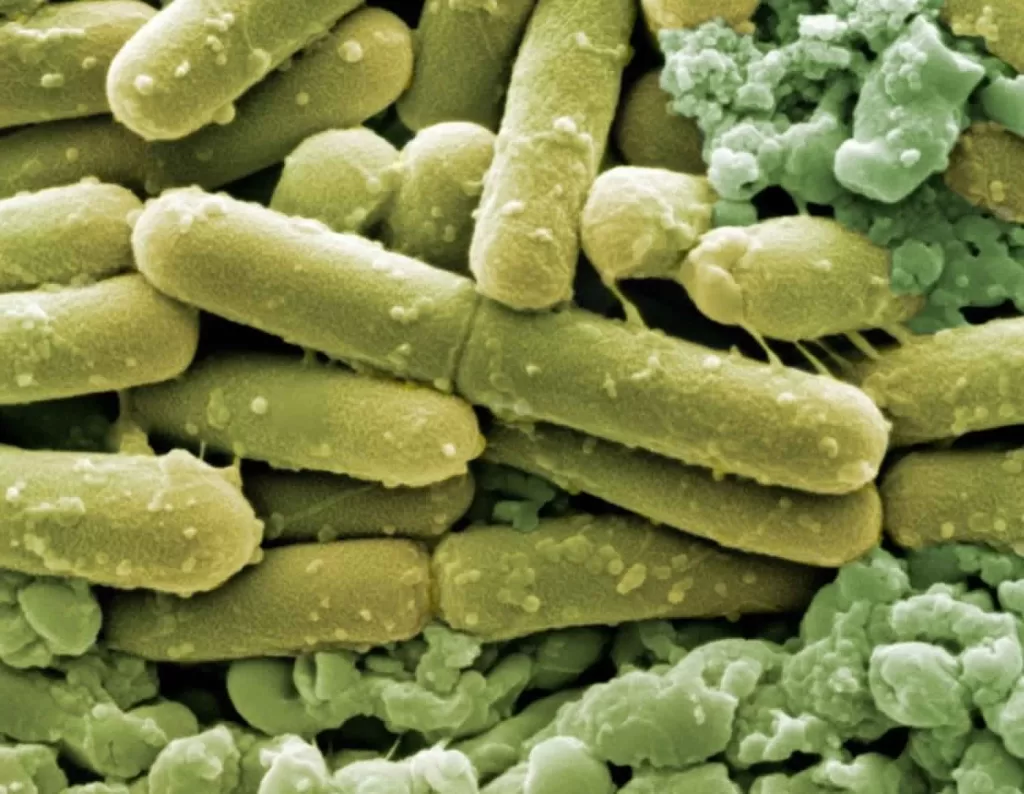
Clostridioides difficile infection (CDI) remains a significant public health concern, particularly within the context of healthcare-associated infections (HAIs). In Canada, an alarming trend has been observed where the rates of adult CDI have fluctuated, with a notable decrease in healthcare-associated cases by 19.9% from 2015 to 2022. Meanwhile, community-associated infections (CAI) have held steady, highlighting the varied epidemiology of this pathogen. The prevalence of CDI among pediatric patients also warrants attention, as severe outcomes have been documented in cases of pediatric CDI (pediatric CDI). Understanding these trends is crucial, not just for adult populations, but importantly for children, given that the characteristics and outcomes differ considerably. Continued surveillance and research are necessary for effectively combating CDI and improving patient outcomes.
The infection caused by Clostridioides difficile, often referred to as C. difficile or simply CDI, is a growing issue that poses risks across various healthcare settings. This bacterium, responsible for a range of gastrointestinal diseases, often emerges in the wake of antibiotic use, leading to both healthcare-associated and community-associated cases. Trends in adult CDI cases compared to pediatric CDI highlight the dynamic nature of this infection, with varying patterns of incidence, severity, and treatment resistance noted in different age groups. Enhanced understanding of C. difficile epidemiology is essential for healthcare providers and policymakers alike, as these insights can guide better prevention and intervention strategies. As we navigate the complexities of CDI, prioritizing surveillance efforts can promote more effective infection control measures.
