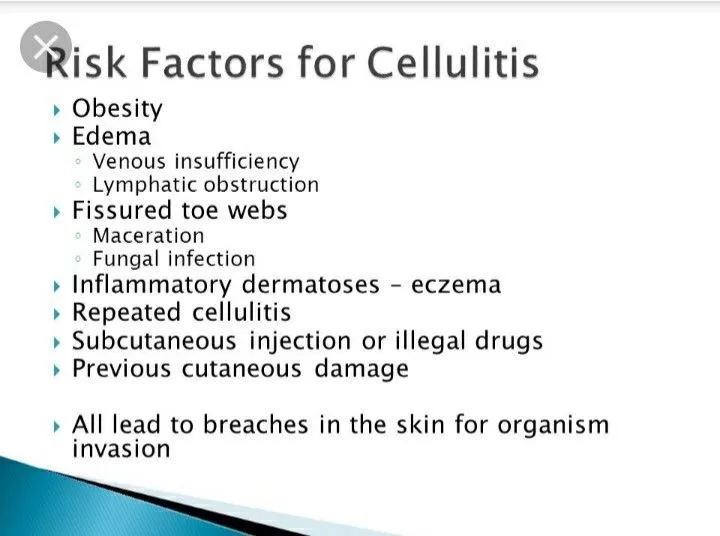
Cellulitis is a bacterial skin infection that poses a significant risk, particularly for individuals with certain predisposing factors. Understanding the risk factors for cellulitis is crucial in preventing this painful condition and avoiding the associated complications. Factors such as a weakened immune system, chronic skin issues, diabetes, and obesity can dramatically increase the chances of developing this skin infection. Moreover, gaining knowledge about the causes of cellulitis will empower you to take actionable steps towards preventing cellulitis by managing these risk factors effectively. This article will explore each risk factor in detail and provide insights into managing cellulitis symptoms and treatment options.
When we consider skin infections like cellulitis, it’s important to recognize the underlying vulnerabilities that elevate one’s risk. The term “cellulitis risk factors” encompasses various elements, including immune deficiencies and chronic dermatological conditions, which set the stage for bacterial invasion. Additionally, factors such as obesity, diabetes, and even age can contribute significantly to an individual’s susceptibility to skin infections. Understanding these interrelated aspects not only aids in identifying potential risks but also emphasizes the importance of proactive measures in managing and preventing serious complications associated with cellulitis. By exploring these topics deeply, individuals can arm themselves with the knowledge needed to safeguard their skin health.
Identifying Common Causes of Cellulitis
Understanding the common causes of cellulitis is crucial when addressing this bacterial skin infection. Generally, cellulitis occurs when bacteria such as Staphylococcus and Streptococcus penetrate the skin through cuts, abrasions, or insect bites. Individuals with conditions that impair skin integrity—like eczema, psoriasis, or any open wounds—are particularly susceptible. Studies emphasize the importance of keeping the skin clean and protected, especially for those with existing skin conditions. This proactive approach helps minimize the potential for bacteria to enter the skin.
In addition to direct skin breaches, other causative factors play a significant role. Diabetes, for instance, impairs the body’s immune response and blood circulation, making individuals more vulnerable. Poorly managed diabetes not only provides an environment for bacteria to thrive but can also mask the symptoms due to nerve damage. For prevention, it’s vital for diabetic patients to monitor their skin condition closely and consult with healthcare providers for routine check-ups.
Preventing Cellulitis: Practical Strategies
Preventing cellulitis requires a proactive approach to skin care and health management. Maintaining good hygiene is one of the most effective strategies to ward off bacterial infections. Individuals should regularly wash their skin, especially areas prone to cuts and abrasions, and apply moisturizers to enhance skin barrier function. Furthermore, it’s advisable to cover any minor injuries with clean bandages until they heal completely, thus minimizing the risk of bacterial entry.
For individuals at higher risk, such as those with a family history of skin infections, chronic conditions, or the elderly, taking preventive measures becomes even more vital. Regular check-ups with healthcare providers can help monitor for early signs of skin infections or other health concerns. Additionally, controlling underlying health issues like obesity and diabetes can significantly lower the likelihood of experiencing cellulitis.
Recognizing Cellulitis Symptoms Early
Recognizing the symptoms of cellulitis early is crucial for effective treatment and recovery. Common symptoms include redness, swelling, warmth in the affected area, and potential pain. In more severe cases, individuals may experience fever or chills, indicating that the infection is spreading. Being vigilant about these symptoms can facilitate timely medical intervention, which is paramount in preventing complications. Individuals should not hesitate to seek medical advice if they notice any unusual skin changes.
