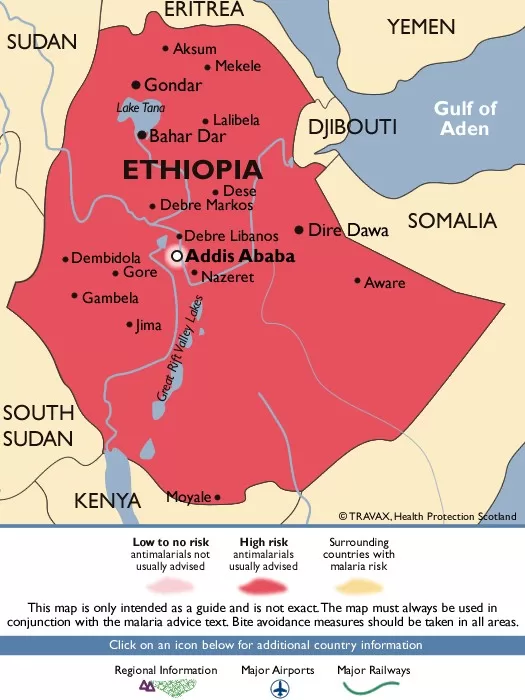
Ethiopia is currently grappling with its worst malaria outbreak in seven years, with staggering reports of more than 7.3 million malaria cases in Ethiopia since the beginning of the year. The World Health Organization (WHO) has confirmed that this health crisis has resulted in at least 1,157 deaths attributed to the deadly Plasmodium falciparum, which accounts for two-thirds of the infections. The western regions, particularly Oromia, Amhara, Southwest, and Southern Ethiopia, have been severely affected, highlighting the urgent need for malaria prevention in Ethiopia. Factors contributing to the surge include seasonal migration to high-risk areas and diminished vector-control efforts, exacerbated by prolonged conflicts and population displacement. With the alarming spread of Anopheles stephensi mosquitoes thriving in urban settings, the focus on effective malaria management and response strategies is more critical than ever to curb this escalating epidemic.
Ethiopia is currently facing a severe health crisis due to a widespread malaria epidemic, which has resulted in millions of reported cases in recent months. The surge in malaria infections, eliciting alarming statistics from the World Health Organization (WHO), underscores the urgent need for public health interventions. Regions like Oromia, Amhara, and Southern Ethiopia are particularly vulnerable, highlighting a critical shift in malaria dynamics. The rapid spread of the Anopheles stephensi mosquito, which flourishes in urban environments, poses new challenges for malaria control in the country. As conditions deteriorate, the focus shifts to strengthening malaria prevention efforts to combat this escalating vector-borne disease.
Overview of the Ethiopia Malaria Outbreak
Ethiopia is currently grappling with a severe malaria outbreak that has reached alarming proportions. The World Health Organization (WHO) reported over 7.3 million malaria cases since the start of the year, with a tragic count of 1,157 fatalities. The predominant culprit, Plasmodium falciparum, is implicated in two-thirds of these infections, highlighting the intensity of the health crisis in the region. Malaria has become a significant burden, affecting large sections of the population, particularly in the western regions of the country, which are well-suited for the reproduction of malaria-carrying mosquitoes.
This outbreak is not just a temporary spike; it indicates a worrying trend that has emerged over the past four years. With the ecological conditions proving favorable for malaria proliferation, regions such as Oromia and Amhara have reported substantially high cases. Increased morbidity and mortality rates illustrate a continuing battle against a disease that had previously been under control, raising urgent concerns about public health strategies and the effectiveness of ongoing malaria prevention efforts in Ethiopia.
Factors Contributing to the Malaria Crisis in Ethiopia
The persistent malaria outbreaks in Ethiopia can be attributed to a combination of factors. One of the primary reasons for the resurgence of malaria cases is diminished vector-control initiatives. For years, these measures were effective in keeping malaria prevalence low, but with conflicts disrupting societal stability and resources, many of these programs have waned, leading to population displacement and increased vulnerability. As seasonal workers move to high-burden areas, the risk escalates, especially among males who represent a significant portion of both outpatient and inpatient cases.
Moreover, the spread of Anopheles stephensi mosquitoes adds another layer of complexity to the crisis. This mosquito species has adapted well to urban environments, leading to increased transmission rates in cities. When coupled with external factors such as drought and food insecurity, the overall risk of malaria in Ethiopia has become unacceptably high. Public health measures must adapt to these changing dynamics to combat both existing and evolving health threats with robust and targeted interventions.
Impact of Climate on Malaria Cases in Ethiopia
Recent climate patterns in Ethiopia have exacerbated the malaria outbreak by creating conditions conducive to mosquito breeding. The country has faced weather anomalies over the past few years, leading to increased rainfall and temperature fluctuations, which are critical in sustaining the lifecycle of malaria vectors. Such climatic irregularities facilitate the higher reproduction rate of mosquitoes, inflicting greater strain on an already overwhelmed health infrastructure. In several regions, including the highland areas that were previously less affected, the rise in temperatures has expanded the malaria endemic zone.
