Alcohol cancer warning labels have recently taken center stage in a crucial public health discussion, spearheaded by United States Surgeon General Dr. Vivek Murthy. He advocates for updates to these labels to reflect the increasing evidence linking alcohol consumption to significant cancer risks, considering it a vital step toward protecting public health. For the first time in over three decades, Murthy’s proposal emphasizes that current warnings fail to inform consumers about the potential dangers of alcohol-related cancer, which accounts for approximately 100,000 cases annually. This push brings attention to the health risks of alcohol and could reshape consumer behavior by raising awareness of the cancer risk associated with drinking. As alcohol consumption cancer research and public awareness expand, implementing clear warning labels on alcoholic beverages could serve as an effective tool to inform individuals about their choices and the associated health implications.
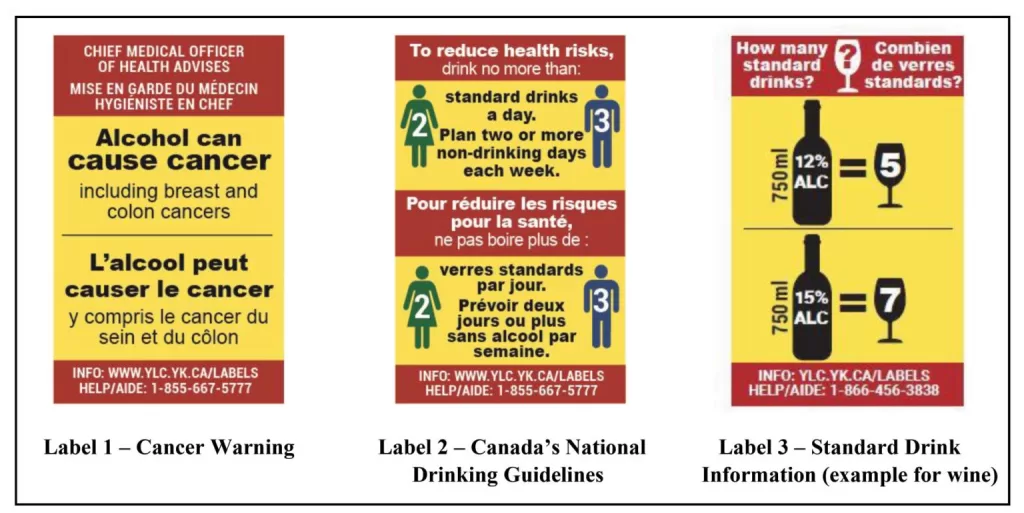
The conversation surrounding alcohol consumption and its health implications has prompted calls for more informative labeling on alcoholic products. Proposed updates to the labels aim to include specific warnings about the connection between drinking and cancer, akin to existing warnings for tobacco products. This initiative reflects a broader effort to enhance consumer knowledge regarding the dangers of alcohol, particularly its links to various forms of cancer. By portraying alcohol as a potentially harmful substance, these changes could stimulate discussion about responsible drinking and public health. Advocates believe that similar to successful tobacco warning campaigns, these alcohol labels could play a pivotal role in reducing consumption and promoting safer drinking habits.
Understanding Alcohol and Its Cancer Risks
The relationship between alcohol consumption and cancer has been increasingly examined in recent years. Studies indicate that drinking alcohol significantly elevates the risk of developing several types of cancer. Notably, the U.S. Surgeon General highlights that alcohol is linked to approximately 100,000 cancer cases annually in the United States. Certain cancers, including breast, liver, and colon cancer, are particularly affected by alcohol intake due to the mechanisms such as DNA damage and hormonal disruption caused by acetaldehyde, a byproduct of alcohol metabolism.
Furthermore, the emerging research supports the Surgeon General’s call for more comprehensive warning labels on alcoholic beverages to increase public awareness. While many people recognize the dangers of tobacco, only about 45% acknowledge that alcohol can increase cancer risk. This stark contrast underscores a critical need for education and transparency regarding health risks associated with alcohol consumption.
The Case for Updated Alcohol Warning Labels
The U.S. Surgeon General’s push for new alcohol warning labels marks a significant shift in public health policy regarding alcohol consumption. The proposal advocates for clear warning labels that explicitly mention cancer risks, aligning with campaigns for transparency seen in tobacco legislation. Since the existing warning labels were implemented in 1988, public knowledge of the health risks associated with alcohol has evolved significantly. The Surgeon General argues that these labels are outdated and do not reflect current understanding, thus jeopardizing public health.
Adding cancer warning labels on alcohol could serve a dual purpose: educating consumers about the risks while potentially curbing alcohol consumption. Historical evidence from tobacco warning campaigns suggests that explicit health warnings can reduce usage rates. Research demonstrates that detailed information can lead to behavioral changes, empowering individuals to make informed choices about their health.
