Bacterial infections with Flu and RSV pose significant health challenges, as a recent study has revealed a higher prevalence of concomitant bacterial infections in patients suffering from these viral infections compared to those with SARS-CoV-2. Researchers found that individuals infected with influenza and respiratory syncytial virus (RSV) are at a markedly elevated risk of secondary infections, which can complicate their clinical outcome. Specifically, the study pointed out the critical need for robust antimicrobial stewardship during the COVID-19 pandemic, given the increased incidence of bacterial co-infections. This highlights the necessity of understanding the RSV pneumonia risk, as not only flu but also RSV infections significantly contribute to bacterial complications. Overall, the findings underscore the importance of careful monitoring and treatment in patients with influenza and RSV to mitigate the dangers associated with bacterial infections.
Understanding the dynamics of bacterial infections alongside viral illnesses such as influenza and respiratory syncytial virus (RSV) is crucial for effective patient management. These viral infections can lead to secondary bacterial complications, making it essential for healthcare providers to recognize the increased risk associated with these conditions. Comparative studies highlight that flu, in particular, has a notable association with bacterial co-infections, further complicating the clinical picture and necessitating targeted treatment strategies. The implications for antimicrobial stewardship during outbreaks of respiratory illnesses, including COVID-19, cannot be understated, as inappropriate antibiotic use can lead to increased antimicrobial resistance. Proper recognition of these co-infections will aid in better treatment outcomes and enhance our understanding of the interplay between viruses and bacterial pathogens.
The Prevalence of Bacterial Infections in Viral Respiratory Illnesses
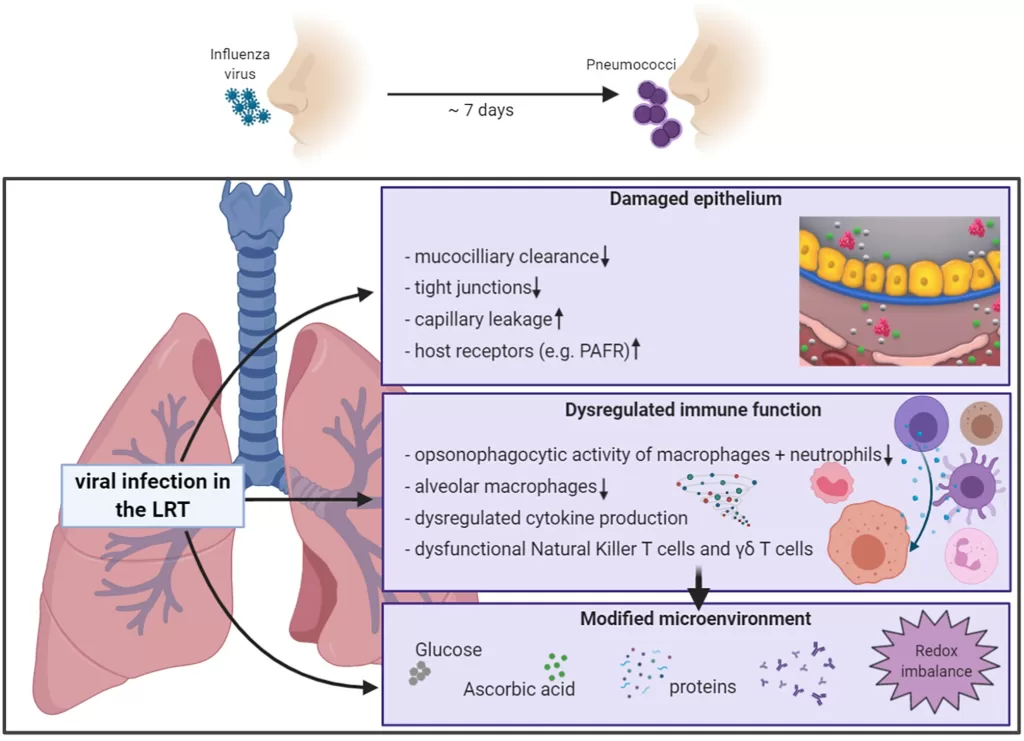
Recent studies, including one conducted in Ontario, illustrate a noteworthy prevalence of bacterial infections occurring alongside viral respiratory infections such as influenza and respiratory syncytial virus (RSV). These infections can complicate the clinical presentation and management of patients. For instance, during the observed period from 2017 to 2019, nearly 0.5% of the 885,004 recorded respiratory viral infections were linked to concomitant bacterial infections. This highlights the critical need for healthcare providers to be vigilant in monitoring these complications, particularly in patients presenting with FLUA and FLUB.
The types of bacteria identified as common pathogens included *Staphylococcus aureus*, *Streptococcus pyogenes*, and *Pseudomonas aeruginosa*. The findings underscore the importance of understanding the interplay between viral and bacterial pathogens, as this knowledge can influence treatment decisions. A nuanced approach to managing these infections, considering factors like the timing of bacterial infection in relation to viral onset, is essential in reducing both morbidity and the potential for adverse outcomes.
