Artemisinin resistance presents a growing challenge in our fight against malaria, specifically in relation to *Plasmodium falciparum*, which is known for its severe impact on global health. In Southeastern Sudan, a recent study revealed alarming statistics, where 22% of *P. falciparum* samples contained the pfkelch13 R622I mutation—an indicator of compromised efficacy against artemisinin-based therapies. This situation is further complicated by the emergence of malaria drug resistance and the prevalence of HRP2 diagnostic deletions, which hinder accurate detection of infections. As the presence of these resistant strains expands, understanding the implications becomes crucial for malaria control initiatives in the Horn of Africa. Stakeholders must prioritize surveillance and develop strategies to combat the effects of artemisinin resistance to safeguard public health.
The phenomenon of resistance to artemisinin highlights a critical concern in malaria management, particularly as it pertains to *Plasmodium falciparum* infections. This situation is evident in regions such as Southeastern Sudan, where alternative pathways for parasite survival, linked to mutations such as Pfkelch13, threaten effective treatment outcomes. The rise of drug resistance, alongside challenges in diagnostic reliability due to HRP2 deletions, underscores the complexity of current malaria control efforts. As we delve deeper into the mechanisms behind these mutations and their effects on malaria drug efficacy, it becomes imperative to understand the broader implications for public health in endemic regions. Addressing these issues requires a multifaceted approach, incorporating both ongoing research and effective public health strategies.
Understanding Artemisinin Resistance in Plasmodium falciparum
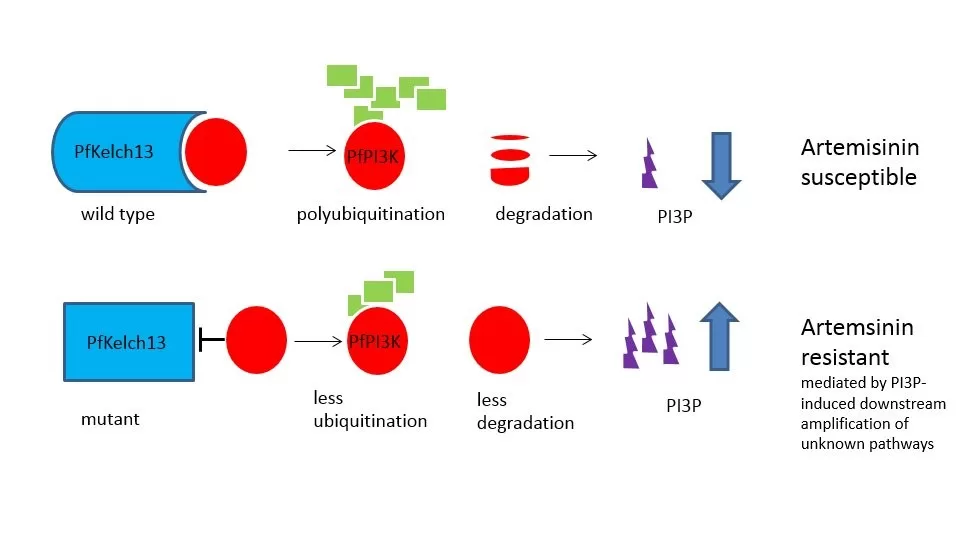
Artemisinin resistance in *Plasmodium falciparum* has emerged as a critical concern for malaria control efforts. Resistance to artemisinin-based therapies jeopardizes years of progress made in reducing morbidity and mortality associated with malaria. The identification of the Pfkelch13 mutation, particularly the R622I variant, has been instrumental in understanding how this resistance manifests. This mutation results in altered responses to treatment, thereby prolonging the duration of infection and increasing the risk of complications and severe disease.
The mechanisms underlying artemisinin resistance are complex and multifaceted. Several studies, including those conducted in southeastern Sudan, showcase the prevalence of these mutations and their implications for treatment protocols. Notably, the persistence of parasites with resistance mutations can lead to therapeutic failures, necessitating adjustments in malaria management strategies. Surveillance and continuous monitoring of these genetic markers are essential to develop effective countermeasures against drug-resistant strains.
