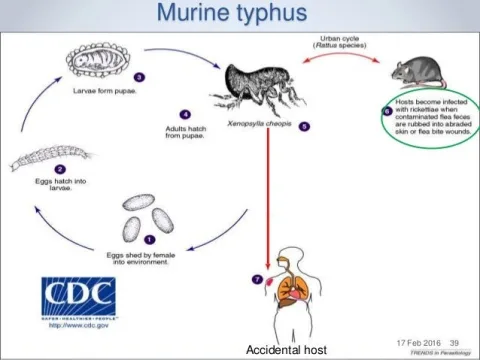
Eschar, a term originating from the Ancient Greek word for “scab,” refers to distinctive skin lesions that play a key role in diagnosing rickettsial infections, particularly related to scrub typhus and spotted fever. These lesions develop at the entry site of rickettsial pathogens, introduced through skin contact with feeding ticks or mites, and typically appear within days of the initial bite. The presence of eschar can be critical in the diagnosis of these infections, especially since they are often painless and may go unnoticed, particularly in individuals with darker skin tones. Understanding eschar is essential for acknowledging its clinical significance and the implications of associated skin lesions in rickettsial pathologies. Therefore, timely recognition and diagnosis of eschar can significantly impact treatment outcomes for patients suffering from these infections.
In the realm of infectious dermatology, terms like “skin ulcerations” and “necrotic lesions” may be used interchangeably with eschar, particularly when discussing symptoms arising from rickettsial infections. These skin manifestations occur when rickettsial pathogens infiltrate the dermis following arthropod bites, such as those from ticks or mites. Understanding these lesions’ characteristics can aid in the management of associated diseases like scrub typhus. Close examination and prompt diagnosis of such ulcerative skin changes are vital to prevent complications linked to untreated rickettsial diseases. By utilizing broader terminologies, healthcare providers can enhance awareness and expedite intervention strategies for patients presenting these concerning symptoms.
Understanding Eschar in Rickettsial Infections
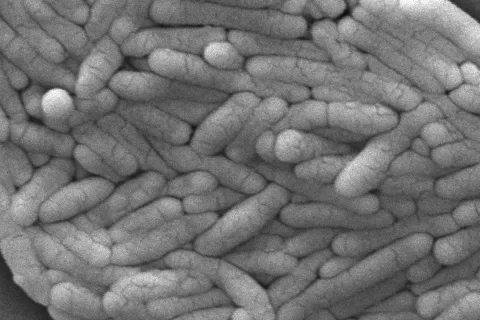
Eschar is a distinctive skin lesion that is commonly associated with rickettsial infections, particularly scrub typhus and spotted fever rickettsioses. Caused by the introduction of rickettsial pathogens through tick and mite bites, these lesions are integral to the clinical diagnosis of these conditions. Typically appearing a few days post-bite, eschars evolve from initial papules into more complex ulcerative lesions, which often have a characteristic brown-black crust and are surrounded by redness. The presence and manifestation of an eschar can greatly aid healthcare professionals in identifying the underlying rickettsial infection and initiating appropriate treatment.
The evolution of eschar involves not only the local response to the rickettsial invasion but also systemic responses that can complicate the clinical picture. Diagnostically, recognizing these skin lesions is pivotal. For instance, the eschar’s location and appearance provide clues about the route of infection through tick or mite bites. Understanding the dynamics of eschar development can help in differentiating between rickettsial infections and other conditions that may also present with similar cutaneous lesions.
The Role of Eschar in Diagnosing Scrub Typhus
Eschar plays a crucial role in diagnosing scrub typhus, a rickettsial infection marked by its characteristic symptoms and skin manifestations. The presence of an eschar often coincides with the incubation period of scrub typhus, making it a noteworthy clinical indicator. In late-stage scrub typhus, eschars may be less pronounced due to other systemic symptoms, but early identification can provide an opportunity for timely intervention. Additionally, utilizing PCR techniques to analyze the eschar can deliver a rapid and accurate diagnosis, significantly impacting patient management.
In some cases, the diagnosis might be complicated by the appearance of atypical eschars, which can resemble more common skin conditions such as acne. This overlap underscores the necessity for clinicians to maintain a high index of suspicion for rickettsial infections when confronted with superficial skin lesions. By understanding the variations in eschar presentation and taking into account the history of tick bites, healthcare providers can improve their diagnostic accuracy and ultimately enhance patient outcomes.
