Flu hospitalization associated with underlying medical conditions presents a significant risk during influenza seasons, especially for individuals suffering from chronic illnesses. According to a comprehensive CDC influenza study, patients with conditions like congestive heart failure (CHF) face an elevated risk of hospitalization due to the flu, with CHF patients being four times more likely to require hospital care. The research, which analyzed data from healthcare systems across California and Minnesota, highlights the critical link between underlying medical conditions and severe flu outcomes. This increased hospitalization risk underscores the importance of vaccination and flu risk management strategies for high-risk groups. By understanding the implications of underlying health issues on influenza hospitalization, we can work towards better health outcomes through targeted preventive measures.
The connection between seasonal viruses like influenza and pre-existing health issues is a matter of growing concern. High-risk patients, especially those with chronic ailments, experience more severe symptoms and complications when infected with the flu virus. Studies reveal that individuals with conditions such as heart disease, diabetes, and chronic respiratory illnesses are more susceptible to hospitalization during flu outbreaks. With the CDC emphasizing the importance of flu vaccinations for vulnerable populations, there is an urgent need to focus on preventive health measures for those with these underlying health challenges. Addressing the hospitalization risks related to flu can significantly enhance the well-being of these individuals during times of increased viral activity.
Understanding the Risks of Influenza Hospitalization for Patients with Underlying Medical Conditions
Influenza hospitalization risk is significantly elevated for individuals who have underlying medical conditions (UMCs). A recent study conducted by the CDC reveals that patients suffering from various health issues, particularly congestive heart failure (CHF), are at a notably higher risk of hospitalization due to flu infections. In fact, those with CHF were found to be four times more likely to be hospitalized compared to individuals without any underlying health concerns. This statistic emphasizes the critical need for targeted preventative measures among vulnerable populations.
The implications of these findings are profound, suggesting that healthcare providers must closely monitor and manage patients with underlying medical conditions to mitigate their risk for severe influenza complications. Conditions such as chronic obstructive pulmonary disease (COPD), diabetes, and cardiovascular diseases notably increase susceptibility to influenza-related hospitalizations. Understanding these risk factors can aid healthcare professionals and public health officials in implementing effective flu vaccination campaigns and ultimately reducing the burden of influenza in high-risk groups.
CDC Study Highlights Importance of Vaccination for High-Risk Populations
The importance of influenza vaccination cannot be overstated, especially for individuals with underlying medical conditions. The CDC study highlights that a higher vaccination prevalence among those at risk results in significantly decreased hospitalization rates. For instance, if vaccination levels were lower, the rates of flu-related hospitalizations among those with UMCs would have been notably higher. This underscores the effectiveness of vaccinations as a crucial tool in preventing severe flu cases and emergency health crises.
Patients with multiple underlying conditions are at an even greater risk. The study shows that the hospitalization rate increases with each additional UMC. Patients with four or more underlying conditions are nearly 60% more likely to be hospitalized for flu than those without any. Hence, targeted vaccination campaigns that focus on educating high-risk individuals about the need for flu shots, alongside easy access to vaccination services, are essential strategies that can drastically reduce flu-related health complications within these vulnerable populations.
Identifying High-Risk Groups for Influenza Complications
Identifying and understanding high-risk groups for influenza complications is crucial for managing public health effectively. Patients with underlying medical conditions such as asthma, chronic kidney disease, and neurological disorders are systematically more susceptible to severe outcomes from influenza infections. The CDC’s analysis of electronic health records demonstrates clear trends: those with pre-existing health issues not only face higher rates of flu hospitalizations but also experience increased severity of symptoms when infected.
Therefore, healthcare providers must prioritize screening for these high-risk groups and ensure they receive timely vaccinations and preventive care. Effective public health messaging should focus on educating both patients and caregivers about the critical need for vaccination to minimize the risk of severe flu complications in individuals with underlying health conditions. This proactive approach can significantly contribute to reducing influenza hospitalization rates in affected populations.
The Role of Data in Understanding Influenza Hospitalization Patterns
Data-driven studies are essential for understanding and mapping influenza hospitalization patterns. The retrospective study conducted across healthcare systems in California and Minnesota provides valuable insights into how underlying medical conditions affect hospitalization due to flu. By analyzing data spanning multiple respiratory virus seasons, researchers identified the prevalence and burden of UMCs, allowing for a more focused understanding of the groups affected by severe influenza outcomes.
This robust analysis not only highlights which conditions pose the most significant risks but also serves as a foundation for public health strategies aimed at preventing influenza hospitalizations. Findings from data like this can drive policy decisions regarding vaccination campaigns, allocation of healthcare resources, and educational initiatives targeting high-risk groups, thereby having a substantial impact on community health outcomes.
