threats. This data-driven approach underlines the necessity of modernizing public health strategies to accommodate rapid advances in genomic technologies.
In essence, genomic data collection and analysis serve as a backbone for shifting health policies towards a more sophisticated response to AMR. By embracing these new methodologies, public health agencies can gain a comprehensive view of the landscape of antibiotic resistance, informing both research and public health initiatives. Consequently, investment in genomic surveillance not only bolsters the immediate response to outbreaks but also lays the groundwork for sustained efforts to understand and combat the evolving challenge of antimicrobial resistance.
Challenges and Opportunities in Implementing Genomic Surveillance Systems
While the integration of genomic data into surveillance systems holds immense promise for addressing antimicrobial resistance, there are significant challenges that must be navigated. Chief among these is the need for robust infrastructure capable of processing and analyzing genomic data at scale. Effective implementation requires collaboration between laboratories, public health officials, and healthcare providers to ensure the data collected are both comprehensive and actionable. Additionally, issues around data sharing and privacy can hinder the timely exchange of critical information needed for public health responses.
Despite these challenges, the opportunities presented by genomic surveillance are vast. For example, establishing a centralized database for genomic information allows for real-time tracking of outbreaks and the dissemination of knowledge across health sectors. Furthermore, educational initiatives that emphasize the value of genomic data in fighting AMR can foster a culture of collaboration and innovation among healthcare professionals. Ultimately, while barriers exist, the potential to advance public health outcomes through genomic surveillance is substantial, marking a crucial step forward in the battle against antimicrobial resistance.
The Future of Genomic Data in Public Health Strategies
As genomic technologies continue to evolve, their role in public health strategies against antimicrobial resistance is set to expand significantly. Future initiatives may leverage advancements in bioinformatics to enhance data analysis capabilities, paving the way for more personalized public health responses tailored to specific populations or outbreak scenarios. The emphasis on precision public health can lead to more efficient resource allocation, particularly in managing cases involving multidrug-resistant organisms.
Additionally, incorporating genomic data into educational programs for healthcare professionals can foster a more profound understanding of the implications of antimicrobial resistance. With a focus on collaborative efforts, health agencies can cultivate partnerships that bridge the gap between clinical practice and disease surveillance. In this context, genomic surveillance is not merely a tool for monitoring pathogens; it is an integral component of a comprehensive strategy for managing public health effectively as we face the ever-growing challenge of AMR.
Frequently Asked Questions
What is the role of genomic data in public health surveillance for antimicrobial resistance?
Genomic data plays a crucial role in public health surveillance for antimicrobial resistance (AMR) by enabling detailed analysis and tracking of multidrug-resistant organisms (MDROs). It facilitates the identification of specific strains responsible for infections, like carbapenemase-producing organisms (CPOs), aiding in early detection and outbreak management. Through whole-genome sequencing (WGS), public health officials can enhance their response strategies by integrating genomic insights with traditional epidemiological data.
How does genomic surveillance improve the detection of multidrug-resistant organisms?
Genomic surveillance improves the detection of multidrug-resistant organisms by providing high-resolution data that uncovers genetic relationships among bacterial strains. This method, specifically through whole-genome sequencing (WGS), allows public health agencies to identify transmission pathways and outbreak clusters, particularly for carbapenemase-producing organisms (CPOs). Such detailed genomic insights lead to more effective AMR strategies and public health interventions.
What are the benefits of using whole-genome sequencing (WGS) in public health for AMR surveillance?
The benefits of using whole-genome sequencing (WGS) in public health for AMR surveillance include enhanced precision in identifying multidrug-resistant organisms (MDROs) and understanding their transmission dynamics. WGS provides comprehensive genomic profiles, which help in characterizing outbreaks, determining the genetic basis of antimicrobial resistance, and guiding treatment options. This genomic approach allows for timely public health responses to emerging threats, especially concerning carbapenemase-producing organisms (CPOs).
How can genomic data address gaps in traditional epidemiological surveillance of AMR?
Genomic data can address gaps in traditional epidemiological surveillance of antimicrobial resistance (AMR) by providing comprehensive insights into the genetic makeup and relatedness of bacterial strains. This information enhances outbreak detection and definitions, as seen with carbapenemase-producing organisms (CPOs), by linking cases that traditional methods might miss. By integrating genomic surveillance with epidemiological investigations, public health authorities can refine their understanding of transmission patterns and improve outbreak response strategies.
What public health strategies are supported by genomic analysis of multidrug-resistant organisms?
Public health strategies supported by genomic analysis of multidrug-resistant organisms (MDROs) include enhanced outbreak response, targeted surveillance systems, and development of intervention measures to combat antimicrobial resistance (AMR). Through genomic insights, authorities can prioritize resources effectively, monitor the spread of resistant strains, particularly carbapenemase-producing organisms (CPOs), and inform clinical treatment decisions, ultimately improving patient outcomes and community health.
Why is monitoring carbapenemase-producing organisms (CPOs) critical in public health?
Monitoring carbapenemase-producing organisms (CPOs) is critical in public health due to their resistance to carbapenems, often considered last-line antibiotics for serious infections. The high mortality rates associated with CPO infections necessitate ongoing surveillance and genomic analysis to prevent further spread and mitigate antimicrobial resistance (AMR). Effective CPO monitoring allows public health officials to detect outbreaks quickly and implement control measures to protect public health.
| Key Points | Details |
|---|---|
| Public Health Priority | Mitigating antimicrobial resistance (AMR) to preserve treatment options. |
| Pilot Program | Washington State Department of Health’s approach to genomic surveillance using whole-genome sequencing (WGS). |
| Organism Focus | Six outbreaks involving *Pseudomonas aeruginosa*, *Acinetobacter baumannii*, and *Klebsiella pneumoniae*. |
| Methodology | Analysis of genomic and epidemiological data to define outbreaks and identify linkages between cases. |
| Results | Genomic clusters aligned with epidemiological data, enhancing outbreak definition and response. |
| Discussion | Integration of genomic data improved outbreak investigations and clarified transmission pathways. |
Summary
Genomic data in public health plays a crucial role in modernizing how we approach antimicrobial resistance (AMR). The Washington State Department of Health exemplifies this by leveraging genomic surveillance systems to enhance our understanding of multidrug-resistant organisms (MDROs). By integrating whole-genome sequencing with traditional epidemiological data, public health authorities can improve outbreak detection, refine case definitions, and ultimately combat the spread of AMR more effectively. This innovative approach underscores the importance of collaborative data sharing and the need for robust surveillance systems in addressing public health challenges.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.