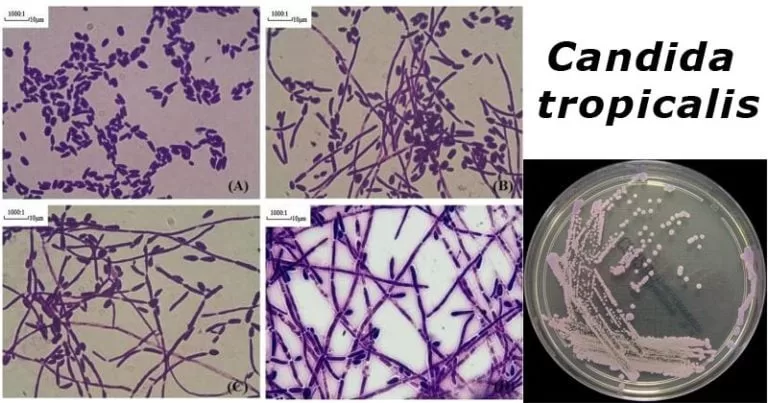
Flucytosine-resistant Candida tropicalis has emerged as a troubling public health concern, particularly in the Netherlands, where case studies reveal an alarming increase in non-Wild Type (WT) strains. This antifungal resistance challenges conventional treatment protocols for fungal infections, as C. tropicalis is already recognized as the second most virulent Candida species after C. albicans. The emergence of resistant C. tropicalis clades, accounting for over 40% of isolates by 2022, emphasizes the urgent need for ongoing surveillance and innovative therapeutic strategies. Studies have linked this resistance to genetic mutations, particularly in the FCY2 gene, further complicating the antifungal landscape. Understanding the mechanisms behind C. tropicalis resistance is crucial for developing effective treatment options and mitigating the risk of severe infections among vulnerable populations.
The rise of antifungal-resistant strains of Candida tropicalis represents a significant challenge in the treatment of debilitating fungal infections. As a member of the Candida genus, C. tropicalis has demonstrated a remarkable ability to adapt and resist common antifungal agents like flucytosine (5-FC), alarming healthcare professionals and researchers alike. This ongoing resistance trend necessitates a close examination of the genetic factors driving clade variations, particularly as these alterations in susceptibility impact patient outcomes. With findings indicating a notable emergence of high MIC values among clinical isolates, future treatment strategies must incorporate real-time surveillance mechanisms to effectively manage and combat Candida tropicalis resistance.
Understanding Flucytosine Resistance in Candida tropicalis
Flucytosine resistance in Candida tropicalis represents a significant challenge in managing fungal infections. This particular species has been increasingly implicated in candidemia, particularly among immunocompromised patients. A recent study highlighted that over 40% of C. tropicalis isolates collected in the Netherlands from 2012 to 2022 exhibited reduced susceptibility to flucytosine. This raises concerns over traditional antifungal treatment strategies that rely on 5-FC, necessitating a deeper understanding of the resistance mechanisms at play.
Research indicates that a mutation in the FCY2 gene is responsible for the non–wild-type (WT) strains, marking a critical turning point in antifungal resistance profiles. By employing advanced methods such as whole-genome sequencing, researchers can track these genetic alterations to better predict the behavior of these pathogenic strains in clinical settings. Understanding the genetic underpinnings of antifungal resistance can inform better treatment approaches and facilitate the development of new therapeutic strategies.
The Epidemiological Impact of C. tropicalis Resistance
The emergence of flucytosine-resistant C. tropicalis clades has significant epidemiological implications. The data collected over the past decade reveals a troubling trend in the prevalence of non-WT isolates, which indicates an adaptation of C. tropicalis to antifungal therapies commonly employed to treat these infections. Given the bimodal distribution of minimum inhibitory concentrations (MICs) observed in various isolates, it is crucial for healthcare professionals to recognize these patterns to enhance antifungal stewardship.
In clinical practice, the rise of antifungal resistance necessitates an urgent reassessment of treatment protocols for candidemia. The shift in resistance patterns among C. tropicalis isolates can lead to increased morbidity and mortality rates if not managed appropriately. Consequently, there is a pressing need for ongoing surveillance and research to understand the dynamics of C. tropicalis resistance, aiming to mitigate the threat posed by these evolving pathogens.
Genetic Mechanisms Behind Antifungal Resistance
The genetic basis for antifungal resistance in Candida tropicalis is a primary focus for researchers aiming to combat these infections effectively. The identification of mutations in genes such as FCY2 has been pivotal in understanding how resistance develops. These insights are not only crucial for diagnosis but can also pave the way for innovative treatment approaches that target these genetic anomalies.
