Current flu activity has shown a notable decline across the nation, with influenza-like illness (ILI) rates dropping significantly last week. According to the latest CDC flu update, while flu hospitalization rates have decreased, there has been an alarming rise in influenza deaths among children, reaching 204 this season. Hospitalization figures indicate a reduction from 4,639 to 3,601 patients, signaling improved outcomes for many. Despite this positive trend, one state’s high ILI activity—specifically Rhode Island—remains a concern for health officials. In light of these developments, it’s crucial for the public to remain aware of the ongoing risks posed by influenza and to stay informed about COVID-19 levels, which currently remain low but warrant continued vigilance.
As we navigate through this season, the landscape of respiratory illnesses—especially the flu—continues to evolve. Reports indicate a steady decline in the prevalence of influenza-related complications, yet serious concerns still linger due to pediatric fatalities. Efforts to monitor not just flu but also other respiratory infections, such as COVID-19, are paramount in our public health strategy. Vaccination and proactive health measures remain vital, especially given the rising hospitalization rates associated with some strains of the virus. Understanding the interplay between these illnesses can empower communities and individuals alike to take informed actions in safeguarding their health.
Current Flu Activity Analysis
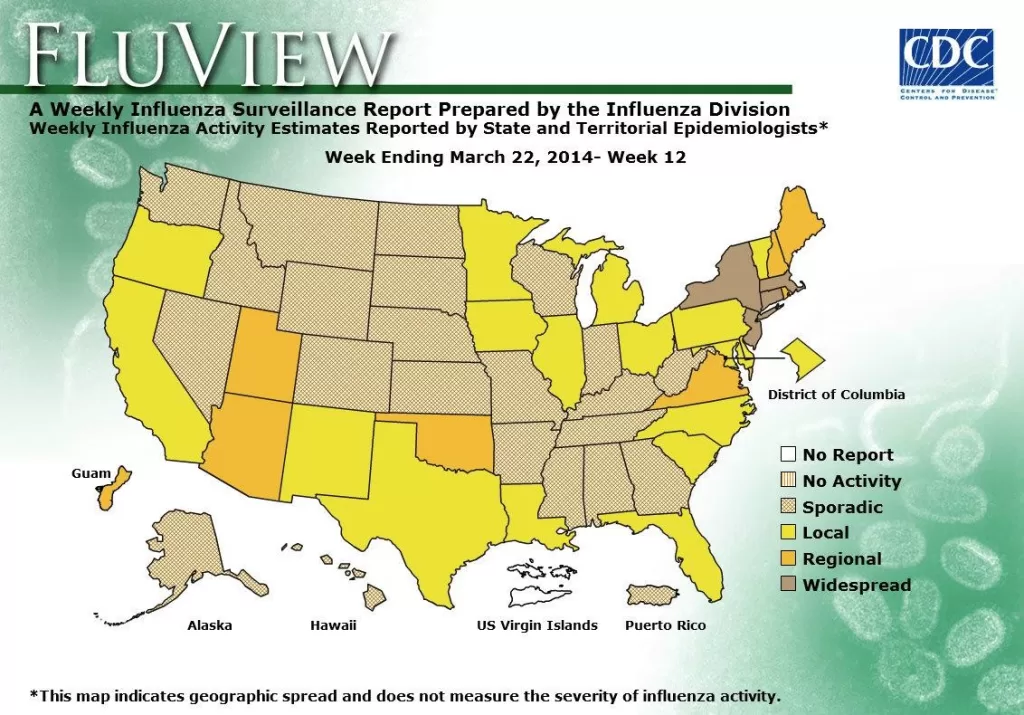
Flu activity across the United States has shown a significant decrease, with the rate of influenza-like illness (ILI) dropping to 2.3% last week, a slight dip from 2.4% the previous week. This positive trend in flu activity is encouraging as health officials monitor seasonal patterns, noting that only Rhode Island reported high ILI activity, while other states showed a much lower incidence of flu cases. The decrease in flu cases correlates with a decline in flu hospitalization rates, which fell from over 4,600 to 3,600 hospitalizations within a week.
Despite the overall drop in flu activity, the Centers for Disease Control and Prevention (CDC) reported a troubling rise in flu-related deaths among children, with 204 fatalities this season, just shy of last year’s total of 207. Pediatric deaths from influenza A have been particularly concerning, emphasizing the importance of vaccination and preventive measures to protect vulnerable populations. Monitoring these statistics is crucial, not just for immediate health implications but also for understanding the long-term impacts of flu seasons in relation to public health.