Overview of Clostridioides difficile Infections
Clostridioides difficile infection (CDI) continues to pose a significant threat to public health across various demographics. This bacterium is particularly notorious for causing severe diarrhea and gastrointestinal complications, often after the use of antibiotics that disrupt the normal gut flora. CDI can manifest in two forms: healthcare-associated infections (HA-CDI), which typically arise in hospitals and long-term care facilities, and community-associated infections (CA-CDI), which can occur in otherwise healthy individuals outside of healthcare settings. Understanding the distinct epidemiology of these infections is crucial for implementing effective preventative strategies.
In Canada, a comprehensive study conducted from 2015 to 2022 revealed that a staggering 94.9% of CDI cases were found in adults, with a notable prevalence of healthcare-associated cases. Not only did this research highlight the epidemiological trends within adult populations, but it also emphasized the growing concerns related to pediatric CDI. By recognizing the differences in CDI onset and outcomes among various age groups, public health initiatives can be more effectively tailored to address these disparities and enhance the overall patient care approach.
Epidemiology of CDI in Adult and Pediatric Populations
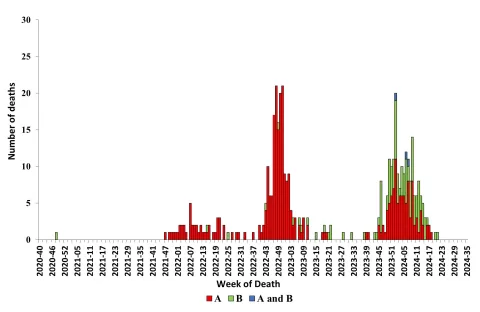
Analyzing the epidemiology of CDI in adults versus pediatric populations reveals distinct patterns in acquisition and outcomes. The recent study showed a marked decrease in adult healthcare-associated CDI rates by 19.9%, suggesting that improved infection control practices are yielding positive results. However, pediatric healthcare-associated infections also decreased significantly, by 29.6%, underscoring the importance of vigilance in younger patients who may present with different risk factors and disease progression. Understanding these demographic-specific trends allows healthcare professionals to tailor preventative measures and treatment protocols to effectively address the varied presentations of CDI.
Furthermore, the data revealed that community-associated CDI in both adults and children remained stable, indicating the need for ongoing monitoring and research. The identification of ribotype strain RT106 as the predominant type in both adult and pediatric cases marks a significant shift in CDI epidemiology, potentially influencing the management strategies employed by healthcare providers. This knowledge can advance our understanding of infection pathways and help develop targeted interventions that are crucial for controlling CDI spread in both community and healthcare settings.
Healthcare-Associated vs Community-Associated CDI Trends
The distinction between healthcare-associated (HA) and community-associated (CA) Clostridioides difficile infections plays a vital role in guiding treatment and prevention strategies. The observed decline in adult HA CDI rates coincides with enhanced infection control measures and antimicrobial stewardship practices in hospitals. This downward trend is encouraging; however, it raises questions about the sustainability of such improvements and whether similar reductions can be achieved in community settings where the dynamics of infection transmission differ.
On the other hand, pediatric cases have shown a remarkable decrease in CA CDI by 58.3%, indicating that awareness and educational efforts in both healthcare providers and the community are bearing fruit. This calls for continued emphasis on understanding and monitoring CA CDI, as these infections often present unique challenges in diagnosis and treatment. By addressing the factors leading to CA transmission, healthcare systems can better protect vulnerable populations and reduce the overall incidence of CDI.
Role of Antibiotic Use in CDI Incidence
Antibiotic use is a well-established risk factor for Clostridioides difficile infection, particularly because these medications can disrupt the gut microbiome and allow CDI to flourish. The Canadian study highlighted the importance of antibiotic stewardship in mitigating the incidence of both HA and CA CDI. With evidence linking antibiotic exposure to increased risk of CDI, healthcare facilities are increasingly focusing on developing protocols that minimize inappropriate antibiotic prescribing.
By implementing stringent antibiotic stewardship programs, hospitals can significantly reduce the rates of CDI while also addressing broader concerns related to antimicrobial resistance. Moreover, educating patients about the risks associated with antibiotic use is essential in community settings, where patients may not have the same level of oversight as in hospitals. Overall, a collaborative effort towards responsible antibiotic usage is crucial for improving patient outcomes and reducing the burden of CDI.