Additionally, these changes in weather are closely tied to agricultural cycles, further complicating the nexus between health and economic stability. Farmers are struggling to adapt, and food insecurity tends to increase during the recruitment of seasonal agricultural workers, which in turn promotes the spread of malaria. This intersection of climate change and health calls for interconnected policies that address both immediate malaria prevention efforts and long-term climate adaptation strategies.
The Role of Health Policy in Addressing Malaria
Health policies play a critical role in managing malaria outbreaks, especially in a rapidly evolving crisis such as experienced in Ethiopia. As malaria cases surge, the Ethiopian government, along with international health organizations like the WHO, must align their policies to focus on re-establishing effective malaria control initiatives. This includes enhancing vector control measures, distributing insecticide-treated bed nets, and increasing access to rapid diagnostic tests and treatment options for those affected. Ensuring robust surveillance systems is also paramount to track malarial trends and respond promptly.
Furthermore, empowering local communities to participate in malaria management can yield significant dividends. Public health education campaigns aimed at raising awareness about prevention tactics and symptoms of malaria could greatly enhance community involvement, leading to better outcomes. Policies that incorporate community health workers as vital resources can help reinforce the fight against malaria by facilitating grassroots engagement and providing much-needed support to erradicate this enduring public health threat.
The Future of Malaria in Ethiopia: Challenges Ahead
The outlook for malaria in Ethiopia remains challenging due to the multitude of factors that contribute to the spread of the disease. As mentioned earlier, the ongoing conflicts and displacement of populations hinder effective control measures and healthcare access. Furthermore, the resurgence of malaria due to Anopheles stephensi underscores the urgent need for adaptive strategies tailored to urban settings, where traditional measures may not suffice. The complexity of these challenges necessitates a multifaceted approach to prevention and treatment.
Looking ahead, Ethiopia must prioritize sustained funding and resource allocation towards malaria eradication efforts. Engaging with local and international partners to increase technical capacity and strengthen health systems will be crucial. The WHO has emphasized the importance of resilience in health initiatives, adapting to both the environmental changes and sociopolitical dynamics that are currently at play. Only through comprehensive planning and community engagement can Ethiopia hope to overcome this severe malaria outbreak and work towards its eventual eradication.
Global Implications of the Ethiopia Malaria Outbreak
The malaria outbreak in Ethiopia has significant implications not only for the nation itself but also for the surrounding regions and the global community. As Ethiopia becomes a central point in the African cluster dealing with resurgent malaria, neighboring countries may face increased risks associated with cross-border transmission. This regional threat underscores the necessity for collaborative efforts in surveillance and health system strengthening among countries across the Horn of Africa. A unified response is critical to contain outbreaks effectively and prevent further spread.
Additionally, the international community must also recognize the broader implications of health crises such as these. It stands as a reminder of the interconnectedness of global health security; infectious diseases know no borders. Investments in global health initiatives to bolster capacity in low-resource settings can diminish the effects of outbreaks in vulnerable areas. With the global population rising and the climate crisis intensifying, ensuring robust and effective malaria prevention and management strategies will benefit not only affected nations but contribute to global public health stability.
Community Empowerment in Malaria Prevention
Community engagement is fundamental in combatting malaria, particularly in places experiencing severe outbreaks like Ethiopia. Empowering local populations with knowledge and resources equips them to take an active role in prevention efforts. Local health workers can become champions of malaria awareness, ensuring that information about transmission, prevention, and available treatments reaches those most affected. Mobile clinics and community health education can significantly bolster the response to this outbreak while fostering a sense of ownership among the community members.
Moreover, community-based initiatives can amplify the effectiveness of existing malaria control programs. Collaborative efforts involving local leaders, schools, and families can enhance the dissemination of preventive measures, such as the importance of using bed nets and seeking treatment promptly. By incorporating culturally appropriate strategies that resonate with local practices, communities can form a united front against malaria, improving overall health outcomes and contributing to long-term disease management.
Importance of Data and Research in Fighting Malaria
As Ethiopia addresses its ongoing malaria outbreak, the significance of data collection and analysis cannot be overstated. Research efforts are essential to understand the specific trends of malaria transmission, the effectiveness of current prevention measures, and the emergence of drug-resistant strains. The WHO’s thorough malaria reports provide invaluable insights, guiding policy and intervention strategies at both the local and national levels. Continuous monitoring of malaria cases and patterns can better inform healthcare providers and policymakers in adapting to the ever-evolving landscape of malaria transmission.
