Disseminated histoplasmosis is a severe fungal infection that poses a critical risk to individuals with advanced HIV, particularly in areas like France and its overseas territories. This condition often goes unrecognized, leading to delayed treatment and worse health outcomes for patients. Studies indicate that the incidence of histoplasmosis is notably high among the HIV population, emphasizing the need for awareness and timely diagnosis of this disease. Not only does disseminated histoplasmosis challenge existing healthcare protocols, but it also highlights the intersection of HIV and fungal infections as a growing public health concern. Understanding the epidemiology of histoplasmosis in populations living with HIV can significantly inform treatment strategies and public health policies, particularly in endemic regions.
Disseminated mycosis, commonly known as disseminated histoplasmosis, manifests as a serious health challenge for people coping with advanced immunocompromising conditions such as HIV. This severe fungal infection frequently masquerades as other illnesses, complicating the diagnosis and leading to late treatment initiation. Recent data has shed light on the alarming rates of disseminated fungal infections among individuals living with HIV, particularly in various geographic regions. As histoplasmosis cases continue to rise in certain territories, this emphasizes the dire need for improved global health strategies to combat the implications of HIV on fungal disease prevalence. Elevated awareness and better diagnostic practices are crucial in addressing this intersection between viral and fungal infections.
Understanding Disseminated Histoplasmosis and its Link to HIV
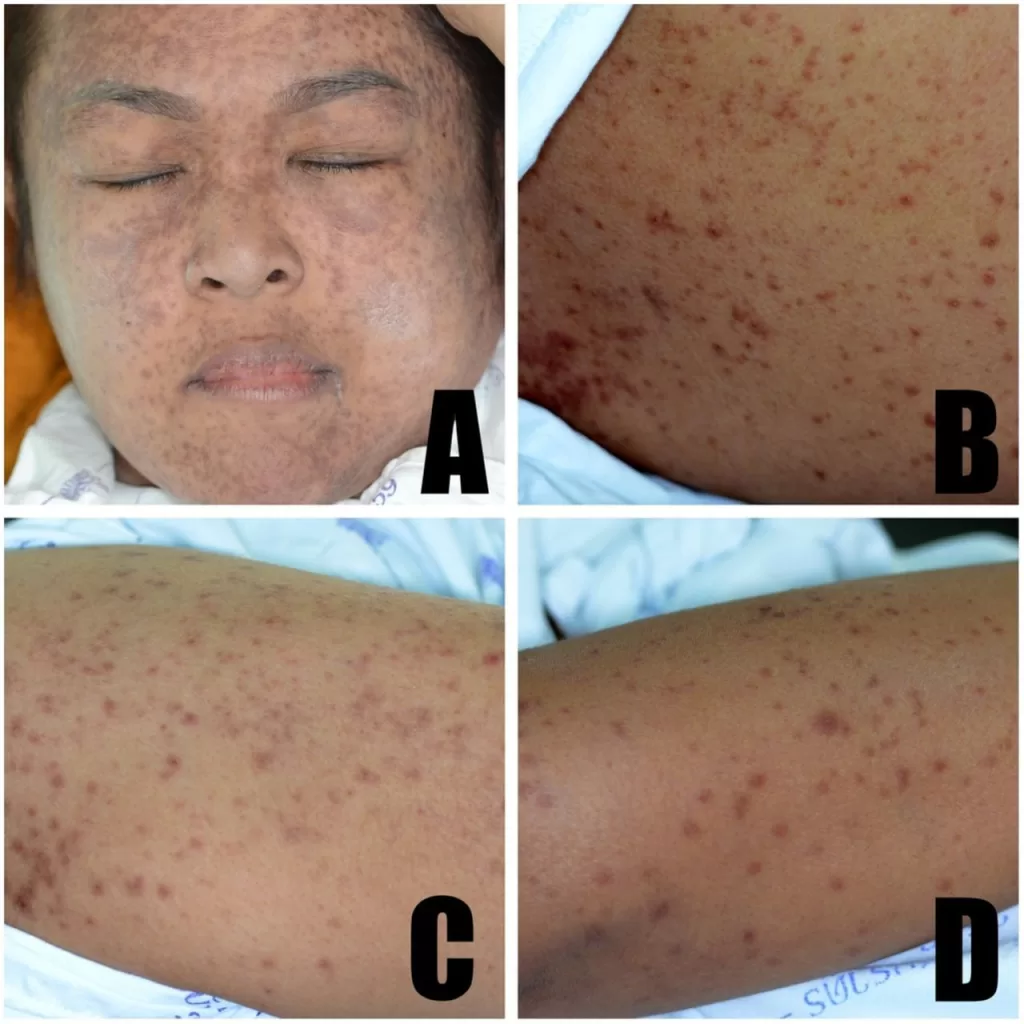
Disseminated histoplasmosis is a severe fungal infection that poses a significant threat to individuals living with HIV, particularly those with advanced stages of the virus. This condition occurs when the Histoplasma capsulatum fungus, typically found in soil and bird droppings, spreads throughout the body. In patients with HIV, the immune system has a reduced capacity to combat such infections, leading to an increased risk of developing disseminated histoplasmosis. The challenge in diagnosing this condition lies in its similarity to other diseases, often resulting in misdiagnosis and delayed treatment, which can exacerbate health outcomes.
The incidence of disseminated histoplasmosis among HIV-positive individuals has been notably documented in various regions, especially in the Americas. Recent studies highlight a concerning trend: while advancements in HIV treatment have reduced the incidence and related mortality rates, the disease still remains a pressing health concern in certain endemic areas. Specifically, regions such as French Guiana exhibit much higher incidence rates compared to metropolitan France, indicating that geographic and demographic factors play crucial roles in the epidemiology of this fungal infection.