For instance, by integrating genomic data with antifungal susceptibility profiles, clinicians can potentially tailor treatment regimens to address specific resistance mechanisms. This approach not only optimizes the efficacy of current antifungal agents but also aids in the development of new agents that can bypass existing resistance pathways, ultimately improving outcomes for patients afflicted with resistant fungal infections.
The Role of Surveillance in Managing Antifungal Resistance
Continued surveillance is essential for tracking the emergence and spread of flucytosine-resistant Candida tropicalis. Regular monitoring enables healthcare institutions to detect shifts in resistance patterns, which are critical for alerting clinicians to potential treatment failures. In the Netherlands, the systematic collection of clinical isolates has highlighted the growing prevalence of certain C. tropicalis clades that demonstrate heightened resistance to 5-FC.
Establishing robust surveillance networks can facilitate the sharing of data across institutions, helping to inform public health strategies aimed at controlling antifungal resistance. By staying vigilant, public health officials and medical professionals can work collaboratively to implement effective interventions, reducing the overall impact of resistant C. tropicalis and protecting vulnerable populations from severe complications associated with candidemia.
Antifungal Strategies Against Resistant C. tropicalis
Addressing the challenge of flucytosine-resistant Candida tropicalis requires a multifaceted strategy that encompasses both clinical treatment and ongoing research. Traditional antifungal therapies may need to be reassessed in light of emerging resistance, prompting healthcare providers to consider alternative agents that are effective against resistant strains. The development of new antifungal compounds or combination therapies could enhance efficacy and curb the spread of resistance.
Additionally, educating healthcare providers on the importance of antifungal stewardship can lead to more judicious prescribing practices. By minimizing unnecessary use of flucytosine and other antifungals, the pressure on C. tropicalis populations to develop further resistance can be alleviated. Ultimately, implementing a combination of advanced therapeutic strategies and educational initiatives will be critical in managing this public health threat.
The Clinical Consequences of Antifungal Resistance
The clinical ramifications of antifungal resistance in Candida tropicalis are profound. As more strains demonstrate reduced susceptibility to flucytosine, healthcare providers face the risk of ineffective treatments leading to worsened patient outcomes. The ability to manage infections effectively diminishes with the rise in resistant strains, leading to increased healthcare costs and prolonged hospital stays.
Furthermore, resistant C. tropicalis poses a particular threat to immunocompromised individuals, who are already at heightened risk for severe infections. This underscores the necessity for rapid diagnostics that can identify resistant organisms early in the clinical course, allowing for timely intervention and adjustment of therapeutic strategies.
Research Insights into C. tropicalis Resistance Mechanisms
Research into the mechanisms behind C. tropicalis resistance to antifungal agents provides critical insights for the medical community. Detailed studies have uncovered specific genetic mutations that play a pivotal role in enabling the organism to withstand treatments. For example, the identified mutation in the FCY2 gene not only alters drug uptake but also highlights the need for more comprehensive understanding of the genetic landscape of resistant strains.
Incorporating these insights into future research agendas can lead to breakthroughs in antifungal development. Understanding the interplay between various resistance mechanisms might facilitate the formation of targeted therapies that could re-sensitize resistant C. tropicalis strains to traditional antifungal agents, ultimately improving management strategies for these challenging infections.
Challenges in Treating Candidemia Due to Resistance
The increasing resistance of Candida tropicalis to flucytosine presents several challenges in treating candidemia. Clinicians are often faced with difficult decisions regarding alternative antifungal agents, which may not have the same efficacy for resistant strains. As traditional therapies fall short, the necessity for innovative antifungal strategies becomes evident.
Furthermore, the potential for treatment failures could lead to serious complications, including sepsis, in vulnerable patient populations, emphasizing the critical need for early and accurate identification of resistant strains. Integrating advanced testing methods can provide clinicians with necessary information to adjust their approach, thereby lowering the risk of adverse outcomes associated with C. tropicalis infections.
Global Implications of Antifungal Resistance Trends
The trends in antifungal resistance among Candida tropicalis strains are not confined to the Netherlands but rather reflect a global public health challenge. As resistance patterns evolve, they highlight vulnerabilities within healthcare systems worldwide. Countries with high rates of antifungal use must pay close attention to these trends, as unchecked resistance can lead to severe outbreaks and increased mortality.
International collaborations in research and surveillance can pave the way for comprehensive strategies to combat C. tropicalis resistance globally. Data sharing and coordinated responses to emerging threats are essential in crafting effective public health initiatives, ultimately aiming to safeguard populations against the rising tide of antifungal-resistant pathogens.
Frequently Asked Questions
What is Flucytosine-Resistant Candida tropicalis and why is it concerning?