Bacterial Infections with Flu and RSV: A Comparative Analysis
When comparing the risks of bacterial infections associated with influenza and RSV, the data reveals varied outcomes which may influence clinical practices. The study reported an odds ratio of 2.30 for FLUB and 1.56 for RSV when matched against SARS-CoV-2, suggesting that patients infected with influenza and RSV are at a greater risk for co-infections. This comparative analysis is critical as it can help inform tailored therapeutic strategies that consider the bacterial etiologies prevalent in patients with these viral infections.
Furthermore, understanding these risks can lead to improved antimicrobial stewardship through more accurate diagnosis and treatment planning. The findings suggest that while SARS-CoV-2 patients may have a higher risk for secondary infections, their odds for co-infections remain comparatively lower. This insight is essential in shaping guidelines for empirical antibiotic therapy, especially in non-critically ill patients, to prevent unnecessary antibiotic use which can escalate the issue of antimicrobial resistance.
The Role of Antimicrobial Stewardship in COVID-19 Management
Antimicrobial stewardship has become a focal point in managing COVID-19, particularly given the evidence of secondary bacterial infections associated with the virus. The recent study highlights that while patients with COVID-19 have a lower risk of co-infections relative to those with influenza or RSV, the relatively significant risk for secondary infections calls for careful considerations in prescribing practices. The study authors stress that early empiric prescribing for COVID-19 patients is unwarranted unless supported by clear clinical indicators of bacterial infection.
This knowledge compels healthcare practitioners to balance the risks of under-treatment and the rise of antimicrobial resistance. Educating healthcare professionals about appropriate antibiotic use and reinforcing guidelines governing empirical antibiotic therapy is vital. Such strategic interventions can enhance patient outcomes without contributing to the growing threat of antimicrobial resistance, especially in the context of respiratory infections like SARS-CoV-2.
Understanding Concomitant Infections: Clinical Implications and Management
The study’s insights into concomitant infections provide invaluable information for clinicians managing patients with viral respiratory infections. Recognizing the patterns of bacterial infections associated with influenza and RSV can lead to more vigilant monitoring and prompt treatment when necessary. The distinction between co-infection and secondary infection as defined by the timing of bacterial onset post-viral infection offers a framework for clinical decision-making.
Implementation of proactive screening measures and targeted treatment efforts for patients at higher risk of concomitant infections can significantly improve clinical outcomes. This is particularly important given the diverse bacterial flora that can complicate standard viral infections, thus necessitating comprehensive treatment plans that integrate both viral and bacterial management.
Patient Characteristics Influencing the Risk of Bacterial Infections
The study has also shed light on how patient characteristics, such as age and underlying health conditions, influence the risk of bacterial infections in respiratory illness cases. For example, older adults and those with comorbidities often show increased susceptibility to bacterial pathogens following viral infections. Understanding these demographics is crucial for tailoring preventative and therapeutic strategies.
This personalized approach not only improves the management of acute infections but also supports broader public health initiatives aimed at controlling bacterial resistance. For instance, elderly individuals with influenza or RSV require closer monitoring for bacterial co-infections, thereby allowing for timely interventions that can alter the course of their treatment and improve their overall outcomes.
Assessing the Risks of Influenza Secondary Infections
Secondary infections in patients who have contracted influenza represent a significant concern in clinical settings, underscoring the importance of informed clinical assessments. The adjusted odds for bacterial infections in FLUB patients were found to be much higher compared to those for SARS-CoV-2, reflecting the need for enhanced vigilance during the flu season. Healthcare providers must be aware of these trends and ready to act quickly in diagnosing and managing these secondary infections to mitigate potential complications.
Analyzing influenza’s propensity to lead to bacterial infections can influence vaccine strategies, prompting discussions about the broader implications of flu vaccination in preventing not just the flu, but also consequently related bacterial infections. Enhanced vaccine campaigns, especially targeting high-risk populations, become an essential public health response to minimize the incidence of secondary infections during flu outbreaks.
Coinfection Dynamics: Insights for Future Research
The findings regarding coinfection dynamics present a vital area for future research and public health planning, especially in the face of emerging infectious diseases. The nuances related to timing—whether bacterial infections occur within days of a viral infection or after—highlight the complex interactions between pathogens. Continued studies into how various strains of viruses interact with bacterial pathogens will provide deeper insights necessary for formulating effective treatment protocols.
Moreover, the evaluation of environmental and biological factors that contribute to the likelihood of coinfections could lead to more targeted epidemiological strategies. Significant output from such research could transform clinical practice by identifying risk factors that predict concomitant infections, enhancing overall patient care while addressing antimicrobial resistance as a byproduct of more efficient management.
