Chronic pancreatitis is a serious and often painful condition that arises from long-term inflammation of the pancreas. This persistent inflammation not only disrupts the organ’s functions but can also lead to debilitating complications, such as diabetes and digestive problems. Early identification of chronic pancreatitis symptoms is critical for effective treatment and management of the disease. Common causes of chronic pancreatitis include excessive alcohol consumption, genetic predispositions, and autoimmune disorders, all of which contribute to the inflammation. Understanding chronic pancreatitis—alongside its symptoms, potential causes, and treatment options—can greatly enhance one’s ability to effectively navigate this challenging health issue.
Chronic inflammation of the pancreas, often termed persistent pancreatitis, presents a series of challenges that significantly affect both physical health and quality of life. This prolonged condition can be triggered by various factors including heavy alcohol intake, genetic abnormalities, or autoimmune responses that attack pancreatic cells. Recognizing the signs of this illness, including digestive complications and abdominal discomfort, is essential for proper pancreatitis management. Treatment strategies range from dietary modifications to enzyme replacement, offering patients multiple avenues for relief. Overall, gaining a comprehensive understanding of these chronic inflammatory processes is vital to address the impact they can have on individuals.
Recognizing the Symptoms of Chronic Pancreatitis
Chronic pancreatitis can present a multitude of symptoms that can deeply impact daily life. Among these, abdominal pain is a prevalent complaint. Patients often describe the pain as debilitating and may find it radiating to the back, stemming from the pancreas’s compromised function. Beyond pain, digestive issues like weight loss and malnutrition are prevalent, as the inflamed pancreas struggles to secrete adequate enzymes for digestion. Malabsorption, particularly of fats and fat-soluble vitamins, leaves individuals feeling fatigued and undernourished.
In addition to the physical manifestations, chronic pancreatitis can evoke psychological distress. The constant discomfort and the dietary restrictions can lead to feelings of anxiety and depression in many patients. Symptoms such as nausea and vomiting can further hinder nutrient intake, creating a vicious cycle that complicates recovery and impacts overall wellbeing. Understanding these symptoms allows for early intervention and management, essential for improving the quality of life in affected individuals.
Exploring the Causes of Chronic Pancreatitis
The causes of chronic pancreatitis are multifaceted and often interrelated. Alcohol misuse remains the primary contributor, with chronic intake leading to toxic effects that impair pancreatic function. Alongside this, genetic predispositions play a significant role; specific gene mutations can heighten susceptibility to the disease. Conditions such as hereditary pancreatitis must be recognized, particularly in younger patients who may not have a history of alcohol use.
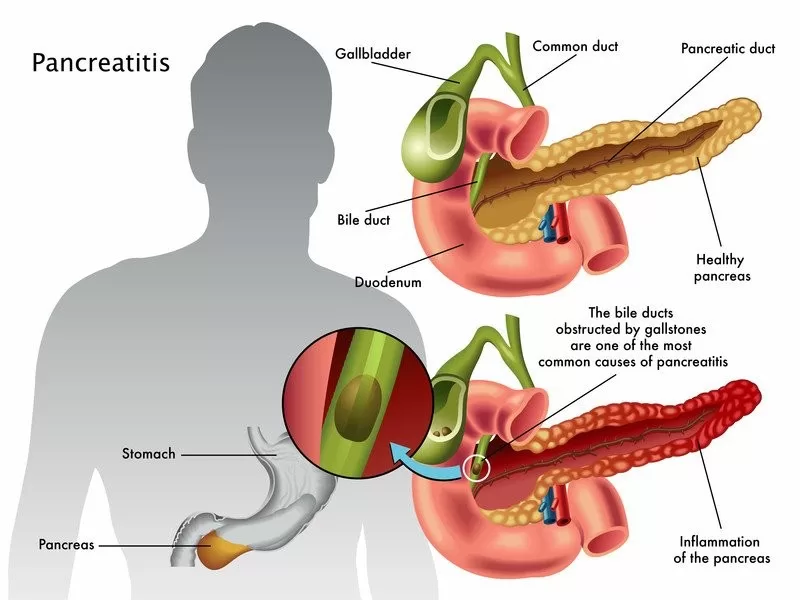
Moreover, autoimmune responses and obstructive pathologies like gallstones are also pertinent causes of chronic pancreatitis. During autoimmune pancreatitis, the body’s immune system attacks its own pancreatic cells, resulting in inflammation. Obstruction due to gallstones can lead to backpressure, further damaging pancreatic tissue. Understanding these causes is crucial not only for prevention but also for tailoring effective management strategies that address the underlying issues.