Flucytosine-Resistant Candida tropicalis refers to strains of the Candida tropicalis species that exhibit resistance to the antifungal medication flucytosine (5-FC). This resistance is concerning because C. tropicalis is a significant pathogen, especially in immunocompromised patients, and rising resistance levels complicate treatment options and increase the risk of severe fungal infections.
What factors contribute to C. tropicalis resistance to flucytosine?
C. tropicalis resistance to flucytosine is primarily driven by genetic mutations, specifically identified mutations in the FCY2 gene that disrupt the uptake and metabolism of the drug. These genetic changes enhance the survival of C. tropicalis in the presence of antifungals, leading to increased prevalence of resistant strains.
How prevalent is Flucytosine-Resistant Candida tropicalis in recent studies?
Recent studies have indicated a concerning rise in Flucytosine-Resistant Candida tropicalis, with certain clades of non-wild-type C. tropicalis accounting for over 40% of isolates collected in the Netherlands between 2012 and 2022. This significant presence raises alarms for healthcare providers regarding the management of systemic fungal infections.
What challenges does antifungal resistance in Candida tropicalis pose for treatment?
Antifungal resistance in Candida tropicalis, particularly to flucytosine, presents major treatment challenges as it limits the effectiveness of standard antifungal therapies. This necessitates the need for healthcare practitioners to explore alternative treatment modalities and highlights the importance of susceptibility testing to guide effective therapy.
What are the clinical implications of the emergence of non-WT C. tropicalis isolates?
The emergence of non-wild-type (non-WT) C. tropicalis isolates has significant clinical implications, including the potential for treatment failures and increased mortality rates among infected patients. Ongoing surveillance and adjustments in clinical protocols are essential to adapt to the changing resistance patterns.
Why is ongoing surveillance important for managing Flucytosine-Resistant Candida tropicalis?
Ongoing surveillance is crucial for managing Flucytosine-Resistant Candida tropicalis to monitor the prevalence and spread of resistant strains. This allows healthcare systems to implement timely interventions, adjust treatment guidelines, and develop strategies to mitigate the impact of antifungal resistance on public health.
What does the term ‘5-FC susceptibility’ refer to in the context of C. tropicalis?
‘5-FC susceptibility’ refers to the effectiveness of the antifungal agent flucytosine in inhibiting the growth of Candida tropicalis. Testing for 5-FC susceptibility is vital in determining the appropriate antifungal treatment, especially given the rise in resistance observed in certain C. tropicalis isolates.
How can healthcare professionals address flucytosine resistance in Candida tropicalis?
Healthcare professionals can address flucytosine resistance in Candida tropicalis by implementing routine antifungal susceptibility testing, utilizing combination therapies, optimizing infection control measures, and staying informed about current resistance trends to adapt treatment plans accordingly.
What genetic mechanisms underlie flucytosine resistance in C. tropicalis?
Flucytosine resistance in Candida tropicalis is mainly attributed to mutations in the FCY2 gene, which are critical for the drug’s efficacy. Understanding these genetic mechanisms is essential for developing targeted therapies and enhancing the effectiveness of existing antifungal treatments.
What role does the Candida tropicalis clade play in antifungal resistance?
The emergence of specific Candida tropicalis clades that exhibit antifungal resistance indicates a shift in the epidemiology of fungal infections. These clades often carry genetic mutations that enhance their ability to resist treatment, making them a focal point for research and clinical attention in the context of managing fungal infections.
| Key Points | Details |
|---|---|
| Emergence of Flucytosine Resistance | Increased incidence of flucytosine-resistant Candida tropicalis clade identified since 2012 in the Netherlands, with over 40% of isolates resistant by 2022. |
| Background Information | Candida tropicalis is the second most virulent Candida species. Resistance to flucytosine is a growing concern, especially among immunocompromised populations. |
| Study Population | The study included 250 C. tropicalis isolates collected from 2012 to 2022 across various clinical settings in the Netherlands. |
| Genetic Mechanism of Resistance | A mutation in the FCY2 gene was associated with 5-FC resistance, indicating a genetic basis for the observed resistance patterns. |
| Importance of Surveillance | Continued surveillance is crucial to monitor the spread of resistance and to guide treatment protocols effectively. |
Summary
Flucytosine-resistant Candida tropicalis presents a growing challenge to public health, particularly due to its significant increase in prevalence and virulence among susceptible populations. The identified genetic mutations, particularly in the FCY2 gene, emphasize the urgent need for continuous monitoring and research to address antifungal resistance effectively. Healthcare professionals must remain vigilant and adapt treatment strategies to combat the rising incidence of this resistant strain.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.