Investing in research also facilitates the discovery of innovative solutions to combat malaria, such as new vaccines, treatment modalities, and improved vector management techniques. Ethiopia has the opportunity to lead in malaria research on the continent, leveraging its diverse ecology and the urgency of its health crisis. A robust research framework that involves collaboration between universities, health institutions, and international partnerships can provide a pathway to sustainable malaria control efforts, contributing to alleviating the health crisis in Ethiopia.
Preventive Measures to Curb Malaria Spread in Ethiopia
Effective malaria prevention is critical in reversing the current trend of increasing cases in Ethiopia. To mitigate the risk of malaria transmission, the deployment of insecticide-treated bed nets (ITNs) must be prioritized across high-burden regions. Since malaria-carrying mosquitoes are primarily active during the night, bed nets provide a reliable barrier against bites and significantly reduce malaria incidence. Furthermore, community awareness programs must emphasize the importance of utilizing these nets consistently for maximum effectiveness.
Additionally, indoor residual spraying (IRS) remains a crucial intervention in controlling malaria outbreaks. Regular spraying of homes can significantly decrease mosquito populations, thereby lowering the chances of new infections. Public health campaigns should also encourage early diagnosis and treatment, enabling individuals to seek medical attention at the onset of symptoms. A comprehensive strategy incorporating both preventive and curative measures will be essential to combat the increasing malaria cases in Ethiopia effectively.
Frequently Asked Questions
What is the current situation regarding the Ethiopia malaria outbreak?
Ethiopia is currently facing its worst malaria outbreak in seven years, with over 7.3 million reported cases since the start of the year, leading to 1,157 deaths according to the WHO. The outbreak is primarily due to the Plasmodium falciparum strain, which is responsible for two-thirds of the cases.
What regions in Ethiopia are most affected by the malaria outbreak?
The western regions of Ethiopia, particularly Oromia, Amhara, Southwest, and Southern Ethiopia Regional State, have reported the highest number of malaria cases during the current outbreak. Favorable ecological conditions in these areas are contributing to the surge in malaria cases in Ethiopia.
How does the Ethiopia malaria outbreak affect men and women?
Current statistics indicate that males account for 56% of outpatient malaria cases and 52% of inpatient admissions during the Ethiopia malaria outbreak. This may be attributed to the movement of seasonal workers to areas that are highly burdened by malaria.
What factors are contributing to the rise of malaria cases in Ethiopia?
The increase in malaria cases in Ethiopia over the past four years can be linked to several factors, including reduced vector-control efforts, prolonged conflicts that have caused population displacement, and a loss of immunity due to decreased malaria control initiatives.
How does climate affect the Ethiopia malaria outbreak?
Weather anomalies, such as prolonged drought, have contributed to the high risk of malaria outbreaks in Ethiopia. These conditions not only favor mosquito breeding but also lead to food insecurity, which exacerbates the overall health crisis.
What role do Anopheles stephensi mosquitoes play in the Ethiopia malaria outbreak?
Anopheles stephensi mosquitoes, which thrive in urban environments, are a significant factor in the current Ethiopia malaria outbreak. Their spread increases the risk of malaria transmission, particularly in urban areas, and poses a challenge for malaria prevention efforts in Ethiopia.
How can malaria be prevented in Ethiopia?
Malaria prevention in Ethiopia requires a multifaceted approach that includes the use of insecticide-treated nets, indoor residual spraying, and health education to mitigate the spread of malaria and the impact of the current outbreak.
What updates has the WHO provided on the Ethiopia malaria outbreak?
According to the latest WHO malaria report, Ethiopia is experiencing a sustained increase in malaria cases, with significant outbreaks continuing in several regions. The WHO emphasizes the need for urgent interventions and increased efforts in malaria control to address the ongoing health crisis.
| Key Point | Details |
|---|---|
| Malaria Cases | Over 7.3 million cases reported in Ethiopia in 2023. |
| Deaths | 1,157 deaths attributed to malaria this year. |
| Primary Cause | Plasmodium falciparum is responsible for two-thirds of cases. |
| Affected Regions | The western regions, particularly Oromia, Amhara, Southwest, and Southern Ethiopia, are most affected. |
| Demographics | Males constitute 56% of outpatient cases and 52% of inpatient admissions. |
| Contributing Factors | Increased malaria activity linked to reduced vector control, population displacement, and loss of immunity. |
| Urban Risk | Spread of Anopheles stephensi mosquitoes threatens urban areas in Ethiopia. |
| Regional Impact | Neighboring countries also face moderate risk due to malaria outbreaks. |
Summary
The Ethiopia malaria outbreak is currently the worst it has seen in seven years, creating a critical public health emergency. With more than 7.3 million cases and over 1,100 fatalities reported, it underscores the urgency for renewed malaria control efforts and vector management strategies. Favorable ecological conditions in the western regions have exacerbated the situation, further complicated by socio-economic challenges and public health infrastructure strains. It is essential to mobilize resources and enact effective measures to combat this outbreak to protect the population’s health.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.