Colorectal cancer microbiota plays a crucial role in the complex landscape of colorectal cancer (CRC), a disease that continues to rise globally. Recent research has illuminated how gut microbiota, specifically certain biofilm-producing bacteria like Fusobacterium nucleatum and Bacteroides fragilis, influence CRC pathogenesis. These pathogenic microbes not only interrupt normal gut flora but also contribute to an inflammatory environment that fosters tumor growth. The intricate relationship between these bacteria and the development of colorectal tumors highlights their potential as biomarkers for cancer progression and as targets for innovative therapies. Understanding these microbial dynamics is vital for enhancing CRC management and prevention strategies.
The microbiome associated with colorectal cancer involves a nuanced interaction of gut microbiota that may contribute to cancer development and progression. As studies delve into the roles of various microbial communities, particular attention is directed toward biofilm-producing organisms such as Bacteroides fragilis and Fusobacterium nucleatum, which have been linked to colorectal cancer. Alterations in these microbial populations can create an environment favorable for cancer initiation, reflecting broader implications for understanding cancer biology. This exploration into the relationships between bacteria, inflammation, and tumor formation deepens our grasp of CRC etiology and may guide future therapeutic interventions.
Understanding the Role of Gut Microbiota in Colorectal Cancer
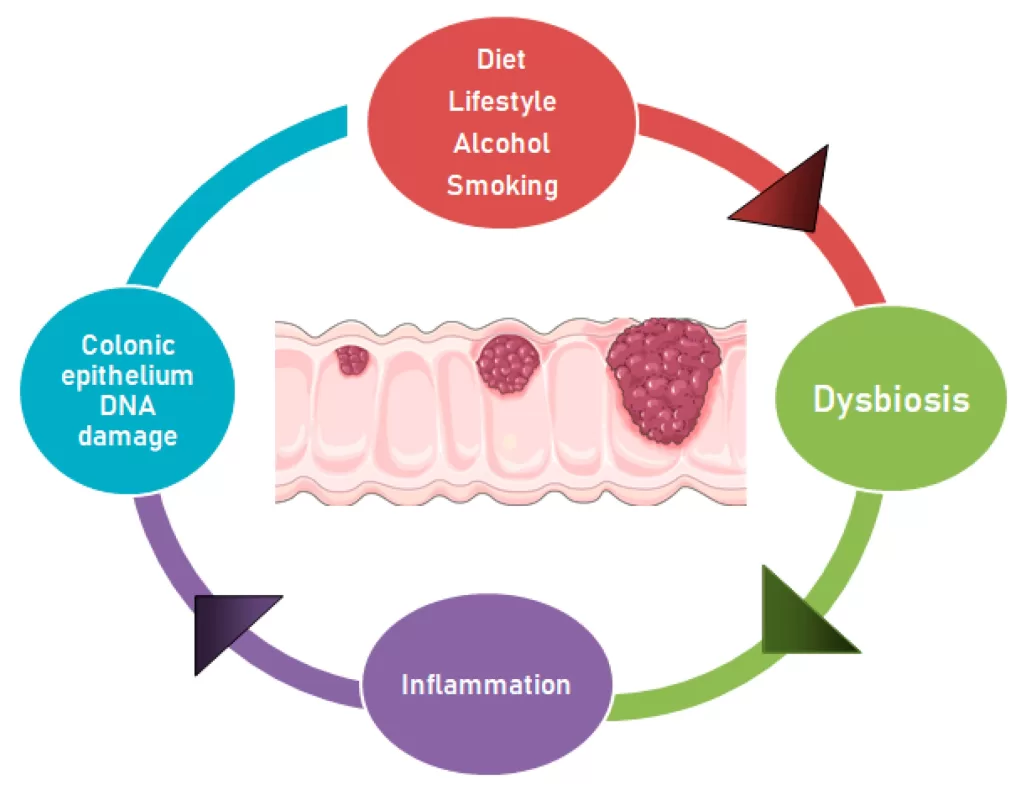
Gut microbiota plays a pivotal role in various aspects of human health, influencing not only metabolic functions but also the immune system. In the context of colorectal cancer (CRC), abnormalities in the gut microbiota composition have been linked to tumorigenesis. Numerous studies have shown that a disruption in the balance of beneficial and pathogenic bacteria can create an inflammatory environment within the colon, which may facilitate cancer development. Specific bacterial taxa, like Fusobacterium nucleatum, have gained attention for their ability to contribute to CRC pathogenesis by promoting cellular processes that lead to tumor growth.
