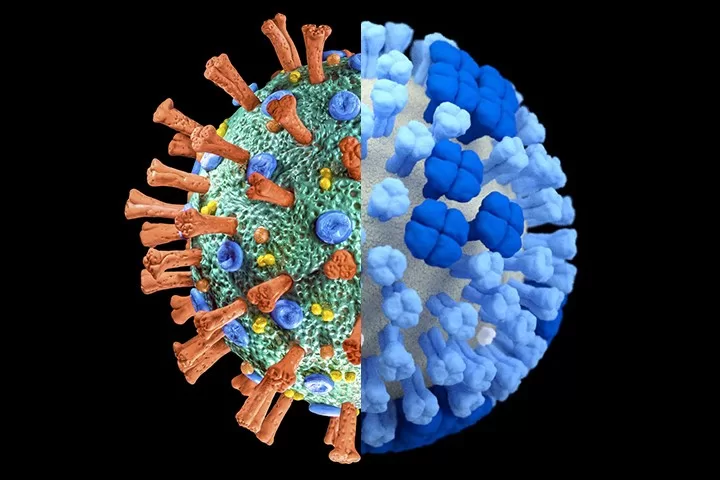
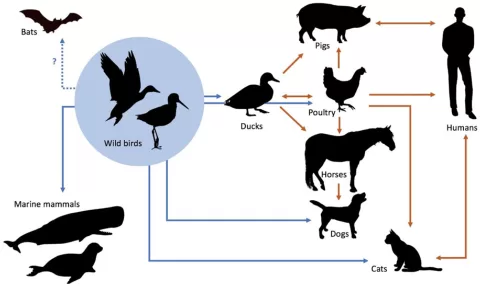
COVID-flu coinfection, which occurs when an individual contracts both COVID-19 and influenza simultaneously, has emerged as a significant health concern, particularly with a global prevalence estimated at 14%. Studies indicate that this viral co-infection can lead to severe respiratory complications, exacerbating existing symptoms and increasing hospitalization risk. Regions such as Asia and Europe have reported higher rates of influenza A and B coinfections, complicating treatment protocols. As the COVID-19 flu prevalence continues to be monitored, understanding the dynamics of these co-infections becomes imperative for healthcare responses. Proper vaccination and treatment strategies are essential to mitigate the impacts of such viral interplays.
The co-occurrence of COVID-19 and influenza infections, often referred to as viral co-infection or dual infection, poses notable challenges for both patients and healthcare systems. This phenomenon, where two respiratory viruses simultaneously infect an individual, necessitates a deeper exploration of the implications for clinical management. With rising cases of COVID-19 flu interactions, health professionals are increasingly focusing on the complexities of diagnosing and treating these patients. By emphasizing the importance of preventive measures, such as vaccination against seasonal flu and SARS-CoV-2, we can better address the issues associated with these co-infections. As research continues to evolve, understanding the nuances of influenza A/B and COVID-19 co-prevalence will be crucial in shaping effective public health strategies.
Understanding COVID-Flu Coinfection Rates
Recent research has identified a global prevalence rate of 14% for COVID-flu coinfection, indicating that millions are affected worldwide. This meta-analysis highlights distinguishable rates across geographical regions, with Asia and Europe reporting the highest incidences of influenza A/B alongside COVID-19. This dual infection can manifest severe respiratory symptoms, putting patients at risk of exacerbations and leading to increased hospitalization rates, particularly among vulnerable populations.
The shared symptoms between COVID-19 and influenza complicate clinical diagnosis, often leading to misinterpretations of patient conditions. Doctors and healthcare professionals must remain vigilant to differentiate between these overlapping viral infections to ensure proper treatment protocols are followed. The implications of COVID-19 influenza A/B coinfection are profound, necessitating further studies to understand its impacts on public health and healthcare systems.
The Importance of Vaccination Against COVID-19 and Influenza
Vaccination has been emphasized as a crucial strategy in the prevention of COVID-flu coinfection. High vaccination rates for both seasonal influenza and SARS-CoV-2 are correlated with reduced rates of coinfection, as noted by recent meta-analysis findings. As dual infections can worsen health outcomes, achieving widespread immunization can serve as a protective factor, especially in high-risk groups like the elderly or those with preexisting health conditions.
Post-vaccination monitoring and continued public health campaigns promote vaccine uptake, thereby lowering the prevalence of both COVID-19 and influenza viruses. Educating the public about the benefits of vaccination can diminish the burden of these infections and improve overall outcomes, reinforcing the importance of preparedness during seasonal outbreaks and pandemic scenarios.