Frequently Asked Questions
What is disseminated histoplasmosis and how does it relate to HIV?
Disseminated histoplasmosis is a severe form of histoplasmosis, a fungal infection caused by the Histoplasma capsulatum organism. It is particularly dangerous for individuals with advanced HIV infection, as their compromised immune systems can lead to a higher incidence of disseminated fungal infections. The connection between HIV and fungal infections like disseminated histoplasmosis highlights the need for timely diagnosis and treatment in vulnerable populations.
What are the incidence rates of disseminated histoplasmosis in HIV-positive individuals in France?
According to a study analyzing the French hospital database, the incidence rate of disseminated histoplasmosis among HIV-positive individuals in France from 1992 to 2021 was 2.8 cases per 1,000 person-years. This figure varied significantly across regions, demonstrating a higher incidence in places like French Guiana compared to mainland France.
How does HIV treatment in France impact the incidence of disseminated histoplasmosis?
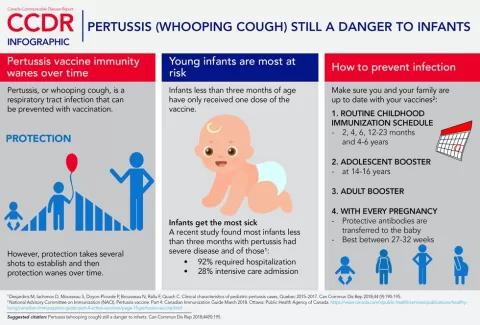
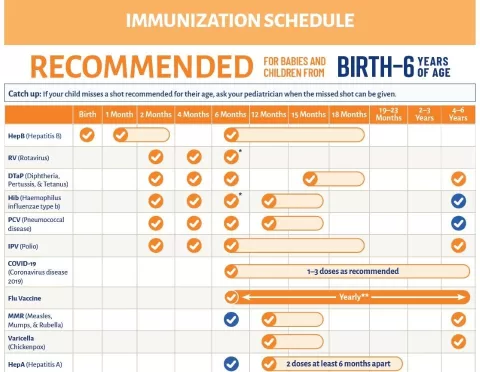
HIV treatment in France, particularly the implementation of antiretroviral therapies, has significantly reduced the incidence and mortality rates associated with disseminated histoplasmosis. The improved management of HIV leads to better immune function, which helps in lowering the risk of developing disseminated fungal infections.
What regions have the highest prevalence of disseminated histoplasmosis in HIV patients?
Regions like French Guiana have notably higher prevalence rates of disseminated histoplasmosis among HIV patients, with an incidence rate of 9.41 cases per 1,000 person-years. This is significantly higher than rates found in mainland France, demonstrating the need for targeted public health initiatives in endemic areas.
What challenges exist in diagnosing disseminated histoplasmosis in HIV patients?
Diagnosing disseminated histoplasmosis in HIV patients presents significant challenges, primarily due to misdiagnosis and underreporting. Lack of awareness and diagnostic resources, especially in endemic regions like sub-Saharan Africa and Asia, complicates timely treatment for patients at risk of severe outcomes from this fungal infection.
Why is ongoing surveillance of disseminated histoplasmosis important for persons living with HIV?
Ongoing surveillance of disseminated histoplasmosis is crucial as it helps public health officials monitor trends, identify outbreaks, and improve diagnostic methods. Given the link between advanced HIV disease and increased susceptibility to this and other fungal infections, enhancing awareness and medical capabilities can significantly improve outcomes for affected individuals.
What can be done to improve the management of disseminated histoplasmosis in HIV-positive patients?
To improve the management of disseminated histoplasmosis in HIV-positive patients, it is essential to enhance diagnostic capabilities, increase awareness among healthcare providers, and ensure access to effective antifungal treatments. Additionally, ongoing education on the epidemiology of histoplasmosis and its relationship with HIV can empower providers to recognize and treat cases more effectively.
| Key Point | Details |
|---|---|
| Health Threat | Significant risk for individuals with advanced HIV, especially in certain regions. |
| Study Cohort | Involved 198,798 HIV-positive individuals in France and overseas territories between 1992-2021. |
| Incidence Rate | Overall rate of 2.8 cases per 1,000 person-years with regional variations. |
| Regional Disparities | Highest in French Guiana (9.41), low in mainland France (0.079). |
| Trends Over Time | Decline in both incidence and mortality rates due to improved HIV treatments. |
| Diagnostic Challenges | Misdiagnosis and underreporting are significant issues, especially in endemic regions. |
| Epidemiological Trends | Data over three decades indicate positive impacts of treatment innovations. |
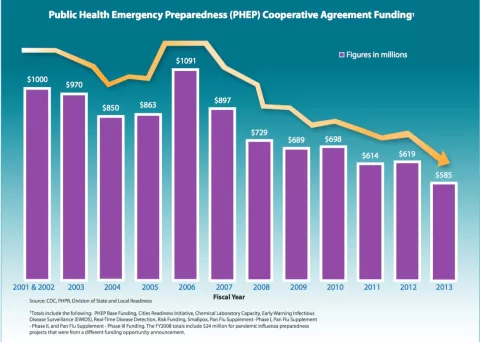
| Public Health Implications | Need for ongoing surveillance and improved diagnostic capabilities. |
Summary
Disseminated histoplasmosis remains a crucial health concern, particularly among individuals living with HIV. Despite the decline in incidence and mortality rates due to advancements in treatment, there is a pressing need for enhanced diagnostic resources and awareness, especially in endemic areas. This study emphasizes the importance of continued vigilance and proactive public health measures to effectively combat this disease.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.