Clinical Characteristics of Eschar and Its Healing Process
Clinically, eschars present as relatively painless and non-itchy lesions, which can lead to their underrecognition, particularly among individuals with darker skin tones. Initially, the eschar may appear as a minor papule before developing into a central ulcer with a regulated healing process. Following the resolution of a rickettsial infection, it is not uncommon for patients to be left with small depressed scars that serve as reminders of their illness. Observing the changes that occur during healing can also provide important clues regarding the severity and progression of the infection.
The healing process of an eschar can vary significantly depending on various factors, including individual healing responses and the overall health of the patient. Notably, eschars associated with rickettsial infections can take several weeks to heal completely, and complications may arise if secondary infections occur. Monitoring the healing stage is essential to ensure that recovery is proceeding without any adverse developments, making periodic examinations valuable in the management of patients with known rickettsial infections.
Eschar Locations: A Guide to Rickettsial Infections
The location of eschars on the body can provide critical diagnostic insights into the type of rickettsial infection present. For instance, eschars resulting from tick bites typically emerge on extremities and the trunk, while mite-associated eschars may be found in areas where skin-to-skin contact or clothing friction occurs. Such knowledge can be vital in guiding comprehensive examinations and understanding potential exposure history, particularly in regions endemic to specific rickettsial species.
In considering locations, it is also important to recognize the overlap with eschars resulting from other infections, such as tularemia or leishmaniasis, which may compound diagnostic challenges. Distinguishing between these conditions relies heavily on clinical acumen and a thorough understanding of the various infection vectors and their associated eschar characteristics.
The Historical Context of the Term Eschar
The term ‘eschar’ has its origins in ancient Greek, derived from ‘eskhára’, which translates to hearth or scab. This etymological background reflects the long-standing association of eschars with healing processes following injury or infection. Over centuries, the word has evolved, passing through Middle French and Late Latin, where it consistently retained meaning related to scarring and skin lesions. This historical context underscores the significance of eschars in dermatological pathology.
Understanding the etymology of eschar can enhance a clinician’s appreciation for the lesion’s clinical implications. By recognizing the historical roots of the term and its evolving definition through different languages, healthcare practitioners can better contextualize eschars within broader discussions on skin health and infectious disease management. This also highlights the connection between early medical observations and contemporary advancements in diagnosing and treating rickettsial infections.
Diagnostic Techniques Involving Eschar in Rickettsial Infections
Modern diagnostic techniques for rickettsial infections often involve direct analysis of eschar tissue. PCR detection of pathogen DNA offers a rapid and accurate means of confirming diagnoses, particularly in the early stages of infection when other clinical manifestations might not yet be apparent. By extracting samples directly from the eschar, healthcare professionals can bypass some of the limitations of traditional serologic testing and provide more immediate results, guiding timely and effective treatment.
Utilizing eschar in the diagnostic process not only informs practitioners of the presence of specific pathogens but also enhances their understanding of rickettsial transmission dynamics. Clinical specimens obtained from eschars can reveal information about the prevalence of different rickettsial species in a given region. This knowledge can inform public health strategies aimed at controlling rickettsial infections and improving patient care through increased awareness and targeted interventions.
Skin Lesions as Indicators of Rickettsial Infection
Skin lesions, particularly those categorized as eschars, serve as vital indicators for diagnosing rickettsial infections. The clinical presentation of these lesions is often distinctive, evolving through specific stages that can significantly aid healthcare professionals in making an accurate diagnosis. Due to their local origin related to tick or mite bites, eschars provide a direct link to potential exposure, thereby enhancing the clinical inquiry necessary for effective treatment.
In summary, eschars are not just incidental findings; they are critical signs that inform the entire clinical approach to rickettsial infections. Awareness of the possible variations in eschar presentation, their locations, and associated symptoms are essential for primary care physicians and specialists alike. Enhanced education about the critical role of skin lesions can lead to better patient outcomes, reduced morbidity, and effective management of rickettsial diseases.
Implications of Misdiagnosing Eschar-Related Conditions
Misdiagnosing a condition involving eschar can have serious implications for patient management and outcomes. Given that eschars can resemble lesions from various other infectious diseases such as leishmaniasis or tularemia, healthcare providers must be vigilant in distinguishing these conditions. An erroneous diagnosis could lead to inappropriate treatment, prolonged illness, and even complicate the patient’s clinical pathway if required treatments for the rickettsial infection are not initiated.
Furthermore, failure to recognize eschars, especially in patients with darker skin tones, poses significant risks, as these lesions may go unnoticed and untreated. This necessitates greater awareness and training for healthcare providers to ensure timely and accurate diagnoses. Incorporating knowledge of eschar-related conditions into broader educational frameworks is crucial for managing rickettsial disease effectively, and ultimately enhancing patient care.
