DoxyPEP, a promising method of STI prevention through the use of doxycycline, has gained attention amid growing concerns about rising sexually transmitted infections (STIs) across various populations. Recent online surveys conducted in the Netherlands have highlighted a significant increase in informal doxycycline use among men who have sex with men, transgender individuals, and gender-diverse people, with 22.5% having used doxyPEP/PrEP. As individuals seek greater autonomy in their sexual health decisions, the current lack of official doxycycline guidelines raises critical questions about safety and antimicrobial resistance. The rise of doxyPEP use reflects changing attitudes toward STI prevention and the pressing need for healthcare providers to adapt to these emerging trends. Concurrently, it underscores the importance of balanced information regarding effective doxycycline use to safeguard public health.
The concept of doxyPEP, or doxycycline prophylaxis, serves as a vital intervention for sexually active individuals looking to reduce the risk of STIs. As STI rates continue to escalate, alternative preventive measures such as PrEP for STIs are becoming increasingly relevant, especially among high-risk groups. This trend highlights the urgency for healthcare professionals to establish comprehensive doxycycline guidelines that inform safer practices and mitigate potential issues surrounding antimicrobial resistance. Additionally, the informal adoption of doxycycline as a preventative measure shows a shift in public health dynamics, calling for enhanced monitoring and education to address user motivations and knowledge gaps. Such proactive measures will be crucial in navigating the balance between personal health empowerment and the overarching goal of preserving antibiotic efficacy.
The Emergence of doxyPEP: A New Approach to STI Prevention
The rise of doxycycline post-exposure prophylaxis, commonly known as doxyPEP, represents a significant shift in the strategy for preventing sexually transmitted infections (STIs) among high-risk populations, such as men who have sex with men (MSM) and transgender individuals. Recent surveys in the Netherlands have indicated that a notable percentage of these individuals are turning to doxyPEP as a proactive measure against STIs, despite the lack of formal guidelines or endorsement from health authorities. This trend underscores a pressing need for evidence-based guidelines and structured health policies that can inform users about the proper use and potential risks associated with doxycycline.
While doxyPEP has shown promising results in clinical trials for STI prevention, the informal usage seen in surveys raises concerns about antibiotic overuse and possible resistance development. As individuals seek out doxyPEP in the absence of official recommendations, public health officials face challenges in ensuring that users are informed, protected, and monitored effectively. The ongoing discussions around doxyPEP highlight the dynamic nature of sexual health practices and the need for responsive healthcare frameworks to address new trends in STI prevention.
Navigating the Guidelines for doxycycline Use
Despite Australia, Germany, and the United States establishing guidelines for prescribing doxyPEP, the Netherlands is notably absent from this list, leaving a gap in standardized healthcare practices. Current observations indicate that, without formal recommendations, many individuals are self-sourcing doxyPEP based on peer influences or personal research. This situation is concerning because it perpetuates the potential for misuse, leading to increased antibiotic consumption and contributing to the broader issue of antimicrobial resistance (AMR) within the community.
Moreover, the lack of guidelines can lead to confusion about eligibility, appropriate dosing, and the efficacy of doxyPEP in preventing STIs. As individuals turn to doxycycline without adequate supervision, the risk of inappropriate use escalates, threatening both individual health and public health. Establishing clear doxycycline guidelines that consider the unique needs of high-risk groups is critical to managing antibiotic use and ensuring effective STI prevention.
The Dangers of Antibiotic Overuse in STI Prevention
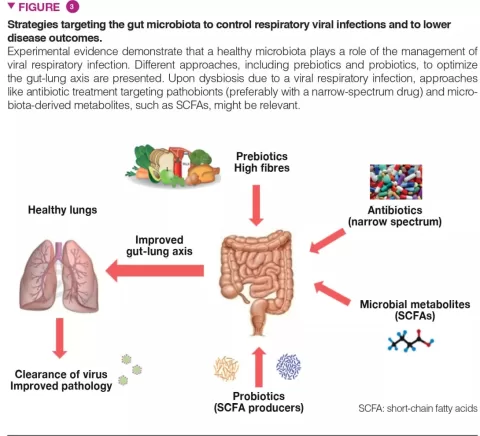
As the use of doxycycline for STI prophylaxis rises, health experts warn against the unintended consequences of antibiotic overuse. High rates of doxyPEP usage reported in recent surveys may increase the prevalence of antibiotic resistance in the population, particularly in communities where STIs are already on the rise. The relationship between frequent doxycycline use and the development of resistant bacterial strains is a significant concern for public health, as it could undermine the effectiveness of antibiotics in treating other infections.
