COVID-19 cardiovascular risk has emerged as an alarming concern, significantly increasing the likelihood of serious heart conditions such as heart attack and stroke, as revealed by recent studies. Research indicates that the effects of COVID-19 can persist for up to three years post-infection, suggesting long-term health implications for those infected. Specifically, adults with non-O blood types—A, B, and AB—display an even greater susceptibility to these risks compared to those with type O blood. The urgency of addressing this elevated heart attack risk is intertwined with broader cardiovascular disease prevention efforts, especially for those who experienced severe cases. Understanding these long-term effects is crucial for public health strategies aimed at mitigating stroke risk COVID-19 survivors might face.
The association between COVID-19 and cardiovascular complications underscores the pressing need to explore its implications on heart health. As the pandemic recedes, the long-lasting effects of the virus are becoming clearer, particularly regarding the increased likelihood of heart-related ailments. Individuals who were hospitalized due to COVID-19 are experiencing elevated rates of cardiovascular problems, comparable to those with established risk factors like type 2 diabetes. The interplay of various blood types and their relationship to COVID-19 outcomes also adds another layer of complexity to this issue. Moving forward, proactive measures in cardiovascular disease prevention will be essential for enhancing patient care and improving health outcomes for COVID-19 survivors.
Understanding COVID-19 and Cardiovascular Risks
The emergence of COVID-19 has not only highlighted the immediate health threats associated with the virus but also its long-term implications, particularly concerning cardiovascular health. Recent research demonstrates that COVID-19 infection significantly increases the risk of serious cardiovascular events, such as heart attacks and strokes, which can persist for up to three years following the initial infection. This prolonged risk underscores the importance of ongoing monitoring and preventive care for individuals who have experienced COVID-19.
Moreover, the study published in the journal Arteriosclerosis reveals that individuals from specific blood types, notably A, B, and AB, are at an even greater risk of heart attack and stroke after contracting COVID-19. This association suggests that genetic factors play a crucial role in determining the extent of cardiovascular risk linked to the virus, indicating a need for tailored health interventions based on individual risk factors.
The Link Between Blood Type and COVID-19 Outcomes
An intriguing aspect of the COVID-19 research is the correlation found between blood type and the severity of cardiovascular outcomes. Individuals with non-O blood types—A, B, and AB—exhibited a significantly higher risk profile for experiencing severe cardiovascular events post-COVID-19. This finding prompts further exploration into the genetic and biochemical mechanisms that may predispose certain blood types to more severe complications following COVID-19 infection.
Understanding the relationship between blood type and health outcomes allows for improved risk stratification in clinical settings. It raises important questions about how blood characteristics might interact with infectious diseases like COVID-19, and whether customized prevention strategies could mitigate the heightened heart attack and stroke risks among those with non-O blood types.
Long-Term Cardiovascular Effects Post-COVID-19 Infection
COVID-19’s impact extends beyond immediate symptoms, with emerging evidence revealing significant long-term cardiovascular risks for those affected. Research indicates that individuals who were hospitalized due to COVID-19 demonstrate a heart attack and stroke risk that rivals those with established cardiovascular concerns like type 2 diabetes. This parallels other studies showing that COVID-19 inflicts lasting damage on the cardiovascular system, necessitating vigilant long-term follow-up and intervention strategies.
These findings highlight the importance of integrating COVID-19 history into cardiovascular risk assessments. Medical practitioners should consider a patient’s COVID-19 infection history as a vital component of their overall health profile, potentially categorizing severe COVID-19 as a significant risk factor for developing cardiovascular diseases.