Effective Treatment Options for Chronic Pancreatitis
Given the absence of a definitive cure for chronic pancreatitis, treatments aim primarily at alleviating symptoms and enhancing quality of life. Lifestyle modifications are at the forefront, with strict adherence to alcohol abstinence and smoking cessation strongly advised. Furthermore, adopting a low-fat diet can alleviate some digestive distress, minimizing the strain placed on the pancreas. These lifestyle changes not only benefit symptom management but can also slow disease progression.
In addition to lifestyle adjustments, medical treatments such as pancreatic enzyme replacement therapy are critical for many patients. By supplementing the digestive enzymes that the injured pancreas fails to produce, patients can better absorb nutrients, combat malnutrition, and improve their overall health status. For those grappling with severe pain, pain management strategies, including medications and even nerve block procedures, become necessary. Ultimately, a comprehensive treatment approach tailored to individual needs is essential for managing this complex condition.
Dietary Management in Chronic Pancreatitis
Diet plays an instrumental role in the management of chronic pancreatitis. Patients are often advised to follow a low-fat diet that minimizes stress on the pancreas and supports healthier digestion. Foods rich in carbohydrates and proteins are recommended, while high-fat foods should be limited to avoid triggering inflammatory responses. By focusing on easily digestible foods, patients can reduce symptoms of discomfort and improve their nutrient intake.
Incorporating dietary modifications also involves being mindful of individual tolerances and preferences, as some may experience varying reactions to certain foods. A registered dietitian can be invaluable in creating personalized meal plans that cater to the unique needs of each patient. Additionally, ongoing research suggests that specific dietary interventions and adjustments, including supplementation with medium-chain triglycerides (MCTs), might further ameliorate symptoms and enhance nutrient absorption, representing a promising avenue for future dietary strategies.
Innovations and Future Directions in Chronic Pancreatitis Management
Recent advancements in chronic pancreatitis research indicate a shift towards more individualized patient care. Innovations in understanding the disease’s pathophysiology have led to new potential therapies aimed at reducing inflammation and restoring pancreatic function. For example, researchers are exploring the efficacy of new pharmacological agents that may offer patients prolonged relief from symptoms and improved quality of life.
Moreover, patient education remains a cornerstone in managing chronic pancreatitis. As healthcare professionals strive to empower patients with knowledge about their condition—such as recognizing early symptoms and implementing necessary lifestyle changes—there is great potential for improving long-term outcomes. The development of comprehensive education programs can further support individuals in navigating their health journeys, ensuring they are well-informed about available resources and the importance of proactive management.
Frequently Asked Questions
What are the common symptoms of chronic pancreatitis?
Chronic pancreatitis symptoms often include severe abdominal pain that may radiate to the back, digestive issues like unintentional weight loss and malnutrition due to enzyme deficiencies, frequent nausea and vomiting, and diabetes symptoms due to insulin production impairment.
What are the main causes of chronic pancreatitis?
The causes of chronic pancreatitis generally include prolonged alcohol use, genetic mutations affecting pancreatic function, autoimmune conditions leading to tissue inflammation, and obstructive issues such as gallstones that damage the pancreas.
What treatment options are available for managing chronic pancreatitis?
Chronic pancreatitis treatment focuses on lifestyle changes like abstinence from alcohol and smoking, following a low-fat diet, pancreatic enzyme replacement therapy, pain management strategies, and, in some cases, surgical intervention to address ductal obstructions or remove damaged tissue.
How can a diet help in the management of chronic pancreatitis?
A pancreatitis diet should emphasize low-fat food choices to reduce digestive stress on the pancreas. Additionally, patients are encouraged to adopt healthier eating habits and avoid trigger foods to alleviate symptoms and improve nutrient absorption.
What recent developments are impacting chronic pancreatitis research and treatment approaches?
Recent developments in chronic pancreatitis research are exploring the links between the condition and factors like obesity and metabolic syndrome, with an emphasis on patient education programs that highlight early warning signs and lifestyle modifications crucial for managing the disease.
| Key Points | Details | |
|---|---|---|
| Symptoms | Abdominal pain, digestive issues, nausea, and diabetes symptoms. | |
| Causes | Alcohol use, genetic factors, autoimmune conditions, and obstructive issues. | |
| Treatment Options | Lifestyle changes, enzyme replacement therapy, pain management, and surgery. | |
| Recent Developments | Research on obesity and patient education programs. | |
Summary
Chronic pancreatitis is a serious condition that requires a comprehensive understanding of its symptoms, causes, and treatment options for effective management. The inflammation of the pancreas can lead to severe abdominal pain, nutritional deficiencies, and diabetes. A multifaceted approach involving lifestyle modifications, medical therapies, and ongoing research is essential for improving the quality of life for those affected by chronic pancreatitis. It is important for patients to stay informed and work closely with healthcare providers to navigate this challenging condition.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.