Influenza Hospitalization Rates: A Concerning Trend Amidst Declining Flu Cases
The current flu season has presented a stark contrast between a decline in active cases and an alarming peak in hospitalization rates. With the cumulative hospitalization rate at 126.6 per 100,000 population, this season’s figures are the highest observed since the 2010-11 flu season. Although the hospitalization rates are starting to decline, it remains critical to ensure that healthcare resources are sufficient to handle the fluctuating patient needs during flu peaks. The statistics also remind us of the seriousness of influenza, even when flu activity is labeled as diminishing.
Furthermore, as flu rates decline, health professionals emphasize the necessity for continued vigilance against respiratory illnesses. The recent statistics regarding flu hospitalization rates underscore the harsh reality that the flu virus can still lead to severe outcomes, particularly in high-risk groups, emphasizing the importance of prompt medical intervention. Increased awareness about flu and its potential complications can help reduce the overall burden during a challenging flu season.
Influenza Deaths and Pediatric Vulnerability
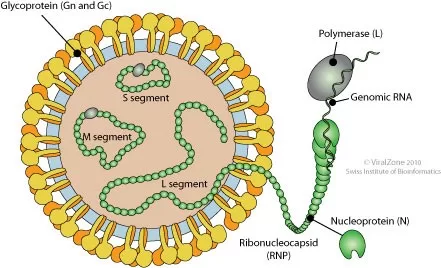
Amid declining flu activity, the reported rise in pediatric flu deaths remains a concern for health officials. As of last week, pediatric deaths have reached 204, marking a worrisome increase among children who are particularly vulnerable to complications from the disease. Influenza A was attributed to most of these deaths, specifically the H1N1 strain, which highlights the variations in flu strains present this season. Health professionals stress the importance of vaccination not just for children but as a community-wide strategy to combat the flu’s spread.
The unfortunate reality of these death statistics underscores the critical role of the CDC in disseminating information and coordinating responses to seasonal flu outbreaks. The rise in pediatric deaths serves as a grim reminder of the need for parents and guardians to stay informed about vaccination schedules and signs of severe flu illness among children. By fostering awareness and encouraging proactive health measures, communities can work together to reduce the incidence of severe cases and ultimately save lives.
The Decline of Hospitalization Rates as a Positive Sign Amidst Influenza Threats
While flu-related deaths are regrettably on the rise among children, it’s essential to highlight the significant decline in hospitalization rates observed over the past weeks. With a drop from 4,639 hospitalizations to 3,601, the overall projection offers a glimmer of hope amidst a challenging flu season. Decreased hospitalization rates could be attributed to increased vaccine uptake and public health campaigns emphasizing prevention.
Healthcare systems are continuing to adapt in light of both the flu and other respiratory viruses like COVID-19. Although COVID-19 levels remain consistently low, it’s pivotal to remind the public that flu season can still lead to severe outbreaks if not managed correctly. Reducing hospitalization rates remains a priority, as preventative measures, including vaccination against both flu and COVID-19, play a critical role in contributing to healthier communities during flu season.
Impact of COVID-19 on Flu Statistics
As flu activity diminishes, it is essential to consider the impact of COVID-19 on flu statistics and public health responses. Current reports indicate that COVID-19 levels remain consistently low, with a death rate of 0.7% compared to 0.3% for flu in the past week. This data not only highlights the importance of ongoing public health initiatives but also raises questions on how COVID-19 has influenced the patterns and responses to seasonal influenza. Increased public health measures for COVID-19 may have inadvertently contributed to the decrease in flu activity.
However, it’s crucial to maintain vigilance as residual effects from the pandemic persist. The CDC’s updates about test positivity rates for flu and COVID-19 reveal a subtle balance in managing both respiratory illnesses. As flu positivity rates decrease to 5.6%, understanding the interplay between COVID-19 and influenza is essential in developing effective strategies for flu seasons, keeping in mind that similar prevention strategies can benefit both diseases.