Preventive Strategies for Cardiovascular Health After COVID-19
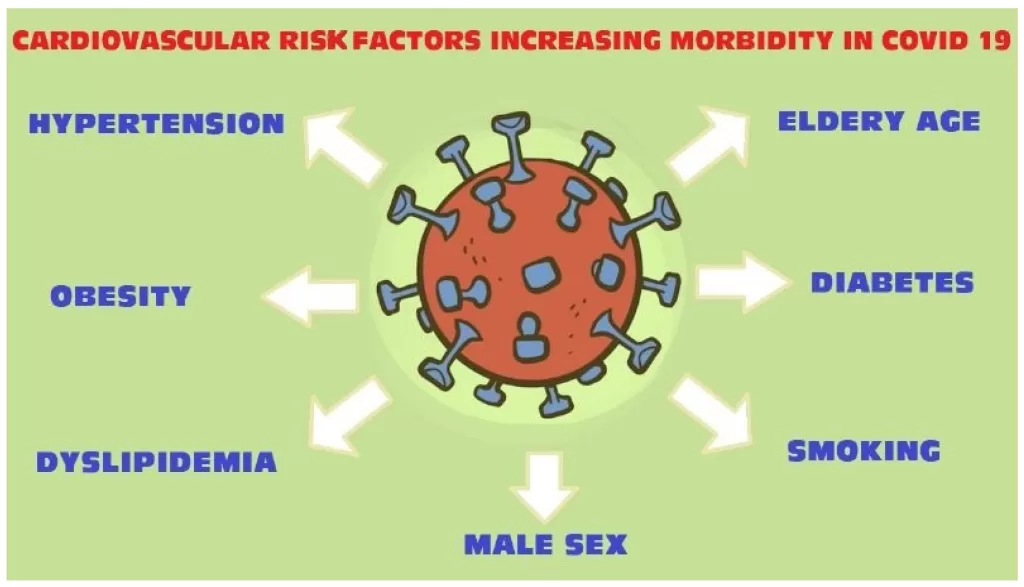
Given the alarming increase in heart attack and stroke risks associated with COVID-19, there is an urgent need for effective cardiovascular disease prevention strategies targeted at COVID-19 survivors. Research suggests that those with a history of COVID-19 might benefit from proactive management of cardiovascular health, similar to individuals with recognized risk factors such as diabetes or hypertension. This can include lifestyle modifications, regular health screenings, and possibly early interventions with medications to mitigate cardiovascular risks.
Healthcare providers are now called to prioritize preventive care in patients who have previously contracted COVID-19, emphasizing the necessity of comprehensive cardiovascular assessments. This might include lifestyle counseling, dietary recommendations, and tailored exercise programs aimed at improving heart health and minimizing the potential long-term impacts of COVID-19 on the cardiovascular system.
COVID-19 Hospitalization: A Marker for Increased Cardiovascular Risk
Research from the UK Biobank underscores that hospitalization due to COVID-19 serves as a potent indicator of long-term cardiovascular health risks. This association is comparable to traditional risk factors such as pre-existing cardiovascular disease. For those hospitalized with severe COVID-19, the likelihood of facing heart attacks or strokes is significantly heightened, necessitating a paradigm shift in managing post-COVID care.
This evidence suggests that medical professionals should view severe COVID-19-related hospitalization as a flag for intensifying cardiovascular risk evaluations. Implementing tailored CVD prevention strategies for these individuals could prove critical in mitigating future cardiovascular events and improving long-term health outcomes.
The Role of Care Providers in Managing COVID-19 Cardiovascular Risks
As healthcare providers navigate the implications of COVID-19 on long-term health, their role in managing cardiovascular risks becomes increasingly vital. With compelling evidence linking COVID-19 to heightened heart attack and stroke risks, medical professionals are encouraged to implement follow-up protocols specifically designed for recovered COVID-19 patients. This might include routine cardiovascular assessments and patient education on recognizing symptoms of potential heart complications.
Moreover, healthcare practitioners should foster a dialogue with patients recovering from COVID-19 regarding the importance of cardiovascular health, encouraging them to adopt healthier lifestyles and report any concerning symptoms early. Such proactive engagement can facilitate timely intervention and ultimately reduce the risk of severe cardiovascular outcomes.
Implications of COVID-19 Research for Global Health
The findings from recent studies on COVID-19 and cardiovascular risks highlight critical implications for global health, especially as many individuals worldwide have contracted the virus. With an increased awareness of COVID-19’s potential to exacerbate heart attack and stroke risks, health systems must be prepared to address these rising issues as a public health priority. This includes integrating cardiovascular health evaluations into post-COVID recovery protocols across the healthcare spectrum.
Additionally, these insights could influence public health policies and health education campaigns, emphasizing the connections between infectious diseases and cardiovascular health. By raising awareness and focusing resources on these findings, health authorities can better prepare for the long-term consequences of the pandemic on cardiovascular disease incidence globally.
The Significance of Ongoing Research in COVID-19 and Cardiovascular Health
Continuous research into the long-term effects of COVID-19 on cardiovascular health is essential to understand and address the heightened risks associated with the virus. Insights from ongoing studies can enhance our knowledge regarding not only the cardiovascular impacts of COVID-19 but also the underlying mechanisms that may predispose individuals to these risks. As the research evolves, it can guide clinical practices and inform public health strategies aimed at mitigating adverse health outcomes.
Furthermore, ongoing research can aid in developing targeted interventions, precision medicine approaches, and innovative treatments to protect vulnerable populations, particularly those with specific blood types or underlying health conditions. The longevity of cardiovascular risks following COVID-19 reinforces the need for sustained investigation and adaptation of healthcare services to address this emerging public health landscape.