Furthermore, understanding the progression of cellulitis symptoms can aid individuals in differentiating between minor skin irritations and a more serious infection. A clear understanding of symptoms can empower individuals to act swiftly—such as contacting a healthcare provider as soon as noticeable changes occur. This proactive response can prevent the escalation of cellulitis and aid in expedited treatment.
Cellulitis Treatment Options Explained
Treatment for cellulitis typically involves the use of antibiotics to target the underlying bacterial infection. The choice of antibiotic may depend on the severity of the infection, the patient’s overall health, and any contributing factors, such as diabetes or immunocompromised status. In milder cases, oral antibiotics may suffice, while more severe infections may necessitate intravenous antibiotics administered in a hospital setting. Understanding available treatment options equips individuals with knowledge for discussions with their healthcare providers.
In addition to antibiotics, supplementary treatments may be recommended to help manage symptoms and promote healing. These can include elevating the affected limb to reduce swelling and applying cool, damp cloths to soothe discomfort. Thoroughly following healthcare professionals’ directives regarding medication and care can significantly enhance recovery speed and reduce the risk of recurrent cellulitis.
Understanding Cellulitis Risk Factors: Who is Most Vulnerable?
Understanding cellulitis risk factors is essential to identify populations that may need more vigilance in skin care and health management. Individuals with weakened immune systems—whether due to chronic illnesses, medications like chemotherapy, or conditions such as HIV/AIDS—are at heightened risk because their bodies can’t adequately fight off infections. This underscores the necessity for maintaining intact skin and promptly addressing any minor wounds.
Moreover, common chronic conditions like diabetes put individuals at an increased risk for cellulitis. High blood sugar can hinder healing and may lead to nerve damage, making it difficult for individuals to notice wounds. Consequently, managing blood sugar levels and practicing diligent foot care are critical for prevention. Identifying these risk factors empowers individuals and caregivers to take proactive measures against potential skin infections.
Frequently Asked Questions
What are the primary risk factors for cellulitis development?
The primary risk factors for cellulitis include a weakened immune system, chronic skin conditions such as eczema and psoriasis, diabetes, obesity, and advanced age. These factors can compromise skin integrity and make it easier for bacteria to enter the skin, increasing the risk of cellulitis.
How does diabetes contribute to the risk of developing cellulitis?
Diabetes significantly raises the risk of cellulitis due to high blood sugar levels that impair the body’s infection-fighting capabilities. Additionally, diabetes can cause peripheral neuropathy, which reduces sensation in the extremities, making it difficult for individuals to notice wounds that can lead to cellulitis.
Can chronic skin conditions increase the risk of cellulitis?
Yes, individuals with chronic skin conditions like eczema or psoriasis have a higher risk of cellulitis. These conditions can damage the skin barrier, allowing bacteria to enter more easily. Proper management of these skin issues through good hygiene and treatment is crucial in preventing cellulitis.
In what ways does obesity influence the risk of skin infections like cellulitis?
Obesity can increase the risk of cellulitis due to poor circulation and skin integrity issues. Skin folds in obese individuals create warm, moist environments that facilitate bacterial growth. Maintaining a healthy weight through diet and exercise can help reduce the likelihood of cellulitis.
What steps can I take to prevent cellulitis if I have a history of the infection?
If you have a history of cellulitis, it’s essential to take preventive measures such as keeping your skin clean and moisturized, managing any underlying health conditions, and seeking medical advice for any skin injuries. Regular check-ups with healthcare providers can help monitor your skin health and mitigate the risk of recurrent cellulitis.
| Risk Factor | Description |
|---|---|
| Weakened Immune System | Conditions like HIV/AIDS and cancer can impair the body’s ability to fight infections. |
| Chronic Skin Conditions | Eczema, psoriasis, and fungal infections weaken the skin barrier, making infections more likely. |
| Diabetes | Impaired defense mechanisms and potential loss of sensation can lead to unnoticed wounds. |
| Obesity | Poor circulation and skin integrity issues create a warm environment for bacterial growth. |
| Age | Thinning skin and impaired immune function increase susceptibility to infections. |
| Previous Instances of Cellulitis | A history of cellulitis raises the risk of future infections due to weakened skin defenses. |
| Edema and Lymphatic Obstruction | Swelling from fluid retention can distort the skin, making it more susceptible. |
| Intravenous Drug Use | Skin punctures from injections can introduce bacteria, increasing infection risk. |
Summary
Cellulitis risk factors are crucial to understand for effective prevention and treatment. Various factors, including a weakened immune system, chronic skin conditions, diabetes, obesity, and age, significantly elevate the likelihood of developing cellulitis. By staying vigilant and maintaining skin integrity through proper hygiene and regular healthcare consultations, individuals can significantly reduce their risk of contracting this bacterial skin infection. Being informed about these risk factors empowers people to act proactively in safeguarding their health.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.