Wastewater Surveillance: A Tool for Monitoring Flu and COVID-19 Trends
One of the emerging techniques in tracking disease spread, such as flu and COVID-19, is wastewater surveillance. Recent findings show low wastewater levels for both influenza A and COVID-19, with some localized spikes in states like Louisiana. This type of monitoring is becoming increasingly vital for accurate public health forecasting and proactive responses. Studies reflect that consistent tracking through wastewater can provide early warnings of rising flu activity or potential outbreaks, shaping responses before they escalate.
Effective wastewater tracking can allow health authorities to allocate resources efficiently, streamline public health responses, and inform community strategies. As influenza and COVID-19 continue to co-circulate, understanding the dynamics through tools like wastewater surveillance can aid significantly in early identification of trends influencing flu hospitalization rates and overall public health initiatives.
Frequently Asked Questions
What is the current flu activity as reported by the CDC?
According to the CDC’s latest update, flu activity continues to diminish nationwide, with a decline in influenza-like illness (ILI) cases. This week, the percentage of outpatient visits for ILI decreased slightly from 2.4% to 2.3%. The flu hospitalization rates also fell significantly from 4,639 to 3,601 patients.
How many influenza-related deaths have occurred this season?
As of the most recent CDC update, there have been 204 reported influenza-related deaths among children this season, which reflects an increase of 6 from the previous week. These figures indicate a concerning trend but also highlight the importance of monitoring flu activity.
What does the CDC say about flu hospitalization rates?
The CDC reports that flu hospitalization rates have decreased, with the total dropping to 3,601 from 4,639 in the previous week. Nonetheless, the cumulative hospitalization rate of 126.6 patients per 100,000 population is the highest since the 2010-11 season.
What is the test positivity rate for flu this week?
This week, the test positivity rate for flu activity has decreased to 5.6%, down from 6.7% the prior week. This drop reflects the ongoing decline in flu cases nationwide, as reported in the CDC’s flu activity update.
How does current flu activity compare to COVID-19 levels?
According to the CDC, while flu activity is decreasing, COVID-19 levels remain low, with a steady death rate of 0.7%. The latest data indicates low levels of wastewater detections for COVID-19 and influenza A, suggesting a lower risk of severe outbreaks from these viruses at this time.
What are the recent trends in pediatric flu deaths?
The CDC has reported a total of 204 pediatric deaths due to influenza this season, just shy of the 207 deaths reported last season. The rise in deaths this week, with five attributed to influenza A and one to influenza B, highlights the ongoing risks associated with current flu activity.
Which state reported the highest flu-like illness activity?
Currently, only Rhode Island is reporting high influenza-like illness (ILI) activity, according to the CDC’s latest weekly update. This remains unchanged from the previous week, while other states have shown decreased flu activity levels.
What should I know about influenza vaccination during this flu season?
Considering the current flu activity and the reported increase in deaths, the CDC recommends getting the influenza vaccine if you have not yet done so. Vaccination is key in mitigating flu-related complications, especially for vulnerable populations.
How do test positivity rates for flu and RSV compare to COVID-19?
The latest CDC data shows that the test positivity rate for flu is 5.6% and for RSV it is 2.4%, indicating a decrease in both. Meanwhile, the COVID-19 positivity rate remains steady at 3.4%, highlighting shifts in respiratory illness trends.
Is it safe to attend gatherings during the current flu activity?
While flu activity is decreasing, it is still recommended to take precautions during gatherings, such as vaccination and good hygiene practices, especially considering the recent increase in pediatric deaths due to influenza as reported by the CDC.
| Key Point | Details |
|---|---|
| Current Flu Activity | Flu activity is diminishing nationwide, with a decrease in outpatient visits and hospitalization rates. |
| Flu Deaths | Pediatric flu-related deaths rose to 204, up 6 from the previous week. |
| Hospitalizations | Hospitalizations dropped from 4,639 to 3,601. |
| ILI Rates | Influenza-like illness (ILI) visits decreased from 2.4% to 2.3%. |
| States Reporting Activity | Only Rhode Island reported high ILI activity. |
| Test Positivity Rate | Flu test positivity rate decreased to 5.6%, down from 6.7%. |
Summary
Current flu activity shows a continued decline across the United States, although there remains a significant concern with pediatric flu-related deaths which have increased to 204 this season. While hospitalization rates have dropped, it’s crucial for the public to stay vigilant as trends become more favorable. The ongoing monitoring by health authorities indicates an overall positive shift, but attention to flu prevention remains essential.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.