Health Implications of Alcohol Consumption
Alcohol consumption has been scientifically linked to increased cancer risk, affecting an alarming number of individuals each year. Medical experts stress that there is no safe level of alcohol when considering cancer; even minimal consumption can pose health risks. This clarion call for awareness is backed by the Surgeon General’s advisory outlining that consuming just two drinks daily can increase one’s lifetime risk of cancer—a staggering truth that warrants greater public scrutiny.
In addition to cancer, alcohol can also have detrimental effects on cardiovascular health. Experts suggest that alcohol can raise blood pressure and lead to heart diseases, further complicating the narrative around supposed “moderate” alcohol consumption benefits. Currently, studies challenge the myths surrounding moderate drinking, asserting that any perceived benefits are heavily outweighed by the risks, particularly concerning cancer and heart health.
Global Perspectives on Alcohol and Cancer Statistics
Globally, the evidence surrounding alcohol consumption and cancer reflects similar trends noted by U.S. health officials. In Europe, for instance, alcohol use was responsible for 180,000 cancer cases in 2018 alone. Alarmingly, the connection is ever-present, with various studies correlating high alcohol use with significant health risks across diverse populations. Understanding these statistics is crucial in framing health policies and implementing effective warning labels on alcoholic beverages.
Further emphasizing the global burden, in countries like China, alcohol accounts for over 93,000 cancer cases annually. This illustrates that the problem transcends borders, affecting millions around the world. As public health experts advocate for broader awareness and policy changes, the global health community recognizes the necessity of engaging in conversations about alcohol-related health risks to foster meaningful change.
Alcohol Consumption and Its Impact on Young Adults
Recent trends indicate a decline in alcohol consumption among young adults, prompting public health officials to consider the implications of societal shifts. Data shows that approximately 50% of individuals aged 18 to 25 reported drinking in the past month, a steep drop from previous years. This shift presents a critical period for educating this demographic about the risks associated with alcohol, particularly the cancer risks highlighted in the surgeon general’s advisory.
Understanding these trends also highlights the importance of engaging with young people through responsible advertising and informative labeling. Campaigns promoting non-alcoholic alternatives, bolstered by the growing popularity of movements such as ‘Dry January’, communicate that choosing to abstain from alcohol can be both socially acceptable and beneficial for long-term health. By harnessing this generational change, health professionals can better address alcohol-related health concerns.
Potential Solutions to Alcohol-Related Health Risks
Tackling the health risks associated with alcohol consumption goes beyond merely relating them to cancer risks. Public health experts suggest integrating various strategies, such as increasing federal excise taxes on alcoholic beverages. Such measures could not only reduce consumption levels but also communicate a societal message that alcohol is not a benign product.
Moreover, universal labeling that includes information about health risks, similar to the requirements for food and tobacco products, can foster informed choices among consumers. These strategies, combined with enhanced awareness campaigns about the health impacts of alcohol, can create a more comprehensive approach to reducing alcohol consumption and its associated health risks.
The Efficacy of Warning Labels in Public Health
The role of warning labels in public health has been an area of extensive research and debate. Advocates for alcohol warning labels emphasize their potential to inform consumers about the health risks, similar to the established effectiveness seen in cigarette warning campaigns. While skepticism exists regarding the immediate impact of text-based warnings, broader public awareness campaigns can amplify their effectiveness.
Additionally, health professionals argue that awareness about alcohol’s dangers shouldn’t solely rest on personal responsibility but should be reinforced through clear, accessible information. Empowering consumers with knowledge about the risks associated with alcohol consumption equips them to make informed choices regarding their health, and encouraging evidence-based practices remains essential in making significant strides forward.
The Controversy Surrounding Legislative Changes
Despite the Surgeon General’s advocacy for updated warning labels, the path forward remains fraught with challenges. Historically, legislative measures concerning alcohol have faced fierce opposition from the beverage industry, which has been known to heavily lobby against changes perceived to impact profits. The push for mandates addressing cancer risks encountered similar hurdles demonstrating the industry’s powerful influence in shaping public narratives around alcohol.
With Congress unlikely to act swiftly on warning label updates, it raises concerns about how proactive health policies will adapt within existing legislative frameworks. As health risks become more defined through compelling evidence, it remains crucial for public health advocates to call for necessary changes that can promote healthier behaviors and ultimately save lives.
Public Awareness: A Key to Change
Raising public awareness regarding the health risks of alcohol is vital in instigating behavioral change. While the Surgeon General’s report emphasizes the correlation of alcohol consumption and cancer, it also highlights a gap in public knowledge, with only a fraction of people recognizing alcohol as a significant risk factor. This indicates a pressing need for enhanced educational campaigns targeting various demographics.
Public health strategies must prioritize engaging communities on the health risks of alcohol through schools, healthcare settings, and social media platforms. By fostering open dialogue and providing clear, factual information, stakeholders can empower individuals to understand the risks, confront myths surrounding alcohol consumption, and ultimately contribute to a cultural shift in how society views alcohol.