The Impact of Pfkelch13 Mutation on Malaria Treatment
The Pfkelch13 mutation is a significant factor in the context of malaria treatment, especially with regards to artemisinin-based combination therapies (ACTs). The R622I variant of this gene has been shown to confer resistance to artemisinin, complicating therapeutic outcomes. In southeastern Sudan, approximately 22% of *Plasmodium falciparum* isolates were found to possess this mutation, indicating a concerning trend that could disrupt malaria control in the region. Given the reliance on ACTs, understanding the prevalence of such mutations is imperative for healthcare providers.
Moreover, the presence of the Pfkelch13 mutation suggests that not only are the current treatment regimens under threat, but also the potential for increased transmission rates. In areas where these mutants are prevalent, achieving effective treatment could require more intensive monitoring and potentially alternative therapeutic strategies. Thus, the urgent response to the emergence of Pfkelch13 mutations, particularly in high-burden areas, is critical for global health initiatives aimed at malaria elimination.
Compounding the challenge presented by the Pfkelch13 mutation is the dissemination of HRP2 diagnostic deletions among *Plasmodium falciparum* populations. This further complicates disease detection and management, as the rapid diagnostic tests (RDTs) that are commonplace may yield false-negative results. The intersection of genetic mutations, such as Pfkelch13, with diagnostic issues emphasizes the need for enhanced surveillance and timely interventions across the affected regions.
Malaria Drug Resistance and its Consequences
The emergence of malaria drug resistance poses serious consequences for public health, hampering prevention and treatment efforts in endemic regions. *Plasmodium falciparum* exhibits resistance not only to artemisinin but also to other antimalarial medications such as sulfadoxine and pyrimethamine. This dual resistance results in increased treatment failures and necessitates a reevaluation of existing protocols to manage malaria effectively. Southeast Sudan has seen a rise in these resistant strains, highlighting the geographical nuances of malaria epidemiology.
The impact of drug resistance extends beyond individual patient outcomes; it poses significant challenges to malaria control programs, potentially leading to increased transmission and morbidity. As resistance spreads, the effectiveness of standard treatment regimens diminishes, thereby straining healthcare resources. Global health organizations must adapt their strategies to tackle these challenges, emphasizing research, funding for new drug development, and localized strategies to combat resistance in specific regions.
HRP2 Diagnostic Deletions and Their Implications
HRP2 deletions in *Plasmodium falciparum* present a major issue for malaria diagnosis, particularly in high-burden areas like southeastern Sudan. The presence of these genetic deletions can lead to the failure of rapid diagnostic tests (RDTs), resulting in erroneous assessments of malaria prevalence and patient management. In the study, it was revealed that 10.7% of the collected samples exhibited hrp2/3 deletions, complicating the overall diagnostic landscape further and potentially prolonging outbreaks.
These diagnostic challenges underscore the necessity for improved molecular diagnostics that can reliably identify the presence of *Plasmodium falciparum*, regardless of hrp2 status. Failure to address this issue may lead to ineffective treatment regimens being administered, contributing to continued transmission and difficulty in controlling malaria outbreaks. Strategic efforts are required to ensure that diagnostic tools evolve with the changing landscape of drug resistance, thus empowering healthcare professionals to make informed clinical decisions.
The Role of Enhanced Surveillance in Malaria Control
Enhanced surveillance is paramount in the fight against emerging malaria threats, notably artemisinin resistance in *Plasmodium falciparum*. As mutations like Pfkelch13 proliferate within populations, ongoing monitoring becomes crucial for timely intervention and management. In southeastern Sudan, establishing robust surveillance systems can help detect resistance patterns early, providing critical data that informs treatment protocols and public health strategies. Such systems allow for the rapid adjustment of therapeutic regimens, ensuring that the burden of malaria continues to be mitigated.
