Antifungal medicines play a pivotal role in the fight against fungal infections, a growing health concern that affects millions globally. These infections range from mild skin irritations to severe, life-threatening conditions, making effective antifungal treatments essential for patient care. As drug resistance becomes an increasingly alarming issue, understanding the spectrum of antifungal medications available is crucial for healthcare professionals and patients alike. From addressing common ailments like oral thrush to combating more serious skin infections, the development of these medicines continues to evolve. Staying informed about the latest advancements in antifungal therapies is vital for ensuring effective management of fungal infections and improving health outcomes.
Antifungal therapies, often referred to as antifungal agents, are critical in treating a variety of mycotic conditions that can lead to severe health complications. These agents target fungal pathogens responsible for infections that affect both human and animal health, necessitating a broad spectrum of treatment options. The rise of fungal diseases highlights the importance of these pharmacological interventions, especially as we face challenges such as drug resistance and the need for innovative treatment strategies. From topical creams to systemic medications, understanding the diverse categories of antifungal solutions is essential for effective treatment. As we explore the landscape of antifungal options, we must remain vigilant about emerging threats and advancements in the field.
Understanding Fungal Infections: Causes and Symptoms
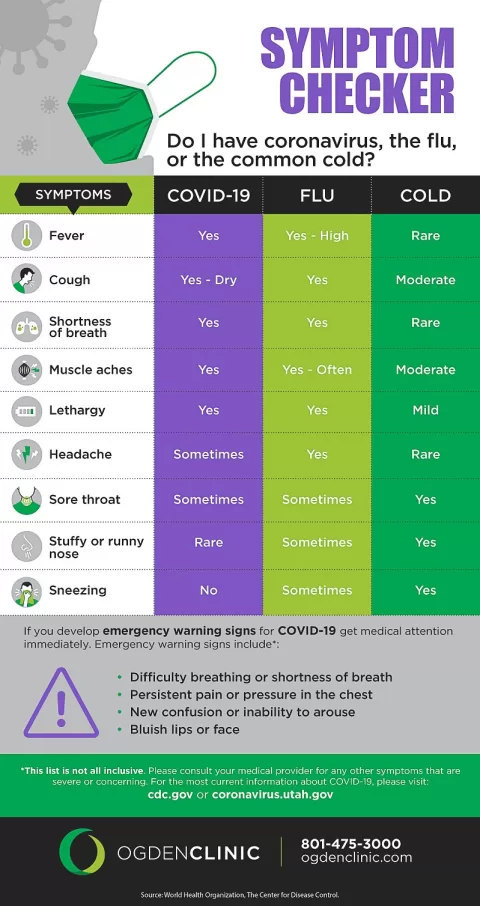
Fungal infections can range from mild to severe and can affect various parts of the body, including the skin, mouth, and internal organs. Common types of fungal infections include athlete’s foot, ringworm, and oral thrush. The symptoms often vary based on the type and severity of the infection, with signs such as itching, redness, and discomfort being prevalent. In some cases, fungal infections can lead to more serious health complications, especially in individuals with weakened immune systems.
Identifying the specific type of fungal infection is crucial for effective treatment. For instance, oral thrush presents with white patches in the mouth and can be especially problematic for those undergoing immunosuppressive treatments. Understanding these symptoms and their implications can aid in early detection and prompt treatment, reducing the risk of complications associated with untreated fungal infections.