Research has demonstrated that increasing tetracycline resistance genes in Neisseria gonorrhoeae bacteria can be traced back to doxyPEP usage, presenting a worrying scenario where standard treatments for gonorrhea and other bacterial infections may become less effective. These findings emphasize the importance of surveillance systems that track antibiotic resistance trends and guide the responsible use of doxyPEP in community settings.
Community Influence on the Rise of doxyPEP
The survey results indicating a high intention to use doxyPEP among participants illustrate the powerful role of community dynamics and peer influence in shaping health behaviors. Many respondents reported using doxyPEP based on recommendations from friends or broader community discussions about STI prevention strategies. This peer-driven approach to health poses both opportunities and risks, as individuals who feel encouraged to adopt doxyPEP may not have access to the necessary information regarding its safe and effective use.
To mitigate potential risks associated with the community-driven adoption of doxyPEP, healthcare professionals must engage with community members to provide accurate, relevant information. Collaborating with community groups to disseminate educational resources about STI protection, applicable guidelines, and the risks of antimicrobial resistance can empower individuals to make safer, well-informed decisions about their sexual health practices.
STI Prevention: The Need for Comprehensive Education
As reported in the survey, a significant percentage of respondents expressed a desire to use doxyPEP if it were formally recommended, shedding light on a gap in knowledge regarding STI prevention methods. Comprehensive education about STIs and antibiotic use should be at the forefront of public health strategies. Health authorities must work to clarify the role of doxycycline not only in preventing STIs but also in preventing the potential development of antibiotic resistance.
Engaging MSM and transgender communities in education initiatives will be crucial in shaping behavioral norms around doxyPEP use. These initiatives should focus on providing factual information about the effectiveness of doxyPEP, recommendations for responsible use, and the importance of regular STI testing, thereby creating a more informed public that is less susceptible to misinformation and peer pressure.
Long-term Implications of doxyPEP Usage
The rise in informal doxyPEP use raises several long-term implications for STI prevention strategies. The unchecked spread of doxycycline could challenge public health efforts to combat STIs, particularly if significant antibiotic resistance emerges as a result. Health decisions made in isolation from professional guidance might lead to unintended health complications, including prolonged infections that could have been easily treated with effective antibiotics, if they were still viable.
Moreover, the evolving landscape of STIs poses a need for continuous evaluation of prophylactic strategies like doxyPEP. Monitoring its adoption and addressing emerging resistance will be essential for developing robust public health responses that protect community health while promoting safe sexual practices.
Peer Networks and Their Role in Health Choices
The influence of peer networks on health choices, particularly in the context of doxyPEP, cannot be underestimated. The survey highlights that many individuals are inclined to try doxyPEP based on peer discussions, reflecting a broader trend where social circles significantly impact personal health decisions. Although peer support can encourage proactive health measures, it can also lead to the propagation of unverified information and potentially unsafe practices.
Thus, fostering a balance between community-driven motivations and professional health advice is critical. Educating peer leaders and influencers within these communities can lead to positive health outcomes, ensuring that individuals are better equipped to make informed choices about doxyPEP and STI prevention.
Assessing Peer Pressure vs. Health Outcomes
Peer pressure plays a dual role in the decision to use doxyPEP, influencing both positive and negative health outcomes among high-risk groups. While it has enabled increased awareness and motivation among individuals to protect themselves against STIs, it may also lead to premature adoption of doxyPEP without thorough understanding or guidance from healthcare providers. The nuances of this relationship need to be addressed, particularly in urban areas where sexual health communities are more vocal and influential.
Public health campaigns must consider the power of peer dynamics and leverage these networks to share supportive and factual information about doxyPEP. Such campaigns can foster an environment where individuals seek professional advice alongside community input, ultimately leading to safer practices regarding STI prevention.
Strategies for Effective Monitoring of doxyPEP Usage
Given the rising informal use of doxyPEP, active monitoring strategies must be implemented to assess its impact on public health. Without structured systems in place, it becomes increasingly difficult to understand patterns of usage and the associated risks of antimicrobial resistance. Researchers and healthcare providers need to collaborate to establish comprehensive tracking frameworks that can effectively measure both the uptake of doxyPEP and changes in resistance patterns amongst bacterial populations.