Impact of CDI on Patient Outcomes
The consequences of Clostridioides difficile infection can be severe, significantly impacting patient morbidity and mortality. An essential finding from the analysis of CDI in Canada was the stark contrast in clinical outcomes between adults and children. Adult patients exhibited a higher 30-day mortality rate of 10.6% compared to just 1.4% in pediatric patients. This discrepancy highlights the urgency needed in addressing CDI, especially in at-risk adult populations where severe outcomes are more prevalent.
Furthermore, the study underscored that severe outcomes, such as ICU admissions and colectomies, were substantially more common in adult cases. Such trends demand a multi-faceted approach that not only focuses on effective treatment but also emphasizes preventative care strategies tailored to the at-risk groups. Increasing clinician awareness of the potential severity of CDI in adults can lead to faster recognition and intervention, ultimately improving patient survival rates.
National Surveillance and CDI Monitoring
Continuous national surveillance is essential for tracking the epidemiology of Clostridioides difficile infection and its changing trends. The Canadian Nosocomial Infection Surveillance Program provides valuable insights into CDI cases across the country, enabling healthcare authorities to assess the effectiveness of infection control strategies and adjust as necessary. By compiling data from a vast network of hospitals, stakeholders can identify outbreaks more rapidly and allocate resources efficiently.
Moreover, this kind of ongoing monitoring facilitates the examination of emerging strains and antibiotic resistance patterns, which are critical for informing treatment guidelines. Surveillance results can guide public health initiatives aimed at education, early detection, and containment of CDI. As the landscape of CDI evolves, the importance of robust surveillance efforts cannot be overstated; these data play a pivotal role in preserving public health and optimizing clinical outcomes.
Future Directions for CDI Research
Research into Clostridioides difficile infection is continually evolving, driven by the need to better understand the factors influencing its incidence and management. Future studies should focus on examining the microbiome’s role in both adult and pediatric populations, particularly concerning susceptibility to CDI. Investigating potential protective factors that could be harnessed therapeutically might provide novel approaches for preventing CDI in at-risk patients.
Additionally, there is a pressing need for research into long-term outcomes for patients who have experienced CDI, including potential recurrence and the impact on their quality of life. This knowledge can help refine current treatment protocols and post-infection care strategies, ultimately leading to improved patient outcomes. A collaborative effort involving clinicians, epidemiologists, and researchers will be crucial in advancing CDI knowledge and enhancing public health responses.
Educational Interventions in CDI Prevention
Educational interventions are essential in combating the rise of Clostridioides difficile infections within both healthcare settings and the community. By providing training and resources to healthcare professionals, we can raise awareness of CDI risk factors, symptoms, and appropriate prescribing practices. This form of education serves as a crucial measure to reduce the incidence of healthcare-associated infections, facilitating quicker recognition and response to potential outbreaks.
Moreover, community-level education plays a critical role in addressing CA CDI, particularly among vulnerable populations. Programs designed to inform patients and their families about the importance of proper hygiene, recognizing symptoms, and when to seek medical care can empower individuals to take proactive steps in preventing CDI. Engaging community leaders and utilizing local platforms for awareness campaigns can significantly enhance the reach and efficacy of these educational efforts.
The Economic Burden of CDI
Clostridioides difficile infections represent a significant economic burden on healthcare systems globally. The costs associated with treating CDI go beyond medication expenses, encompassing extended hospital stays, potential surgical interventions, and long-term care for complications arising from severe cases. In Canada, the economic implications are multidimensional, necessitating a thorough analysis of CDI’s financial impact on both healthcare providers and patients.
By investing in prevention and control measures, healthcare systems can not only improve patient outcomes but also reduce the overall costs related to CDI treatment. Strategies such as enhanced infection control protocols, targeted surveillance, and antibiotic stewardship can ultimately lead to decreased hospitalization rates and associated costs. It’s imperative that policymakers and healthcare administrators prioritize CDI management within their budgeting frameworks to alleviate the financial strain on healthcare resources.
Frequently Asked Questions
What is Clostridioides difficile infection (CDI) and how does it affect patients?