The Role of Antifungal Treatments in Managing Infections
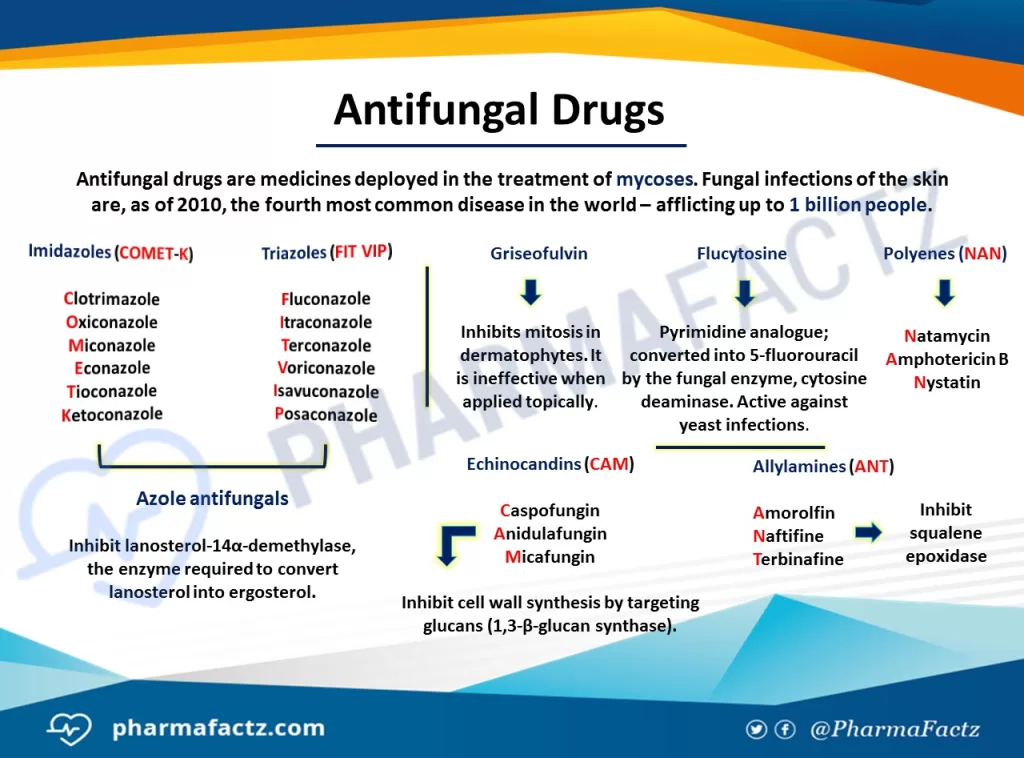
Antifungal treatments play a pivotal role in managing various fungal infections effectively. These treatments are classified into several categories, such as topical, oral, and intravenous antifungals, each tailored to combat specific types of fungi. For instance, topical treatments like clotrimazole are effective for superficial skin infections, while oral antifungals such as fluconazole are prescribed for more invasive infections that can affect internal organs.
The choice of antifungal treatment is often guided by the infection’s severity, the patient’s health status, and potential drug resistance. As the landscape of fungal infections evolves, healthcare providers must stay informed about the latest antifungal treatments to ensure optimal patient outcomes. By employing a tailored approach to antifungal therapy, clinicians can significantly improve the management of fungal infections in their patients.
Exploring Drug Resistance in Antifungal Therapies
Drug resistance has emerged as a significant concern within the realm of antifungal treatments. As fungi evolve, they can develop mechanisms to evade the effects of commonly used antifungal medications, rendering standard treatments less effective. This phenomenon is particularly alarming given the rising incidence of invasive fungal infections, which can be life-threatening, especially for immunocompromised individuals.
To combat this growing challenge, researchers are focusing on developing next-generation antifungal agents that can overcome the resistance mechanisms employed by fungi. This may involve innovative approaches, such as utilizing combination therapies or creating new drug classes that target different aspects of fungal biology. Addressing drug resistance in antifungal therapies is crucial for ensuring effective treatment options remain available for patients suffering from fungal infections.
Innovative Treatments for Oral Thrush and Skin Infections
Oral thrush, a common fungal infection caused by an overgrowth of Candida species, requires specific antifungal treatments to restore balance. Nystatin and fluconazole are frequently prescribed to manage this condition effectively. Topical treatments are often the first line of defense, especially in mild cases, while systemic treatments may be necessary for more severe or recurrent infections.
Skin infections caused by fungi, such as athlete’s foot and ringworm, also benefit from targeted antifungal therapies. Topical antifungals like terbinafine and miconazole are commonly used to treat these conditions. It is essential to follow healthcare professional recommendations for treatment duration and application methods to ensure complete resolution of the infection and prevent recurrence.