Creating a system for feedback from users of doxyPEP will provide invaluable data regarding their experiences, perceived effectiveness, and any adverse effects. Such insights could inform ongoing research and adaptations of public health recommendations, ensuring they align effectively with actual community practices and challenges.
Frequently Asked Questions
What is doxyPEP and how is it related to doxycycline use?
DoxyPEP refers to the use of doxycycline as post-exposure prophylaxis to prevent sexually transmitted infections (STIs), particularly in high-risk populations like men who have sex with men (MSM) and transgender individuals. Doxycycline use in this context is aimed at significantly reducing the incidence of STIs such as syphilis and chlamydia when taken shortly after unprotected sex.
What does current doxycycline guidelines say about STI prevention?
Currently, only a few countries like Australia, Germany, and the United States have established guidelines for administering doxycycline as prophylaxis against STIs (doxyPEP). In contrast, the Netherlands has determined that it is not recommended as they seek to prevent potential overuse and antimicrobial resistance.
How does doxyPEP function as a PrEP for STIs?
DoxyPEP functions as a Pre-Exposure Prophylaxis (PrEP) by providing a protective measure against STIs such as syphilis and gonorrhea when taken after unprotected sexual encounters. Its effectiveness has been demonstrated in high-risk groups, but formal guidelines and recommendations are still evolving.
What are the risks associated with doxycycline use for STI prevention?
The use of doxycycline for STI prevention poses risks, particularly concerning the development of antimicrobial resistance (AMR). Overuse could lead to increased antibiotic consumption and create resistant strains of bacteria, making it crucial to monitor and establish guidelines around doxyPEP.
Why is there concern about antimicrobial resistance in relation to doxyPEP?
Concerns about antimicrobial resistance arise due to the potential for significant increases in antibiotic consumption through doxyPEP use, which could lead to rising resistance levels in bacteria, including Neisseria gonorrhoeae. This poses risks for population-level antibiotic effectiveness and necessitates robust monitoring strategies.
What insights were gained from the recent survey on doxyPEP use in the Netherlands?
The recent survey revealed a substantial rise in informal use of doxyPEP, with 22.5% of respondents having used it, reflecting a significant increase from previous surveys. It highlighted user motivations focused on STI protection and perceived safety, indicating a growing informal demand for doxycycline as prophylaxis.
Is doxycycline the only antibiotic being used for STI prevention in informal settings?
No, the survey indicated that many respondents were using other antibiotics besides doxycycline for STI prevention, such as azithromycin and amoxicillin, none of which have been proven effective for this purpose, raising concerns about safety and effectiveness.
What role do peer recommendations play in the uptake of doxyPEP?
Peer recommendations significantly influence the uptake of doxyPEP, as many individuals reported being motivated to use it based on advice from their peers and community, underlining the importance of trusted voices in health decision-making and the need for accurate public health messaging.
What measures are suggested to address the challenges associated with doxyPEP?
To address challenges associated with doxyPEP, there is a call for developing formal guidelines on its use, alongside monitoring systems to track usage patterns and antimicrobial resistance. Implementing community-based education can help promote informed and safe choices regarding doxycycline use.
What steps are needed to ensure safe use of doxyPEP among sexually active individuals?
To ensure safe use of doxyPEP among sexually active individuals, healthcare providers must establish clear guidelines, promote awareness about potential risks such as antimicrobial resistance, and foster community engagement for safer health practices.
| Key Points | Details |
|---|---|
| Increase in doxyPEP/PrEP Use | 22.5% of 1,633 surveyed MSM, transgender, and gender-diverse individuals reported ever using doxyPEP/PrEP. |
| Recent Usage | 15% reported recent use of doxyPEP/PrEP, with 65% intending to use it if available. |
| Lack of Guidance | Not recommended in the Netherlands; guidelines only exist in Australia, Germany, and the USA. |
| Potential Risks | Increased antibiotic use could lead to antimicrobial resistance and alter gut microbiome. |
| Community Influence | Peer recommendations and community discussions heavily influence the decision to use doxyPEP/PrEP. |
| Need for Monitoring | Survey highlights need for guidelines, monitoring, and regulation of doxyPEP/PrEP use. |
Summary
doxyPEP is witnessing a significant rise in informal usage in the Netherlands despite its absence in formal medical guidelines. A recent survey shows that a notable percentage of men who have sex with men, transgender individuals, and gender-diverse communities are using doxycycline for STI prevention. This trend calls for immediate action from health authorities to establish formal guidelines and monitoring systems to safeguard public health and mitigate potential risks associated with increased antibiotic use.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.