Understanding the Connection Between COVID-19 Severity and Cardiovascular Outcomes
The severity of COVID-19 symptoms has been directly linked to increased cardiovascular outcomes, with studies confirming that individuals who experience severe illness are at a greater risk for heart attacks and strokes post-recovery. This connection highlights the need for detailed assessments of patients’ cardiovascular health during and after severe bouts of COVID-19, especially for individuals with co-existing health conditions.
Hence, healthcare providers should prioritize monitoring cardiovascular health in individuals who had severe COVID-19, ensuring that preventative care strategies are promptly initiated. Recognizing the link between COVID-19 severity and cardiovascular risk can lead to dedicated healthcare plans that effectively minimize long-term consequences for these patients.
Frequently Asked Questions
How does COVID-19 increase cardiovascular risk like heart attack and stroke?
COVID-19 infection has been shown to elevate the risk of cardiovascular events such as heart attacks and strokes for up to three years after the initial infection. Research indicates that this increased risk can be comparable to traditional cardiovascular risk factors, including type 2 diabetes and peripheral artery disease.
Are individuals with non-O blood types at higher risk for heart attacks after COVID-19?
Yes, studies have found that individuals with non-O blood types (A, B, or AB) have a significantly higher risk of heart attack and stroke following a COVID-19 infection. This risk is approximately 65% higher compared to those with type O blood.
What are the long-term effects of COVID-19 on cardiovascular health?
COVID-19 can lead to long-term cardiovascular complications, with increased risks of heart attack, stroke, and death lasting for up to three years post-infection. This underscores the importance of cardiovascular disease prevention strategies for those who have recovered from COVID-19.
Should COVID-19 be considered a cardiovascular risk factor?
Absolutely. Given the substantial increase in heart attack and stroke risks associated with severe COVID-19 infections, it may be appropriate to classify COVID-19 as an additional risk factor for cardiovascular disease, similar to established factors like type 2 diabetes.
What preventive measures can help mitigate the cardiovascular risks associated with COVID-19?
Individuals who have suffered from COVID-19 should consider cardiovascular disease prevention treatments such as lifestyle modifications, regular health screenings, and possibly medication, especially if they have other risk factors. Consulting with healthcare providers is crucial.
Can people with a history of COVID-19 still enhance their cardiovascular health?
Yes, individuals with a history of COVID-19 can still improve their cardiovascular health. Engaging in regular physical activity, maintaining a heart-healthy diet, managing stress, and avoiding smoking are effective strategies to enhance cardiovascular well-being.
Is there a relation between COVID-19 severity and long-term heart risks?
Yes, the severity of COVID-19—especially in cases that required hospitalization—is directly related to higher long-term risks of cardiovascular events. The more severe the infection, the greater the risk of heart complications thereafter.
What population is most at risk for increased cardiovascular complications from COVID-19?
According to recent studies, older adults, individuals with pre-existing conditions, and those with non-O blood types are at an elevated risk for cardiovascular complications after a COVID-19 infection.
How should healthcare systems adapt to the findings on COVID-19 and cardiovascular risks?
Healthcare systems should prioritize cardiovascular assessments for individuals with a history of COVID-19 infections, implement preventive care strategies, and educate patients about the long-term cardiovascular risks post-infection.
What is the significance of this research on COVID-19’s impact on cardiovascular health?
The findings highlight the global importance of understanding COVID-19’s long-term cardiovascular risks. With millions affected, it emphasizes the need for ongoing monitoring and preventive measures to reduce the burden of cardiovascular disease stemming from COVID-19.
| Key Findings | Details |
|---|---|
| COVID-19 Increases Cardiovascular Risk | COVID-19 infection increases the risk of heart attack and stroke for up to three years post-infection. |
| Blood Type Impact | Individuals with blood types A, B, or AB are at a higher risk of heart attack and stroke compared to type O. |
| Study Background | The study analyzed over 10,000 adults, focusing on the long-term risks of cardiovascular events after COVID infection. |
| Significant Statistics | The risk of heart attack and stroke was more than twice as high in COVID-positive individuals, and nearly four times higher for hospitalized patients. |
| Call for Preventive Measures | Recommendations for cardiovascular disease prevention for individuals with a history of COVID-19 infection. |
Summary
COVID-19 cardiovascular risk has become a critical area of concern as recent studies show that individuals infected with COVID-19 face elevated chances of heart attack and stroke well after recovery. The implications of this increased risk highlight the importance of preventive care for those who have suffered from COVID-19, particularly among those with non-O blood types who are more susceptible. As researchers continue to explore these findings, it becomes evident that managing cardiovascular health post-COVID is essential for improving long-term outcomes.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.