Advancements in Antifungal Research and Development
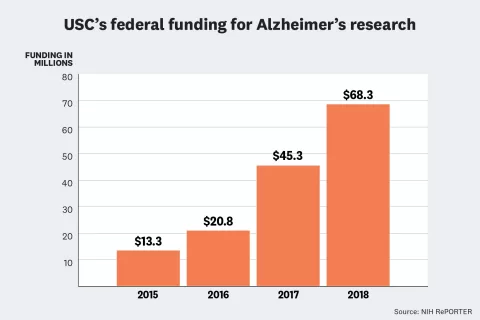
The field of antifungal research is experiencing significant advancements, driven by the pressing need to address both the rising incidence of fungal infections and the challenges posed by drug resistance. Researchers are exploring new molecules and treatment modalities that can effectively target fungi while minimizing side effects. This includes the development of antifungal medications that can penetrate biofilms, which are protective layers formed by fungi that can lead to treatment failure.
Furthermore, ongoing clinical trials are crucial in assessing the safety and efficacy of novel antifungal therapies. These advancements could lead to improved treatment options for patients suffering from challenging fungal infections, ensuring that healthcare providers have access to a robust arsenal of antifungal medicines to combat these diseases effectively.
Frequently Asked Questions
What are antifungal medicines used for?
Antifungal medicines are primarily used to treat various fungal infections, including skin infections like athlete’s foot, oral thrush, and invasive fungal diseases. They can be administered topically, orally, or intravenously, depending on the severity and type of infection.
How do antifungal treatments work against fungal infections?
Antifungal treatments work by targeting the cell structures of fungi, disrupting their growth and reproduction. Different classes of antifungal medicines, such as azoles and echinocandins, utilize various mechanisms to effectively combat fungal infections.
What is antifungal drug resistance and why is it a concern?
Antifungal drug resistance occurs when fungi adapt to resist the effects of antifungal medications, making infections harder to treat. This is a significant concern in public health as it can lead to treatment failures and increased mortality from fungal infections.
What are the common antifungal treatments for oral thrush?
Common antifungal treatments for oral thrush include topical medications like nystatin and systemic treatments such as fluconazole. These help eliminate the overgrowth of yeast in the mouth, alleviating symptoms and preventing recurrence.
What should I do if I have a persistent skin infection that may be fungal?
If you have a persistent skin infection that may be fungal, it’s crucial to consult a healthcare professional. They can diagnose the condition accurately and recommend appropriate antifungal treatments tailored to effectively address your specific infection.
| Key Point | Details |
|---|---|
| Introduction | Importance of antifungal medicines in addressing fungal infections affecting millions globally. |
| Global Accessibility | Millions lack access to antifungal medicines, leading to over 3,500 deaths daily from fungal infections. |
| Diverse Treatments | Antifungal treatments include topical (e.g., clotrimazole), oral (e.g., fluconazole), and intravenous (e.g., amphotericin B) options. |
| Dermatological Advancements | Fungal acne requires specialized antifungal treatments, differing from traditional acne. |
| Drug Resistance | Fungi are evolving resistance to antifungal drugs, necessitating ongoing research for new treatments. |
| Specialized Medications | Special treatments exist for oral thrush and pet infections, emphasizing the need for effective antifungal therapies. |
Summary
Antifungal medicines are crucial for treating fungal infections that pose serious health risks to individuals globally. With the rise in fungal infections and the concerning issue of drug resistance, the demand for effective antifungal treatments continues to grow. Recent advancements have shed light on the importance of global accessibility to these medications, as many individuals, even in high-income countries, remain unable to access life-saving antifungal treatments. It is essential for healthcare professionals and public health organizations to address these challenges, ensuring that both humans and animals receive the necessary antifungal therapies. As research progresses, staying informed about the latest developments in antifungal medicines will be vital in the fight against fungal infections.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.