The Impact of Concomitant Infections on Healthcare Systems
Concomitant infections not only affect individual patient outcomes but also present substantial challenges to healthcare systems. The increased incidence of secondary infections in patients with viral respiratory diseases leads to higher hospitalization rates and prolonged healthcare resource utilization. These factors place additional burdens on an already strained system, particularly during peak flu seasons or public health crises like the COVID-19 pandemic.
Addressing the healthcare implications of concomitant infections emphasizes the need for system-wide strategies, including improved surveillance and integrated care approaches. By bolstering infectious disease protocols and ensuring that healthcare infrastructures can adapt to changing infection dynamics, systems can better respond to both current and future respiratory infection challenges.
Conclusion: The Need for Comprehensive Infection Management Strategies
The study’s results advocate for a comprehensive approach to managing respiratory infections, highlighting the interconnectedness of viral and bacterial pathogens. Effective treatment protocols must consider the potential for concomitant infections, especially in vulnerable populations. Integrating findings from current research into practical guidelines will enable healthcare providers to deliver more precise care that is responsive to the complexities of these infections.
As we navigate the evolving landscape of infectious diseases, continued emphasis on research, education, and preventive strategies will be fundamental in curbing both the incidence of respiratory infections and their associated bacterial complications. This holistic perspective on patient care can ultimately lead to better health outcomes while supporting public health efforts to combat the rise of antibiotic resistance.
Frequently Asked Questions
What is the relationship between bacterial infections and influenza and RSV?
Bacterial infections can commonly accompany viral infections such as influenza (FLUA and FLUB) and respiratory syncytial virus (RSV). A recent study found that patients with flu and RSV have a higher prevalence of concomitant bacterial infections compared to those with SARS-CoV-2, emphasizing the importance of monitoring and treating these secondary infections.
How do bacterial infections with FLUA differ from those with RSV and SARS-CoV-2?
According to a study, patients with FLUA show a 4.7% incidence of concomitant bacterial infections, which is higher compared to RSV at 3.4%. In contrast, the incidence for SARS-CoV-2 is significantly lower at 0.3%. This indicates that patients with influenza are at a greater risk for additional bacterial infections than those infected with SARS-CoV-2.
What are the most common bacteria involved in secondary infections following FLUA and RSV?
The study revealed that the most prevalent bacteria causing concomitant infections in patients with FLUA and RSV included *Staphylococcus aureus*, *Streptococcus pyogenes*, and *Pseudomonas aeruginosa*. Understanding these common pathogens is essential for effective treatment planning and antimicrobial stewardship.
What is the risk of secondary infections in COVID-19 patients compared to those with influenza or RSV?
While patients with COVID-19 have a lower risk of co-infections immediately after infection compared to those with influenza or RSV, the risk of developing secondary bacterial infections increases significantly after 48 hours. This highlights the need for careful monitoring and possible treatment options for COVID-19 patients who may develop these infections.
How can antimicrobial stewardship be improved in patients with viral infections like flu and RSV?
Antimicrobial stewardship can be enhanced by recognizing the low risk of concurrent bacterial infections in influenza and RSV patients. The study suggests that empirical antibiotic therapy should be administered cautiously, particularly in non-critically ill patients with COVID-19, to avoid unnecessary antibiotic use that could contribute to antimicrobial resistance.
What does the term ‘concomitant infections study’ refer to in the context of FLUA and RSV?
The term ‘concomitant infections study’ refers to research that investigates the occurrence of bacterial infections alongside viral infections such as influenza and RSV. The findings show a distinct prevalence and risk profile for bacterial infections in these patients, providing valuable insights for clinical practices and treatment strategies.
| Key Points |
|---|
| A population-based study in Ontario analyzed bacterial infections alongside viral infections including influenza, RSV, and SARS-CoV-2. |
| The study found that Flu and RSV patients had a higher prevalence of bacterial infections than those with SARS-CoV-2. |
| From 885,004 observations, 4,230 were related to concomitant bacterial infections, with significant rates in FLUB and FLUA patients compared to COVID-19 patients. |
| The most common bacterial pathogens involved were *Staphylococcus aureus*, *Streptococcus pyogenes*, and *Pseudomonas aeruginosa*. |
| The odds of secondary bacterial infections were found to be higher in SARS-CoV-2 patients after 48 hours compared to other viral infections. |
| Findings indicate a need for careful antibiotic prescribing to avoid worsening antimicrobial resistance. |
Summary
Bacterial infections with Flu and RSV represent a significant public health concern, particularly given the findings from a recent study that highlights their increased likelihood compared to SARS-CoV-2. The implications of these results underscore the importance of antimicrobial stewardship in treating viral infections, focusing on avoiding unnecessary antibiotic prescriptions in patients with low risks of bacterial co-infections. Understanding the dynamics of these simultaneous infections is crucial for healthcare providers when making treatment decisions.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.