AI in Medical Diagnostics is revolutionizing the healthcare landscape by significantly enhancing the speed and accuracy of disease detection. As artificial intelligence healthcare technologies advance, tools like machine learning medicine are becoming invaluable assets in clinical settings, allowing for more precise radiology, pathology, and biosignal analysis. These AI diagnostics tools process vast amounts of medical data rapidly, aiding doctors in making informed decisions about patient care. The integration of ethical AI in medicine is also a key consideration, ensuring that these technologies operate within frameworks that respect patient rights and data privacy. By comparing AI-driven diagnostics with traditional methods, we can better understand how technology can augment human expertise and improve clinical outcomes.
The integration of advanced computational techniques in hospital settings is reshaping the landscape of disease diagnosis and treatment planning. When exploring alternative terms, we can refer to AI in Medical Diagnostics as intelligent systems for healthcare diagnostics or automated analysis in medical settings. These sophisticated technologies leverage big data analytics and predictive modeling to support healthcare professionals in identifying conditions earlier and with greater precision. Furthermore, these innovations pose both opportunities and challenges, particularly concerning data security and algorithmic bias. As the medical field embraces these technological advancements, it must also navigate the ethical landscape to ensure a patient-centered approach in all diagnostic processes.
The Rise of AI in Medical Diagnostics
Artificial Intelligence is increasingly regarded as a cornerstone in the evolution of medical diagnostics. Leveraging advanced algorithms, machine learning models can analyze extensive datasets derived from various sources—ranging from Electronic Health Records (EHRs) to imaging data such as MRIs and CT scans. This ability not only streamlines the diagnostic process but also allows AI systems to detect patterns and anomalies that might elude even the most experienced physicians. As a result, healthcare providers can offer prompt and accurate diagnoses, greatly enhancing overall patient care outcomes.
Moreover, AI’s role extends beyond simple diagnosis into predictive analytics, where AI-powered models anticipate potential health threats before they manifest visibly. This proactive approach is crucial, especially in managing infectious diseases and chronic illnesses, where early intervention can be life-saving. As AI continues to advance, the integration of these technologies into daily medical practice shows great promise for reducing the burden on healthcare professionals, allowing them to focus on delivering personalized patient care rather than getting bogged down in administrative tasks.
AI in Medical Diagnostics: Tools and Technologies
AI diagnostics tools are at the forefront of transforming healthcare, with technologies such as natural language processing and deep learning driving innovation in this space. These tools enable the examination and interpretation of vast amounts of medical data with remarkable speed and accuracy. For instance, AI algorithms can efficiently identify cancerous lesions in imaging studies, often outperforming human radiologists in both precision and speed. This not only enhances diagnostic outcomes but also allows for a quicker turnaround time in patient management, facilitating timely treatment interventions.
The implications for machine learning in medicine are profound, providing healthcare professionals with enhanced capabilities for diagnosing diseases with a high degree of confidence. As AI technologies become more sophisticated, they are also being integrated into clinical decision support systems (CDSS), offering clinicians data-driven recommendations tailored to individual patient profiles. However, the implementation of these tools must also consider ethical considerations to ensure that patient data is used responsibly, and that the algorithms do not perpetuate existing biases in healthcare.
AI Doctor Comparison: Strengths and Limitations
When comparing AI diagnostics to human doctors, it is essential to examine both the strengths and limitations of these technologies. On one hand, AI demonstrates formidable accuracy, punctuated by its ability to process vast datasets for more reliable diagnosis. For instance, studies reveal that AI systems can reach diagnostic rates comparable to expert physicians in areas like dermatology and radiology, making them invaluable in resource-constrained environments where human expertise might be scarce.
Conversely, human doctors bring invaluable attributes such as empathy, intuition, and contextual understanding, especially in complex or sensitive cases. While AI can analyze data and suggest diagnoses, it lacks the human ability to understand nuanced patient histories and emotional cues. Therefore, a collaborative approach—where AI acts as an augmentation to human capabilities, rather than a replacement—appears to be the most beneficial path forward in the evolution of medical diagnostics.
Case Studies: Successful Applications of AI in Diagnostics
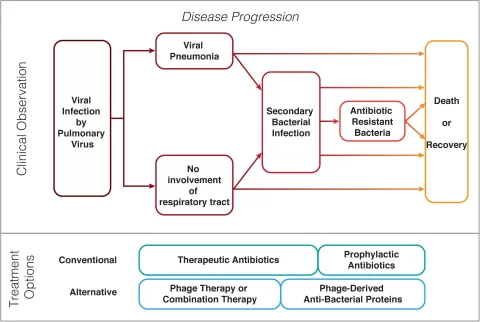
Numerous case studies underscore the successful application of AI in medical diagnostics, illustrating its transformative potential. For instance, machine learning techniques, specifically extreme gradient boosting (XGBoost), have been effectively utilized to predict antimicrobial resistance in various pathogens. This capacity to anticipate drug resistance patterns supports healthcare providers in making informed decisions regarding antibiotic therapies, which is crucial in managing infectious diseases.