Clostridioides difficile infection (CDI) is a bacterial infection that primarily affects the colon and leads to symptoms such as diarrhea, abdominal pain, and fever. It is particularly concerning in healthcare settings, where it can cause severe complications, including hospitalization and increased mortality rates, especially in adults compared to pediatric patients.
How prevalent are healthcare-associated and community-associated Clostridioides difficile infections (CDI) in adults?
In Canada from 2015 to 2022, healthcare-associated (HA) Clostridioides difficile infections (CDI) comprised 73.2% of adult cases, while community-associated (CA) CDI accounted for 26.8%. Although HA CDI rates in adults have decreased by 19.9%, community-associated cases have remained stable during this period.
What are the trends in pediatric Clostridioides difficile infection rates?
Pediatric Clostridioides difficile infection (CDI) reflects significant trends, with healthcare-associated infection rates dropping by 29.6% and community-associated rates declining drastically by 58.3% from 2015 to 2022. This highlights the importance of effective infection control measures in reducing CDI incidence among children.
What ribotypes are most commonly associated with Clostridioides difficile infection?
The study identified ribotype (RT) 106 as the most common ribotype associated with Clostridioides difficile infection (CDI) cases among both adults and pediatric patients during the period from 2015 to 2022, surpassing the previously dominant RT027. RT027 is particularly linked to severe outcomes in adult patients.
Why is surveillance important for understanding Clostridioides difficile infection epidemiology?
Ongoing surveillance for Clostridioides difficile infection (CDI) is crucial for understanding its evolving epidemiology and guiding public health interventions. By monitoring trends in both healthcare-associated and community-associated CDI, health authorities can identify outbreaks, assess the effectiveness of infection control strategies, and implement targeted prevention efforts.
What are the implications of Clostridioides difficile infection resistance patterns in treatment?
Research has shown that Clostridioides difficile infection (CDI) demonstrates differing resistance patterns, with adult cases exhibiting higher moxifloxacin resistance compared to pediatric cases. Understanding these resistance trends is vital for optimizing treatment strategies and managing CDI effectively across different age groups.
How do Clostridioides difficile infection outcomes differ between adults and children?
Clinical outcomes of Clostridioides difficile infection (CDI) vary significantly between adults and pediatric patients. Adult patients face a higher risk of severe outcomes, including ICU admission and death, with a 30-day mortality rate of 10.6%, whereas pediatric patients have a mortality rate of only 1.4%, indicating the need for tailored clinical approaches.
What preventive measures are effective against Clostridioides difficile infections?
Effective preventive measures against Clostridioides difficile infection (CDI) include enhanced infection control practices, judicious use of antibiotics to avoid disruption of gut flora, and proper hand hygiene in healthcare settings. Continued education and vigilance are essential to reduce both healthcare-associated and community-associated CDI cases.
| Key Point | Details |
|---|---|
| Study Overview | Investigation into HA and CA Clostridioides difficile infections (CDI) among adults and children in Canada from 2015-2022. |
| Total Cases | 30,824 reported CDI cases; 94.9% in adults and 5.1% in pediatric patients. |
| HA vs CA CDI Rates | Adult HA CDI decreased by 19.9%. Pediatric HA CDI decreased by 29.6%; CA rates showed stability. |
| Ribotype Changes | RT106 became the most common ribotype, replacing RT027, which was linked to severe outcomes in adults. |
| Resistance Patterns | Higher moxifloxacin resistance in adults; similar clindamycin and rifampin resistance across both groups. |
| Clinical Outcomes | Adult mortality rate: 10.6%. Pediatric mortality rate: 1.4%. Severe outcomes more frequent in adults. |
| Importance of Surveillance | Ongoing national surveillance critical for understanding CDI epidemiology and guiding prevention. |
Summary
Clostridioides difficile infection (CDI) remains a significant public health issue, with ongoing research highlighting the trends, resistance patterns, and clinical outcomes associated with HA and CA CDI in Canada. This investigation from 2015 to 2022 reveals a promising decrease in infection rates, particularly among pediatric patients, alongside a shift in prevalent ribotypes, underscoring the importance of continued surveillance and infection control measures to further mitigate this healthcare challenge.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.