Moreover, biofilm-forming bacteria are increasingly recognized for their contributions to CRC. These bacteria can form dense microbial communities that protect pathogenic strains from host immune responses and antibiotic treatments. By adhering to the colonic mucosa, these biofilms not only enhance bacterial survival but also create localized environments conducive to inflammation, further driving cancer progression. Understanding these interactions between gut microbiota and CRC is crucial for developing targeted therapies and preventive strategies.
Biofilm-Producing Bacteria: Key Players in CRC Pathogenesis
The presence of biofilm-producing bacteria in colorectal cancer tissues has been identified as a significant factor influencing disease progression. In particular, Bacteroides fragilis and Fusobacterium nucleatum have emerged as critical players in CRC pathogenesis. These bacteria not only exhibit enhanced gene expression in tumor environments but also establish dense biofilms that may alter local microbial ecosystems. Such biofilms can disrupt normal gut homeostasis and promote an inflammatory state, essential for tumor initiation and progression.
Recent research highlights that the spatial distribution of these biofilm-forming bacteria within tumor tissues correlates with the microenvironment’s characteristics. For example, within the crypts of Lieberkuhn, the concentration of Fusobacterium nucleatum is particularly pronounced, suggesting a direct association with tumor development. The intricate relationship between biofilm-producing bacteria and tumor biology points to the necessity of exploring these organisms not merely as bystanders but as active contributors to CRC pathogenesis. This understanding could pave the way for innovative therapeutic approaches targeting biofilms in CRC.
The Impact of Microbial Sidedness on CRC Development
Recent findings have indicated that the sidedness of colorectal cancer—whether left-sided or right-sided—can significantly impact the gut microbiota composition. Studies have shown distinct microbial profiles associated with different tumor locations, impacting disease prognosis and treatment responses. For instance, left-sided CRC is often enriched with specific pathogenic bacteria such as Bacteroides fragilis, which may worsen inflammation and promote tumor progression in that region.
This variation in microbial diversity and composition underscores the importance of personalized treatment strategies in CRC management. Targeting specific bacterial populations linked to tumor sidedness could lead to more effective interventions. Furthermore, comprehending how these microbial differences relate to gut microbiota’s overall health can help clinicians devise holistic approaches for CRC patient care, integrating lifestyle and dietary recommendations alongside tailored treatments.
Exploring Fusobacterium Nucleatum: The Oncogenic Microbe
Fusobacterium nucleatum has been identified as a key microbial player in colorectal cancer, linking its presence to tumor development. This bacterium has shown to promote inflammation and enhance cancer cell proliferation through various mechanisms, including immune evasion and the induction of oncogenic pathways. Its ability to thrive in biofilm forms further complicates the inflammatory states within the gut, suggesting that Fusobacterium could serve as both a marker and a mediator of CRC progression.
Understanding the functional roles of Fusobacterium nucleatum in CRC highlights the urgent need for targeted therapies that address the microbial contributions to cancer. Research is ongoing to explore potential interventions that could disrupt the biofilm structures or inhibit the pathogenic actions of F. nucleatum, paving the way for innovative strategies in CRC prevention and treatment.