The Future of Alcohol Regulation and Policy
As the discourse surrounding alcohol consumption evolves, so too must the strategies to regulate it. Enhancing policies related to alcohol, including tax measures and regulatory oversight, is essential to address the accompanying health risks, particularly as they relate to cancer. As experts advocate for stricter regulations, it’s critical to align public health messages with legislative actions to create a unified approach.
Legislators must recognize the growing evidence and public health demands for more comprehensive education and awareness regarding alcohol consumption. By integrating experts’ recommendations, such as those from the WHO and the U.S. Surgeon General, future policies can better reflect scientific findings, engage the public, and promote healthier behaviors that prioritize safety and well-being.
Frequently Asked Questions
What is the importance of cancer warning labels on alcohol beverages?
Cancer warning labels on alcohol beverages are essential as they inform consumers about the health risks associated with alcohol consumption. The U.S. Surgeon General’s proposal highlights the connection between alcohol consumption and various cancers, thereby promoting public awareness and encouraging informed decision-making.
How does the Surgeon General propose to update alcohol warning labels?
The Surgeon General proposes to update alcohol warning labels to include cancer risk information, marking the first major change in 35 years. The updated labels would aim to reflect current scientific understanding of health risks associated with alcohol consumption, including its link to numerous cancers.
What does research say about alcohol consumption and cancer risk?
Research indicates that alcohol consumption significantly increases cancer risk, with approximately 100,000 cancer cases and 20,000 cancer deaths in the U.S. attributed to alcohol annually. Studies show that even moderate drinking can raise the risk of developing various cancers, including breast and liver cancer.
Are existing alcohol warning labels effective in conveying health risks?
Existing alcohol warning labels are considered outdated and insufficient, focusing only on pregnancy risks and impaired driving. The lack of information about cancer risks is a significant gap that could mislead consumers, underlining the need for updated warning labels that reflect current health knowledge.
What types of cancer are linked to alcohol consumption?
Alcohol consumption has been linked to at least seven types of cancer, including breast, colon, liver, mouth, throat, esophageal, and laryngeal cancers. These risks are driven by mechanisms such as DNA damage and hormonal disruption.
How much alcohol increases the risk of cancer?
There is no safe level of alcohol consumption regarding cancer risk. Even consuming two drinks per day can increase the lifetime risk of developing cancer, emphasizing the need for public awareness and health warning labels on alcoholic beverages.
What role do alcohol cancer warning labels play in public health?
Alcohol cancer warning labels play a critical role in public health by raising awareness, supporting broader alcohol policies, and potentially influencing consumer behavior. Similar to tobacco warnings, they can help educate the public about the serious health risks associated with drinking.
Could cancer warning labels lead to decreased alcohol consumption?
While it is uncertain how effective text warnings will be in reducing alcohol consumption, studies on cigarette warning labels suggest that clear health warnings can lead to lower smoking rates, indicating a potential for similar outcomes with alcohol warning labels.
Why does the alcohol industry resist stronger warning labels?
The alcohol industry often resists stronger warning labels due to concerns about potential negative impacts on sales and business. Industry lobbyists argue that such warnings may be ineffective or could adversely affect consumer perceptions.
What are alternative measures to reduce alcohol consumption beyond warning labels?
Experts recommend additional measures, such as increasing taxes on alcohol, limiting marketing, and reducing availability, to effectively curb alcohol consumption. These strategies, combined with warning labels, could create a more comprehensive approach to tackling alcohol-related health risks.
| Key Point | Details |
|---|---|
| Surgeon General’s Proposal | Dr. Vivek Murthy proposes new cancer warning labels on alcohol to reflect updated health evidence. |
| Current Warning Labels | Existing labels focus on pregnancy and driving, not on cancer risks, making them outdated. |
| Cancer Risk Statistics | Alcohol-related consumption accounts for approx. 100,000 cancer cases and 20,000 deaths per year in the US. |
| Effective Public Health Measure? | Murthy believes that updated labels could promote awareness and reduce consumption, similar to cigarette warnings. |
| Global Perspectives | Alcohol consumption connects to significant cancer cases worldwide, with varying impacts across regions. |
| Alcohol’s Role in Cancer | Alcohol increases the risk of several cancers through mechanisms like DNA damage and hormonal disruption. |
| Challenges to Implementation | Industry opposition may delay or prevent Congressional changes to alcohol labeling. |
Summary
Alcohol cancer warning labels are crucial as they aim to inform consumers about the serious risks associated with alcohol consumption, particularly its links to various cancers. As proposed by the US Surgeon General, these labels would mark a significant update since the last change in 1988, addressing a pressing public health issue and enhancing consumer awareness. Given the rising evidence connecting alcohol to cancer, it is essential that these labels not only educate the public but also potentially curb harmful drinking habits.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.