Furthermore, integrating molecular diagnostics into these surveillance efforts can simultaneously address the challenges posed by HRP2 deletions by providing more accurate estimates of malaria prevalence. By incorporating detailed genetic analyses, health authorities can better understand the dynamics of resistance, evaluate the effectiveness of current treatments, and strategize future interventions. The outcome of enhanced surveillance can have profound impacts on controlling malaria transmission and efficacy of treatments in regions heavily affected by *Plasmodium falciparum*.
Challenges of Malaria Management in Southeastern Sudan
Southeastern Sudan faces unique challenges in malaria management, primarily driven by the emergence of drug resistance and the inability of current diagnostic tools to accurately detect malaria infections. The region, known for its high malaria transmission rates, has reported alarming levels of *Plasmodium falciparum* with significant resistance markers including the Pfkelch13 R622I mutation and HRP2 deletions. These challenges necessitate targeted interventions that address both treatment efficacy and diagnostic accuracy, critical for the region’s health infrastructure.
Additionally, the limited access to healthcare facilities and resources compounds the issue of managing malaria effectively. Without proper infrastructure and training, healthcare workers may struggle to implement the necessary strategies to combat resistant strains. Efforts must focus on strengthening local health systems, equipping them with both the tools and knowledge to recognize and respond to the complexities of malaria endemicity. Collaborative initiatives involving governments, NGOs, and international organizations are essential to tackle these pressing health concerns.
Community Awareness and Education on Malaria Risks
Community awareness is vital in addressing malaria risks in regions affected by drug resistance, such as southeastern Sudan. Educating the population about the symptoms, transmission, and treatment of malaria can facilitate earlier diagnoses and reduce transmission rates. Awareness campaigns can also inform communities about the importance of adherence to treatment regimens, especially given the backdrop of emerging drug-resistant strains of *Plasmodium falciparum*. By understanding their role in malaria prevention, individuals can contribute proactively to local health outcomes.
Moreover, educational initiatives can help demystify the complexities surrounding malaria diagnostics, particularly the limitations posed by HRP2 diagnostic deletions. Empowering communities with knowledge about alternative diagnostic strategies available for detecting *Plasmodium falciparum* is essential for effective malaria management. Community engagement and education should be integral components of malaria control programs, facilitating a shared responsibility between health authorities and local populations in combating this persistent disease.
The Importance of Research in Malaria Drug Resistance
Research plays a critical role in addressing malaria drug resistance, particularly in understanding the genetic factors contributing to the emergence of treatment-resistant *Plasmodium falciparum* strains. Studies focusing on the molecular basis of resistance, such as the mechanisms associated with the Pfkelch13 mutation, provide invaluable insights that can inform clinical practices and public health policies. Continuous research efforts are needed to monitor resistance trends and develop new therapeutic approaches to combat emerging strains effectively.
Moreover, fostering partnerships between researchers and healthcare providers ensures that findings are translated into actionable strategies that can directly benefit affected populations. Funding and support for research on malaria drug resistance are essential in driving innovations that improve treatment options and diagnostic techniques. By prioritizing research as a cornerstone of malaria control, stakeholders can both anticipate future challenges and forge pathways for effective interventions against this disease.
Conclusions about Malaria Resistance in Southeastern Sudan
Concluding this examination of malaria resistance in southeastern Sudan, it is evident that immediate action is required to mitigate the threat posed by *Plasmodium falciparum* and the rising instances of artemisinin resistance. The identification of significant mutations such as Pfkelch13 R622I, alongside issues of HRP2 diagnostic deletions, underscores the complexity of managing malaria in this region. Collaboration among local health authorities, the international community, and researchers is essential to build strategic responses necessary to address these challenges.
In conclusion, ongoing research, enhanced surveillance, and community engagement will be key components of a successful strategy to combat malaria drug resistance in southeastern Sudan. Future endeavors must focus on refining treatment protocols, improving diagnostic accuracy, and ultimately, striving towards the goal of malaria elimination in the region. Only through a comprehensive and collaborative approach can the fight against malaria adapt to the evolving challenges presented by drug-resistant strains.