The Role of Bacteroides Fragilis in Gut Microbiota and CRC
Bacteroides fragilis is another significant bacterium associated with colorectal cancer. Studies indicate that while it is a normal component of the gut microbiota, certain strains can become pathogenic under specific conditions, particularly when accompanied by dysbiosis. This bacterium is known for its ability to form biofilms, which can protect harmful bacteria and promote an environment conducive to cancer development. The balance between different strains of Bacteroides can heavily influence gut health and disease state.
The investigation into Bacteroides fragilis not only sheds light on its role in CRC but also opens up avenues for microbiome-based therapies. Targeting pathogenic strains could provide a means of modulating the gut environment to restore balance and potentially reduce CRC risk. Ongoing research is focusing on identifying microbial signatures that could predict CRC risk, emphasizing the importance of B. fragilis in future therapeutic strategies.
Therapeutic Implications of Targeting Gut Microbiota in CRC
The emerging evidence connecting gut microbiota and colorectal cancer underscores the potential for novel therapeutic approaches. By understanding how specific bacteria, such as Fusobacterium nucleatum and Bacteroides fragilis, contribute to CRC pathogenesis through biofilm formation and inflammatory responses, new interventions can be developed. One such approach may involve the use of probiotics or prebiotics to restore a healthy gut microbiota balance, potentially reducing the risk of tumor development.
Moreover, microbiota-focused therapies, including targeted antibiotics, could offer a strategy to selectively deplete pathogenic bacteria responsible for tumor promotion. Clinical trials are needed to assess the effectiveness of these interventions and their impacts on CRC outcomes. As research continues to uncover the intricate relationships between microbiota, biofilms, and cancer, refining therapeutic strategies based on gut microbiota modulation may significantly benefit CRC prevention and management.
Examining Biofilms and Their Influence on Therapeutic Targets in CRC
Biofilms present a unique challenge in the treatment of colorectal cancer due to their protective properties, which shield pathogenic bacteria from host immune responses and conventional therapies. The dense structures formed by bacteria like Bacteroides fragilis and Fusobacterium nucleatum not only harbor these pathogens but create an environment that promotes chronic inflammation and disease progression. Understanding the mechanisms of biofilm development is essential for identifying new therapeutic targets that could render these bacteria more susceptible to treatment.
Emerging research suggests that disrupting biofilm formation may enhance the efficacy of existing treatments and reduce tumor burden. Investigations into compounds that can inhibit biofilm development or destabilize existing biofilms could lead to significant advancements in the management of CRC. As the field continues to evaluate the complex interactions between biofilms, gut microbiota, and cancer progression, innovative therapeutic strategies may emerge, improving outcomes for CRC patients.
The Importance of Microbiota Diversity in CRC Prevention
Microbiota diversity plays a crucial role in maintaining gut health and preventing colorectal cancer. A diverse gut microbiome can enhance immune responses, promote gut barrier integrity, and inhibit the growth of pathogenic organisms. Research indicates that a reduction in microbiota diversity is often associated with an increased risk of CRC, highlighting the importance of diet and lifestyle factors that can support a healthy microbial ecosystem.
Encouraging dietary practices that promote gut diversity, such as consuming prebiotic and probiotic-rich foods, can be an effective preventive strategy against CRC. Furthermore, educating patients on the impact of lifestyle choices—such as diet, physical activity, and antibiotic use—on gut microbiota can empower them in their cancer prevention efforts. Continued studies are necessary to explore the precise connections between microbiota diversity and CRC risk, paving the way for public health initiatives focused on promoting gut health.
Future Directions in CRC Microbiota Research
As research continues to unravel the complex relationships between gut microbiota and colorectal cancer, future studies are poised to explore several pivotal areas. One key direction is the identification of microbial biomarkers that could predict an individual’s risk of CRC, potentially allowing for earlier interventions or screening strategies. Investigating how lifestyle factors and dietary habits influence microbial communities could yield insights into preventive measures for at-risk populations.