Impact of COVID-19 Hospitalization Risks
Hospitalization risks associated with COVID-19 coinfection with influenza strains have raised alarming concerns among healthcare providers. The combination of these viral infections can lead to more severe respiratory complications, such as pneumonia and acute respiratory distress syndrome (ARDS). The increased hospitalization rate among affected individuals is primarily due to the inability of the immune system to cope with two pathogens attacking simultaneously, leading to worsened clinical outcomes.
Understanding the hospitalization risks tied to COVID-19 influenza A/B coinfection is essential for crafting effective healthcare responses. Healthcare systems need to prepare for potential surges in hospital admissions related to these viruses, adapting protocols for rapidly identifying and treating coinfected patients to mitigate the impact on resources and improve patient care.
Challenges in Diagnosing Viral Coinfections
Diagnosing COVID-19 and influenza A/B coinfections presents considerable challenges for healthcare practitioners. The overlap in symptomatology can lead to diagnostic confusion, as both viruses can produce similar clinical presentations. Moreover, existing diagnostic tests may not always differentiate clearly between COVID-19 and flu infections, complicating treatment considerations and prompting potentially ineffective interventions.
To combat these diagnostic challenges, healthcare professionals are urged to adopt comprehensive testing strategies, especially during peak flu and COVID-19 seasons. Empowering clinicians with the latest diagnostic tools and guidelines can enhance accuracy, facilitate earlier interventions, and ultimately improve patient outcomes in cases of co-infection.
Meta-Analysis Findings on COVID-Flu Coinfection
A comprehensive meta-analysis has revealed staggering findings concerning the rates of COVID-flu coinfection. With an overall estimated prevalence of 14%, the research illustrates significant variations among studies, indicating a high level of heterogeneity in reporting. Such discrepancies could be attributed to differing geographies, methodologies, and time frames studied, highlighting the complexity of understanding viral interactions in real-world settings.
Furthermore, the study’s conclusions emphasize the necessity for refined meta-regression models to explore how these factors may contribute to the observed heterogeneity. Identifying clear patterns will be imperative for future research and public health recommendations to address the dual threat posed by these respiratory pathogens.
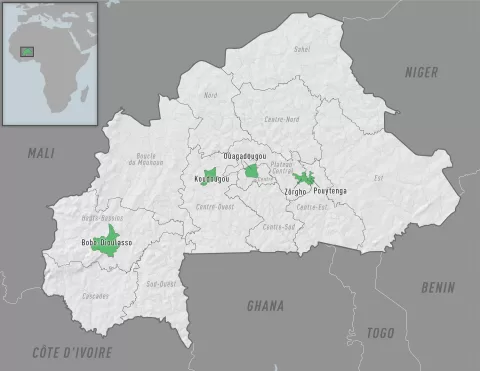
Geographical Variations in Virus Coinfection Rates
The geographical distribution of COVID-19 flu prevalence has shown notable regional variations, especially between Asia and Europe. In the meta-analysis, Europe exhibited some of the highest recorded rates of coinfection at 21%, indicating a pressing need for targeted public health strategies in these areas. Understanding these regional nuances can foster tailored health responses to contain the spread of these infections and better allocate resources where they are most needed.
Such geographical disparities in virus prevalence further necessitate international collaborations and data-sharing initiatives among researchers. Sharing insights and findings on COVID-19 and influenza A/B coinfections can illuminate trends and aid in developing global health strategies, ultimately reducing infections and improving healthcare outcomes worldwide.
Viral Co-Infection Treatment Options
Effective treatment for COVID-flu coinfection remains a challenge due to the complexities involved in managing two viral infections simultaneously. Current therapeutic guidelines need to accommodate the duality of symptoms and treatment repercussions. Research continues to explore viable treatment options that address both viruses, contributing to the knowledge base on optimal management strategies for co-infected patients.
Existing antiviral medications have shown promise, yet more studies are vital to determine the most effective protocols for patients facing COVID-19 alongside influenza. Continued investigation into treatment efficacy, along with a deeper understanding of viral interactions, will be critical for improving clinical outcomes and managing the public health ramifications of viral co-infections.
The Role of Data in Understanding COVID-19 and Flu Dynamics
The integration of comprehensive data analysis plays a pivotal role in elucidating the dynamics surrounding COVID-19 flu prevalence and coinfection rates. By employing different statistical models and data collations from various studies, health researchers can gain insights into the patterns of infection and co-infection, enhancing their understanding of the diseases’ interactions.
