Chest pain types can vary widely in nature and severity, making it an essential topic for anyone concerned about their health. From the alarming sensations associated with cardiac distress to the less serious manifestations due to gastrointestinal or musculoskeletal issues, understanding these variations is crucial. Symptoms of chest pain can often be perplexing, leading individuals to wonder if they are experiencing a life-threatening condition or something benign. Differentiating chest pain—whether cardiac versus non-cardiac—can significantly impact treatment decisions and outcomes. Knowing when to seek medical help can save lives, empowering patients with the knowledge required to respond appropriately to their symptoms.
Chest discomfort comes in various forms and can pose different challenges for individuals trying to identify the cause. Ranging from acute pressure indicative of heart issues to the gnawing pains reminiscent of digestive trouble, recognizing these disparate feelings is vital for effective response. Understanding the root of these sensations—be it heart-related or stemming from lung, gastrointestinal, or musculoskeletal origins—can help guide a patient’s next steps. Moreover, comprehending the urgency of seeking medical assistance when faced with chest pain is crucial. By familiarizing ourselves with these alternative terms and their implications, we enhance our ability to navigate potential health crises.
Types of Chest Pain: An Overview
Chest pain can be categorized into two primary types: cardiac and non-cardiac. Cardiac pain is most alarming due to its association with heart conditions such as angina and myocardial infarction. Angina presents as a squeezing sensation in the chest, often triggered by physical exertion or emotional stress, and it signals reduced blood flow to the heart. Meanwhile, a myocardial infarction signals a full blockage of blood flow, typically characterized by acute, intense pain that may radiate to other areas of the body, accompanied by symptoms like sweating and shortness of breath.
Non-cardiac chest pain, often less critical but still concerning, arises from different bodily systems. Gastrointestinal issues, such as GERD, can cause burning sensations in the chest that may be mistaken for heart pain. Musculoskeletal injuries, including costochondritis, yield localized pain that worsens with movement. Recognizing these distinctions is vital for determining the appropriate response to chest pain.
Understanding the Symptoms of Chest Pain
The symptoms of chest pain vary widely depending on its underlying cause. Cardiac chest pain typically includes a sense of heaviness or tightness in the chest, which might extend to the arms, neck, or jaw. It can also occur alongside other symptoms such as breathlessness, cold sweats, or nausea. In contrast, non-cardiac conditions exhibit different symptoms; for example, gastrointestinal pain may present with heartburn or a bitter taste in the mouth, while musculoskeletal pain usually feels sharp and localized.
It’s important for individuals to educate themselves on these varying symptoms. When experiencing chest pain, taking note of how it feels, its duration, and any additional accompanying symptoms can inform healthcare professionals and assist in a proper diagnosis and treatment plan. Identifying these symptoms early can be lifesaving, especially when cardiac issues are involved.
Causes of Chest Pain: A Comprehensive Guide
Chest pain can arise from a vast array of causes, which can be divided into cardiac and non-cardiac origins. Cardiac causes usually stem from issues like coronary artery disease, which narrows the arteries and limits blood flow to the heart, leading to conditions such as angina or heart attacks. Additionally, inflammation of the heart lining, known as pericarditis, can present as sharp, severe chest pain that worsens with deep breathing.
On the other hand, non-cardiac causes of chest pain are also numerous. Gastrointestinal disorders, such as peptic ulcers or reflux disease, can lead to similar discomfort as heart attacks. Furthermore, lung-related issues like pneumonia and pulmonary embolism can also be mistaken for cardiac pain due to overlapping symptoms. Recognizing these causes not only helps in managing pain effectively but also in determining when medical attention is necessary.
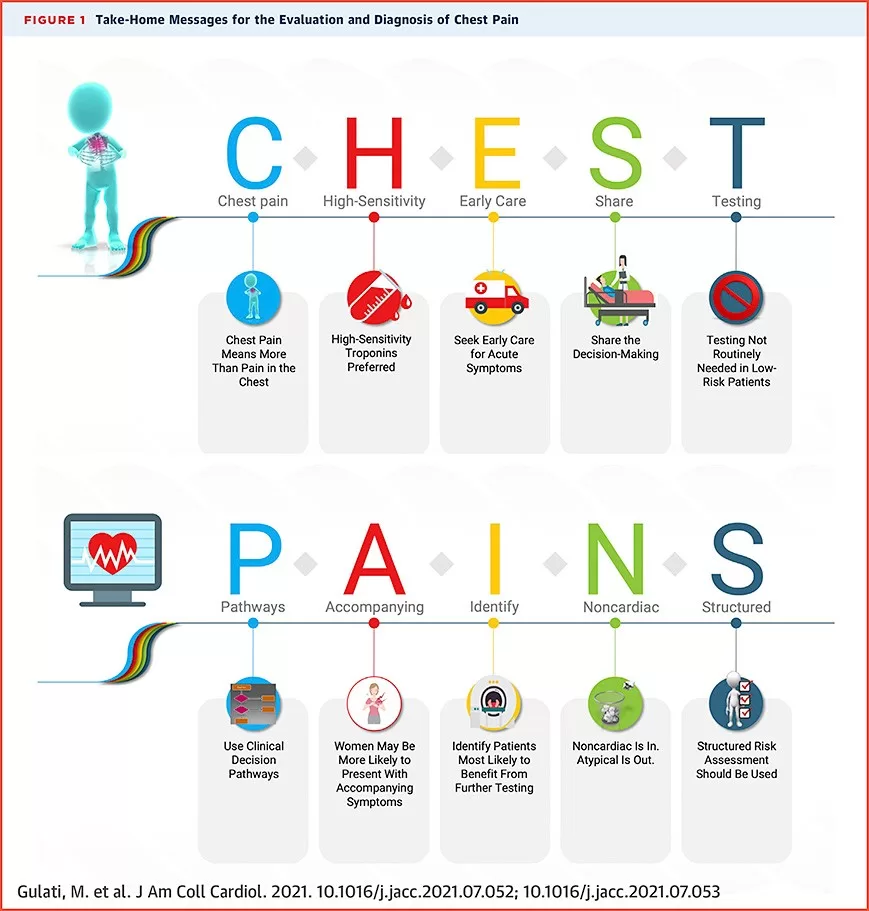
Cardiac versus Non-Cardiac Pain: Key Differences
Differentiating between cardiac and non-cardiac pain is crucial for proper treatment. Cardiac pain is often described as an intense pressure, heaviness, or tightness, frequently accompanied by radiating sensations to the arms, back, or jaw. Patients may also experience palpations and extreme fatigue. In contrast, non-cardiac pain often has distinct characteristics, such as a sharp or burning sensation, and it may change with position or movement, which is uncommon with cardiac pain.