Future Directions in Eschar Research and Rickettsial Pathology
Future research in the domain of eschar pathology related to rickettsial infections holds promise for improving clinical outcomes. Ongoing studies into the molecular mechanisms underlying eschar formation may yield insights into the pathophysiology of rickettsial infections. Advances in genetic and genomic techniques can aid in characterizing various strains of rickettsia, as well as their unique interactions with host tissues during infection.
Moreover, the role of eschars in community health initiatives cannot be overstated. By integrating findings from eschar research into public health messaging, health practitioners can better inform communities about the risks of tick and mite exposure, thereby reducing infection rates. Focused education programs that highlight the importance of recognizing eschars can empower communities to seek timely medical attention, ultimately lowering the burden of rickettsial diseases.
Frequently Asked Questions
What is an eschar in relation to rickettsial infections?
Eschar is a distinctive skin lesion that occurs due to rickettsial infections, particularly from tick or mite bites. These lesions are crucial for diagnosing conditions like scrub typhus and spotted fever rickettsioses, typically developing at the site where the rickettsial pathogens enter the skin.
How do eschars develop after tick bites?
Following a tick bite, eschars usually emerge within a few days, corresponding to the incubation period of the rickettsial infection. The eschar initially appears as a small papule and evolves into a central ulcer covered by a brown-black crust, signaling tissue necrosis due to the growth of the rickettsial pathogen.
How can the diagnosis of eschar assist in identifying scrub typhus?
The presence of an eschar is a key diagnostic feature of scrub typhus. Medical professionals can utilize PCR methods to detect rickettsial DNA from eschar tissue or swabs, facilitating quick diagnosis and treatment of the infection.
Where do eschars typically appear from mite-associated rickettsioses?
In cases of mite-associated rickettsioses, eschars commonly develop in areas where skin contacts skin or clothing, such as the axilla, groin, neck, and waist. Less frequently, they may occur at the wrist or elbow joints.
What characteristics define a rickettsial eschar?
Rickettsial eschars are usually painless, non-itchy lesions ranging from 0.5 to 3.0 cm. They typically evolve from a papule to a central ulcer, surrounded by a red halo, and may take weeks to heal, sometimes leaving a small scar.
Can eschars vary in appearance among different patients?
Yes, eschars can vary significantly among patients. Those with darker complexions may overlook the lesions, resulting in delays in diagnosis. Occasionally, atypical eschars may resemble acne, complicating the recognition of rickettsial infections.
What other infectious diseases can present with eschars?
Eschar-like lesions can also occur in various infectious diseases, including tularemia, leishmaniasis, anthrax, and certain mycobacterial and fungal infections. These similarities necessitate careful differential diagnosis when evaluating skin lesions.
Is there a specific timeframe for eschar healing?
The healing time for rickettsial eschars can be several weeks, depending on individual patient factors and treatment. It is important for patients to seek medical attention if they notice such lesions, especially after known tick exposures.
What historical context does the term eschar have?
The term eschar is derived from Ancient Greek ‘eskhára,’ evolved through Latin and Middle French, illustrating its historical connections to healing and skin scabs. This reflects the physical nature of eschars as scabs formed from skin lesions.
What is the role of PCR in the diagnosis of eschar-associated rickettsial infections?
PCR (Polymerase Chain Reaction) is a rapid diagnostic method that allows for the identification of rickettsial DNA from eschar tissue or swab samples, helping doctors confirm a rickettsial infection early in its course.
| Key Points |
|---|
| Eschar refers to skin lesions caused by rickettsial infections from ticks or mites, crucial in diagnosing scrub typhus and spotted fever. |
| Eschar lesions typically appear within a few days after tick or mite bites and can take weeks to heal. |
| Rickettsial eschars are often painless and may be overlooked, especially in patients with darker skin. |
| PCR detection of the pathogen’s DNA from eschar samples serves as a rapid diagnostic method. |
| Eschar’s linguistic origin traces back to Ancient Greek, indicating a historical association with healing. |
Summary
Eschar is a critical term in understanding skin lesions associated with rickettsial infections. These lesions, often overlooked during early diagnosis, can be vital indicators of scrub typhus and spotted fever. Proper identification and rapid diagnostic approaches, such as PCR testing, can enhance the treatment process. With a rich historical etymology behind the term, eschars remain a significant aspect of clinical consideration in infectious disease.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.