Furthermore, tracking data trends helps public health officials make informed decisions regarding vaccination strategies and resource allocation. By leveraging data analytics, we can forecast potential spikes in cases, facilitate timely public health responses, and refine strategies aimed at minimizing the impacts of such viral infections on communities.
Future Research Directions on COVID-19 and Influenza
Given the rising concern regarding COVID-flu coinfections, future research must focus on several key areas to enhance our understanding and management strategies. Investigating the long-term effects of coinfections on health outcomes will prove invaluable, especially as survivors of COVID-19 continue to grapple with post-viral complications. Continued exploration into how such infections interact at the cellular and systemic levels is also essential.
Moreover, research must be directed towards the development of combination vaccines and therapies that could prevent both COVID-19 and influenza A/B. Innovative approaches, such as genetic and recombinant technologies, could lead to breakthroughs that significantly reduce the burden of these diseases and protect at-risk populations from simultaneous infections.
Frequently Asked Questions
What is the prevalence of COVID-flu coinfection globally?
According to a recent meta-analysis of 38 studies, the global prevalence of COVID-flu coinfection is estimated at 14%. This rate reflects the prevalence of influenza A/B coinfections among COVID-19 patients, with variations noted particularly in Asia and Europe.
How do COVID-19 and influenza A/B co-infections affect hospitalization risks?
Co-infections of COVID-19 and influenza A/B can significantly increase hospitalization risks. Patients coinfected with these viruses face exacerbated respiratory symptoms and complications, including pneumonia and respiratory failure, which can lead to higher rates of severe cases and hospital admissions.
What challenges do healthcare providers face in diagnosing COVID-flu coinfection?
One of the main challenges in diagnosing COVID-flu coinfection is that both viruses share similar symptoms. Diagnostic tests may fail to differentiate between COVID-19 and influenza, complicating clinical assessments and appropriate treatment protocols for affected patients.
Are COVID-19 coinfections with influenza A/B more common in certain geographical areas?
Yes, the meta-analysis indicates that the prevalence of COVID-19 coinfections with influenza A/B is notably higher in regions like Asia and Europe, where the rates can reach up to 21%. This geographic variation may stem from differing public health policies and vaccination coverage.
What treatment strategies are recommended for managing COVID-flu coinfections?
Optimal treatment for COVID-flu coinfections is crucial for mitigating disease severity. High vaccination rates against both COVID-19 and seasonal influenza are recommended to reduce the incidence of these co-infections and their associated complications.
How does the co-existence of COVID-19 and influenza A/B affect immune responses?
The co-existence of COVID-19 and influenza A/B can lead to immune overload, making the body’s immune response less effective against either virus. This interaction can worsen respiratory symptoms and lead to more severe health outcomes for individuals with co-infections.
What implications do COVID-flu coinfection statistics have for public health measures?
The observed 14% prevalence of COVID-flu coinfection underscores the need for robust public health measures, including vaccination campaigns, to prevent co-infection and reduce burden on healthcare systems, especially during periods of high respiratory virus activity.
Is there a relationship between vaccination coverage and the rates of COVID-flu coinfection?
Yes, high vaccination coverage against both SARS-CoV-2 and seasonal influenza may lower the rates of COVID-flu coinfection, as seen in declines in hospitalizations related to severe cases during the pandemic.
| Key Point | Details |
|---|---|
| Global COVID-flu Coinfection Rate | 14% prevalence based on a meta-analysis of 38 studies. |
| Regions with Highest Rates | Asia and Europe have the highest rates of influenza A/B co-infection, with significant variation across studies. |
| Impact of Coinfection | Coinfection can lead to severe respiratory symptoms and increased risks of hospitalizations and mortality. |
| Heterogeneity in Studies | Substantial variability in studies due to geographic, methodological, and diagnostic criteria differences. |
| Vaccination Effects | Higher vaccination rates against both viruses may reduce the risk of co-infection. |
| Consistency Over Time | Coinfection rates remained similar before and after 2021 (14%). |
Summary
COVID-flu coinfection presents a significant global health challenge, with a reported prevalence of 14%. This meta-analysis highlights the complexities arising from co-infections, particularly in regions like Asia and Europe where rates are highest. The intertwining of COVID-19 and influenza can exacerbate respiratory issues and complicate clinical treatment due to overlapping symptoms. With notable heterogeneity among studies, continuous monitoring and vaccination efforts are critical to mitigate the impact of such co-infections.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.