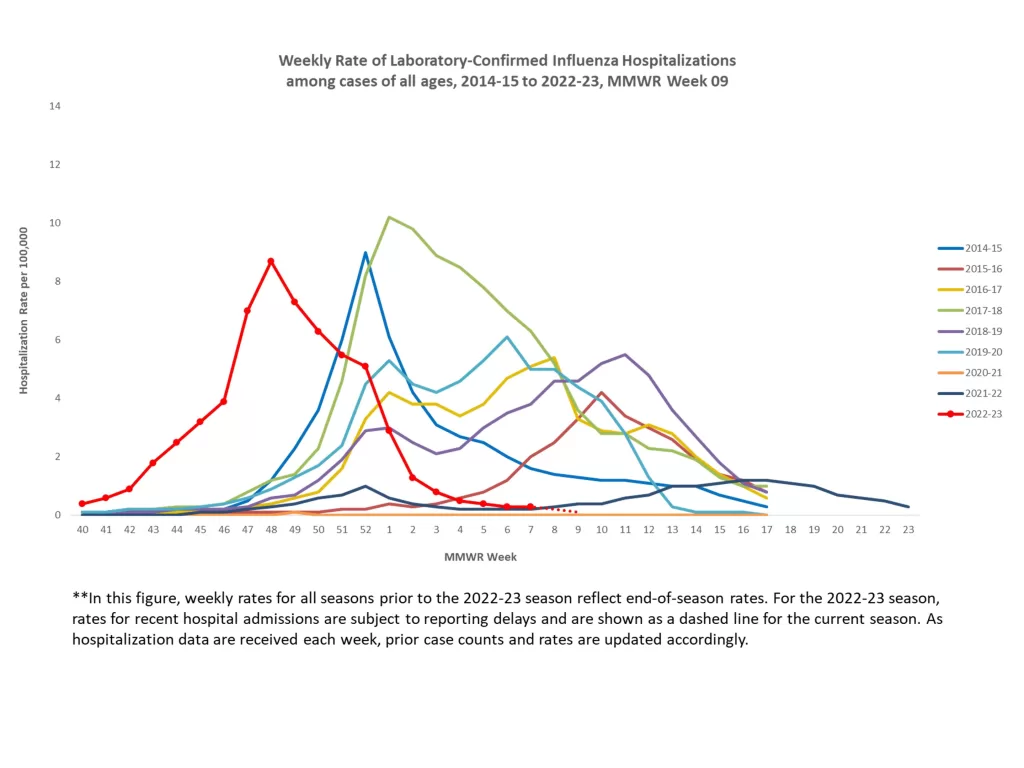
Seasonal Influenza Trends and Hospitalization Risks
Seasonal trends in influenza can significantly impact hospitalization rates. Each flu season, individuals with underlying medical conditions tend to face increased risks, making it essential to track influenza activity closely. The reported hospitalization rates from the CDC indicate that certain seasons can escalate flu severity, particularly among those already compromised by other health issues. Seasonal peaks in influenza viruses can lead to higher rates of acute respiratory illness, further straining healthcare systems.
Moreover, understanding these seasonal trends allows for better preparedness and response strategies in healthcare settings. By anticipating potential surges in hospitalizations, healthcare systems can ensure adequate resources, staffing, and vaccine supplies are in place. This proactive approach is particularly important for managing patients with UMCs, who may require additional support during peak flu seasons.
Preventive Measures Beyond Vaccination for At-Risk Patients
While vaccination remains the primary defense against influenza hospitalizations, additional preventive measures are critical for patients with underlying medical conditions. Strategies such as practicing good hygiene, including regular handwashing and avoiding close contact with sick individuals, can further reduce the risk of infection. Healthcare providers should work with patients to develop comprehensive care plans that incorporate both vaccination and these preventative behaviors to maximize protection against flu.
In conjunction with vaccinations, education on recognizing early symptoms of influenza can empower high-risk patients to seek timely medical attention. Prompt treatment for flu can prevent complications that often lead to hospitalization, particularly for individuals with UMCs. The integration of lifestyle modifications, regular medical check-ups, and health education into the care regimen of these patients represents a holistic approach to managing their health and minimizing flu-related risks.
Impact of Vaccination on Hospitalization Rates in the Elderly
Older adults constitute a significant proportion of the population at risk for severe influenza outcomes. The CDC study indicates that for the elderly with underlying medical conditions, the hospitalization rates due to flu are especially concerning. Vaccination plays a pivotal role in this demographic, helping to mitigate severe disease and subsequent hospitalizations. Evidence shows that influenza vaccination substantially lowers the risk of respiratory infections among seniors, thereby reducing strain on healthcare services.
Health practitioners must emphasize the importance of flu shots for older individuals, particularly those with existing health issues. Enhanced education about vaccine effectiveness and accessibility to vaccinations can lead to higher uptake rates in this vulnerable age group. Consequently, improving vaccination rates among older adults with UMCs is essential to decreasing hospitalization rates and enhancing overall community health.