Frequently Asked Questions
What is artemisinin resistance in *Plasmodium falciparum* and its implications for malaria treatment?
Artemisinin resistance in *Plasmodium falciparum* refers to the reduced effectiveness of artemisinin-based treatments, particularly in regions with high transmission rates. This resistance threatens malaria treatment outcomes and complicates control efforts, as evidenced by the high prevalence of Pfkelch13 mutations like R622I found in southeastern Sudan.
How do Pfkelch13 mutations relate to artemisinin resistance in malaria?
Pfkelch13 mutations, such as R622I, are genetic changes in *Plasmodium falciparum* that are strongly associated with artemisinin resistance. These mutations affect the parasite’s response to artemisinin-based combination therapies (ACTs), leading to prolonged parasite clearance times, which complicates malaria treatment.
What role do HRP2 diagnostic deletions play in malaria detection and treatment efficacy?
HRP2 diagnostic deletions in *Plasmodium falciparum* compromise the accuracy of rapid diagnostic tests (RDTs), which rely on HRP2 for parasite detection. This can result in undetected infections and ineffective treatment outcomes in artemisinin-resistant malaria cases, particularly in areas like southeastern Sudan.
Why is surveillance of artemisinin resistance crucial in regions like southeastern Sudan?
Regular surveillance for artemisinin resistance in regions such as southeastern Sudan is critical to identify and manage *Plasmodium falciparum* strains with reduced susceptibility to artemisinin. This ongoing monitoring helps ensure effective malaria treatment strategies and ultimately protects public health in high-transmission areas.
What are the consequences of artemisinin resistance on malaria control efforts in sub-Saharan Africa?
Artemisinin resistance poses considerable challenges to malaria control in sub-Saharan Africa. It undermines the effectiveness of first-line treatments, increases the risk of treatment failure, and may lead to a surge in malaria morbidity and mortality, stressing the importance of swift responses to emerging resistance patterns.
How are researchers studying artemisinin resistance in *Plasmodium falciparum*?
Researchers study artemisinin resistance by analyzing genetic mutations like Pfkelch13 in a wide array of *Plasmodium falciparum* samples from areas with reported resistance. Techniques such as molecular analysis of blood samples are employed to monitor the prevalence of resistant strains and to inform public health policies.
What impact do artemisinin-resistant *Plasmodium falciparum* strains have on malaria treatment regimens?
Artemisinin-resistant *Plasmodium falciparum* strains necessitate changes in malaria treatment regimens, often requiring the use of alternative drugs or combination therapies to overcome reduced efficacy. This adaptation is crucial to effectively manage infections and prevent further transmission in affected regions.
| Key Point | Details |
|---|---|
| Study Overview | Hospital-based cross-sectional study in southeastern Sudan conducted in 2017. |
| Sample Size | 257 *P. falciparum* samples were analyzed. |
| Resistance Findings | 22% of samples had the pfkelch13 R622I mutation; 10.7% showed hrp2/3 gene deletions. |
| Geographic Focus | Focus on the Al Jazirah and Al Qadarif states in southeastern Sudan. |
| Implications | Emergence of artemisinin resistance threatens malaria treatment and control efforts. |
| Surveillance Need | Highlights the need for enhanced surveillance of drug-resistant parasites in the Horn of Africa. |
Summary
Artemisinin resistance has emerged as a significant challenge in malaria control, particularly in regions like southeastern Sudan. The study conducted shows a worrying prevalence of the Pfkelch13 R622I mutant within *Plasmodium falciparum*, indicating a need for urgent surveillance and monitoring. The presence of genetic variations linked to drug resistance not only complicates treatment protocols but also jeopardizes ongoing public health efforts to combat malaria. Therefore, addressing artemisinin resistance through improved regional strategies and diagnostics is essential to ensure effective malaria management moving forward.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.