Furthermore, the development of microbiome-targeted therapies holds promise for transforming CRC treatment paradigms. As understanding deepens regarding how specific bacteria contribute to tumorigenesis, the potential to create tailored therapeutic approaches becomes increasingly feasible. These advancements may not only benefit those with existing CRC but could also play a significant role in preventative strategies, enhancing the overall landscape of cancer care.
Frequently Asked Questions
What role does gut microbiota play in colorectal cancer (CRC) development?
Gut microbiota significantly influences colorectal cancer (CRC) development, as alterations in microbial composition can promote inflammation and tumor progression. Studies show that increases in specific pathogenic bacteria, including Fusobacterium nucleatum and Bacteroides fragilis, contribute to CRC pathogenesis by forming biofilms that enhance tumor initiation.
How are biofilm-producing bacteria related to colorectal cancer pathogenesis?
Biofilm-producing bacteria play a crucial role in colorectal cancer pathogenesis by establishing a pathogenic environment within the gut. These bacteria, like Bacteroides fragilis and Fusobacterium nucleatum, are found in higher abundance in CRC tissues, suggesting they contribute to tumorigenesis through inflammatory processes and interactions with host cells.
What distinguishes the gut microbiota in left-sided versus right-sided colorectal cancer?
The gut microbiota composition varies significantly between left-sided and right-sided colorectal cancer. Studies indicate that Fusobacteriota and Bacteroidota are notably enriched in left-sided CRC, whereas a different microbial profile may be associated with right-sided lesions, highlighting the tumor’s location’s influence on microbial diversity and potential disease mechanisms.
Can the presence of Fusobacterium nucleatum indicate the severity of colorectal cancer?
Yes, the presence of Fusobacterium nucleatum in colorectal cancer tissues is often correlated with more advanced disease stages. Higher abundance of this biofilm-producing bacterium has been linked to worse prognosis and tumor aggression, indicating its potential role as a biomarker for CRC severity.
What methods were used to analyze gut microbiota in colorectal cancer studies?
In colorectal cancer studies, gut microbiota analysis typically involves sequencing the 16S rRNA gene to identify bacterial DNA from biopsy samples. Techniques like scanning electron microscopy (SEM) and fluorescence in situ hybridization (FISH) are also employed to visualize biofilm structures and assess bacterial localization within tissues, providing insight into microbial interactions in CRC.
Why are Bacteroides fragilis and Fusobacterium nucleatum considered critical in CRC research?
Bacteroides fragilis and Fusobacterium nucleatum are critical in colorectal cancer research due to their prominent role in enhancing tumorigenesis through inflammatory pathways and biofilm formation. Their elevated presence in CRC tissues underscores their potential as therapeutic targets or biomarkers for early detection and prognosis of colorectal cancer.
| Aspect | Key Points |
|---|---|
| Colorectal Cancer (CRC) | Prevalent global malignancy with complex causes and significant mortality rates. |
| Microbiota’s Role | Gut microbiota and biofilm-producing bacteria may influence CRC progression. |
| Study Methodology | Analysis of paired biopsies from 35 CRC patients using 16S rRNA sequencing and biofilm visualization techniques. |
| Microbiota Findings | Firmicutes were dominant, with significant presence of Bacteroides and Fusobacterium, especially in left-sided CRC. |
| Biofilm Production | Higher gene expression of biofilm producers like B. fragilis and F. nucleatum found in tumor tissues. |
| Tumor Sidedness Impact | Differences in microbial profiles between left and right-sided CRC; increased pathological bacteria in CRC tissues. |
| Study Limitations | Small sample size and focus limited to stage III CRC; calls for further research across stages and populations. |
Summary
Colorectal cancer microbiota play a crucial role in the pathogenesis of CRC, as highlighted by significant alterations in gut microbial communities and increased biofilm formation. These findings suggest that understanding the relationship between microbiota and CRC can provide insights into disease mechanisms and potential therapeutic strategies.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.