The onset and triggers of pain can also provide insights into its origin. While cardiac pain may occur suddenly during rest or exertion, non-cardiac pain may correlate with eating habits or certain activities. Understanding these nuances can empower individuals to assess their symptoms more accurately, ensuring timely medical intervention when necessary.
When to Seek Medical Help for Chest Pain
Recognizing when to seek medical attention is paramount for individuals experiencing chest pain. Immediate medical help is warranted if the pain is sudden, severe, or accompanies symptoms such as shortness of breath, dizziness, sweating, or nausea. Even if initial pain subsides, it is still crucial to consult healthcare professionals, especially if it resembles any previously experienced chest discomfort.
Early intervention can significantly impact treatment outcomes, particularly for cardiac-related conditions. Individuals should not dismiss chest pain or assume it will resolve on its own. The complexities surrounding chest pain necessitate a cautious approach, where erring on the side of caution can make the difference between life and death in severe cases.
Frequently Asked Questions
What are the common symptoms of chest pain and how do they differ between cardiac and non-cardiac causes?
The symptoms of chest pain can vary widely depending on the cause. Cardiac pain, often linked to conditions like angina and heart attack, typically feels like pressure, squeezing, or tightness in the chest, often radiating to the arms, neck, or jaw. Non-cardiac chest pain, on the other hand, may include sharp, burning sensations commonly associated with gastrointestinal issues like GERD or musculoskeletal conditions, which usually hurt more with movement or pressure. Recognizing the symptoms of chest pain types can aid in seeking timely medical advice.
How can I differentiate between cardiac versus non-cardiac chest pain?
Differentiating chest pain types is crucial for appropriate treatment. Cardiac pain often presents as a heavy or crushing sensation, particularly during exertion or stress, and may involve additional symptoms like sweating, nausea, or shortness of breath. In contrast, non-cardiac pain, related to gastrointestinal disorders or musculoskeletal issues, may feel more localized and could intensify with certain movements or eating. Understanding these distinctions helps determine when to seek medical help.
What are some common causes of chest pain that are not related to heart issues?
Many causes of chest pain are not heart-related. Gastrointestinal problems such as GERD can lead to burning sensations, while esophageal spasms may cause sharp pain. Musculoskeletal pain can arise from injuries to the chest wall, and lung conditions like pneumonia or pulmonary embolism can also present with chest pain. Being aware of these non-cardiac causes can help alleviate anxiety and guide the decision of when to seek medical help.
When should I seek medical help for chest pain?
It is essential to seek medical help for chest pain if it is sudden and severe, accompanied by shortness of breath, or associated with symptoms such as dizziness, nausea, or sweating. If the pain persists or worsens over time, immediate consultation with a healthcare professional is crucial, as it may indicate a serious condition, whether cardiac or non-cardiac. Knowing when to seek medical assistance can be lifesaving.
How can understanding chest pain types improve my health outcomes?
Understanding the various chest pain types enhances your ability to identify symptoms accurately, differentiating between potentially serious cardiac issues and common non-cardiac problems. This knowledge empowers you to make informed decisions regarding when to seek medical help, leading to timely interventions that can significantly improve health outcomes. Staying informed means prioritizing your health and well-being.
| Type of Chest Pain | Description | Common Causes |
|---|---|---|
| Cardiac Pain | Heavy pressure or squeezing sensation, possibly radiating to other areas. | Angina, Myocardial Infarction (Heart Attack). |
| Gastrointestinal Pain | Sharp or burning sensation, often after meals or when lying down. | GERD, Esophageal Spasms. |
| Musculoskeletal Pain | Localized pain that worsens with movement or pressure. | Costochondritis, muscle strain. |
| Lung-Related Conditions | Sharp chest pain, worsens with deep breaths or coughing. | Pneumonia, Pulmonary Embolism. |
| Psychological Factors | Chest tightness, rapid heartbeat, may mimic heart attack symptoms. | Panic attacks, anxiety disorders. |
Summary
Chest pain types can significantly affect how individuals respond to their health concerns. By recognizing the different types of chest pain, such as cardiac, gastrointestinal, musculoskeletal, lung-related, and psychological factors, patients and healthcare providers can better determine the appropriate course of action. It is essential to understand the specific characteristics that differentiate these pain types, which helps in identifying whether medical assistance is urgently needed. By being informed and vigilant about chest pain types, individuals can ensure they prioritize their health and seek timely intervention when necessary.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.