Healthcare System Preparedness for Flu Seasons
Healthcare system preparedness is crucial when tackling the challenges posed by seasonal influenza, especially for populations with underlying medical conditions. The insights drawn from the CDC’s findings can guide hospitals and clinics in developing contingency plans that cater specifically to at-risk patients. Enhancing staffing levels during flu surges, ensuring that clinics have adequate influenza vaccines, and providing immediate access to care for symptomatic patients are all key components of a robust preparedness strategy.
Furthermore, healthcare systems can implement community outreach programs to encourage vaccination among high-risk individuals. By connecting vulnerable populations with resources and information, they can foster an environment that prioritizes prevention and timely intervention, ultimately reducing severe hospitalization rates and improving health outcomes for those affected by influenza.
Educating Patients and Caregivers About Influenza Risks and Prevention
Patient and caregiver education is a fundamental element of influenza prevention, particularly for those with underlying medical conditions. Understanding the elevated risks associated with flu hospitalizations can encourage proactive health behaviors, such as receiving annual vaccinations, recognizing the symptoms of influenza, and seeking prompt medical care. Educational initiatives should focus on clear messaging regarding the importance of flu shots and the consequences of delayed treatment for individuals at higher risk.
Healthcare providers play a critical role in this educational effort. By fostering open communication with patients and their caregivers, they can effectively convey essential information regarding flu risks, prevention strategies, and the importance of laboratory tests for early detection. Such educational partnerships are vital in ensuring that those with underlying health issues are well-prepared for the flu season, ultimately minimizing the risk of hospitalization.
Frequently Asked Questions
What is the impact of underlying medical conditions on flu hospitalization rates?
Individuals with underlying medical conditions (UMCs) face a significantly higher risk of hospitalization due to flu. Research from the CDC indicates that patients with conditions such as congestive heart failure (CHF) are particularly vulnerable, showing a hospitalization rate that is up to four times greater compared to those without such conditions.
How does the CDC study inform us about flu hospitalization risk?
The CDC study highlights that adults with various underlying medical conditions are at increased risk for hospitalization due to flu. Data indicates that each additional UMC corresponds to a rising hospitalization rate, emphasizing the importance of monitoring and preventive measures for at-risk populations.
Which underlying medical conditions increase the risk of hospitalization due to flu?
Notable underlying medical conditions that increase flu hospitalization risk include congestive heart failure (CHF), chronic obstructive pulmonary disease (COPD), diabetes, and certain blood disorders. Patients with multiple UMCs face an even greater risk, underscoring the need for thorough health assessments during flu season.
What role does vaccination play in preventing flu hospitalization among individuals with UMCs?
Vaccination against the flu is critical for individuals with underlying medical conditions, as it significantly reduces the risk of hospitalization. The CDC study suggests that if vaccination rates were lower, the hospitalization rates for those with UMCs would have been much higher, highlighting the effectiveness of the flu vaccine.
What recommendations does the CDC provide for individuals at high risk for flu hospitalization?
The CDC recommends annual flu vaccination for everyone aged 6 months and older, emphasizing its importance for individuals with underlying medical conditions. Vaccination is a key preventive strategy to protect high-risk groups from severe illness and hospitalization due to influenza.
How prevalent is flu hospitalization among adults with underlying medical conditions?
In the analyzed study involving 870,888 adults, 1,403 were hospitalized due to the flu, representing a hospitalization rate of 1.2 per 1,000 person-years. This figure is notably higher among those with underlying medical conditions, showcasing the heightened vulnerability within this demographic.
Which groups are most affected by flu hospitalization according to the CDC’s findings?
Groups most affected by flu hospitalization include older adults and those with underlying medical conditions such as heart disease, COPD, and diabetes. Each additional UMC can significantly elevate the risk of hospitalization, reinforcing the need for targeted prevention efforts.
What findings did the CDC study reveal about the relationship between UMCs and flu risk?
The CDC study revealed that adults with underlying medical conditions are at a higher risk for acute respiratory illness and hospitalization related to the flu. The data underscored that the risk increases with the number of UMCs, emphasizing the critical nature of preventive measures for these high-risk individuals.
| Underlying Medical Conditions (UMC) | Increased Hospitalization Risk | Vaccination Status |
|---|---|---|
| Congestive Heart Failure (CHF) | 4 times greater than those without CHF | 44% vaccinated |
| Chronic Obstructive Pulmonary Disease (COPD) | 3.0 times greater | 44% vaccinated |
| Blood Disorders | 3.6 times greater | 44% vaccinated |
| Diabetes | Increased risk depending on other UMCs | 44% vaccinated |
| Chronic Kidney Disease, Asthma, etc. | Higher risk with multiple UMCs | 44% vaccinated |
Summary
Flu hospitalization rates are significantly affected by underlying medical conditions (UMC), as individuals with these conditions are more likely to require hospitalization for influenza infection. The recent study by the CDC highlighted that conditions such as congestive heart failure, chronic obstructive pulmonary disease, and others distinctly elevate the risk of hospitalization. These findings underscore the critical importance of flu vaccination, particularly for those with UMCs, to mitigate severe illness and associated hospitalizations.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.