Another noteworthy example includes the deployment of deep learning models for rapid blood culture diagnostics in intensive care settings. Here, AI significantly reduces the time required to diagnose infections, allowing clinicians to initiate appropriate treatment strategies more swiftly. These case studies highlight how AI innovations not only enhance diagnostic accuracy but also the overall efficiency of healthcare delivery, establishing a robust framework for integrating AI technologies into clinical practice.
Ethics and AI in Medical Decision-Making
While the integration of AI into medical diagnostics holds tremendous promise, ethical considerations cannot be overlooked. Issues such as data privacy, informed consent, and algorithmic bias must be rigorously addressed to ensure fair and equitable healthcare outcomes. The reliance on vast volumes of sensitive health data raises significant privacy concerns, compelling stakeholders to establish clear data governance frameworks that safeguard patient information while promoting transparency in AI operations.
Furthermore, the risk of algorithmic bias can exacerbate healthcare disparities, especially when AI models are trained on datasets that do not adequately represent all demographics. To mitigate these ethical risks, regulatory measures such as the General Data Protection Regulation (GDPR) and the EU AI Act have been adopted, imposing strict requirements on AI technologies in healthcare. Ultimately, navigating these ethical challenges will be vital in ensuring that AI complements the human touch in medicine, fostering a patient-centric approach that benefits all individuals.
Future Directions for AI in Medical Diagnostics
The future of AI in medical diagnostics looks promising, particularly with the advent of emerging technologies such as Quantum AI and General AI. Quantum computing, with its powerful processing capabilities, has the potential to revolutionize how medical data is analyzed, enabling unprecedented speeds and efficiencies in diagnostics. This advancement could lead to real-time data analysis and improved predictive models, thereby enhancing patient outcomes significantly.
Moreover, ongoing research into General AI aims to develop systems that can replicate the cognitive abilities of human physicians in diagnostic processes. While these technologies are still in their infancy, they hold the promise of creating highly adaptive and intelligent systems capable of making complex medical decisions. As these advancements unfold, it is critical for regulatory frameworks to evolve in tandem, ensuring that ethical guidelines, accountability, and data protection are maintained, thereby fostering public trust in AI-driven healthcare solutions.
Personalized Medicine: The Role of AI
Personalized medicine is an emerging paradigm in healthcare that tailors treatment strategies to individual patient characteristics, and AI is playing a crucial role in this transformation. By analyzing genetic, environmental, and lifestyle factors, AI algorithms can support healthcare providers in crafting customized treatment plans that align with the unique health profiles of patients. This capability is particularly valuable in fields such as oncology, where tumor genomics can inform targeted therapies that enhance efficacy while minimizing adverse effects.
AI-driven predictive analytics can also assist clinicians in identifying patients at high risk for certain conditions, enabling preventive measures to be implemented before any symptoms arise. This proactive approach not only improves health outcomes but also reduces overall healthcare costs by mitigating the development of severe diseases. As the application of AI in personalized medicine expands, it will be critical to maintain an ethical focus on data use, ensuring that advancements benefit all patients equitably.
AI’s Impact on Healthcare Accessibility
One of the remarkable advantages of AI in medical diagnostics is its potential to enhance healthcare accessibility, particularly in underserved areas. AI-powered diagnostic tools can bridge the gap where specialist availability is limited, allowing primary care providers to utilize these technologies for more accurate assessments. This democratization of healthcare means that patients in remote locations can receive quality diagnostic support without the need for extensive travel or resources.
Furthermore, AI can help reduce the workload on healthcare systems by automating routine diagnostic tasks. This not only allows clinicians to focus on more complex cases but also increases the capacity to treat a larger number of patients effectively. The ultimate aim is to ensure that quality healthcare is accessible to everyone, regardless of geographical or socioeconomic barriers, thus promoting health equity across diverse populations.
The Collaborative Future of AI and Human Practitioners
Looking ahead, the future of medical diagnostics will likely center around a collaborative model between AI technologies and healthcare practitioners. This synergy will leverage the strengths of both parties: the efficiency and data-handling capabilities of AI will complement the critical thinking, empathy, and ethical decision-making that human doctors provide. Such collaboration could enhance decision-making processes, ultimately leading to superior patient outcomes.
To foster this collaboration, training programs that educate healthcare professionals on the capabilities and limitations of AI tools will be essential. Empowering doctors with knowledge on how best to utilize AI in their practice will ensure that these technologies are seen as allies rather than replacements. In this way, the evolution of AI in medical diagnostics can enhance the quality of care while preserving the essential human elements of medicine.
Frequently Asked Questions
What are the capabilities of AI in medical diagnostics?
AI in medical diagnostics enhances accuracy, efficiency, and speed in disease detection. AI-powered tools process vast amounts of medical data, including imaging scans and biosignals, aiding in early detection and treatment planning. They utilize advanced algorithms to analyze Electronic Health Records (EHRs) and provide real-time clinical decision support.
How do AI diagnostics tools compare to human doctors?
AI diagnostics tools offer advantages in speed and accuracy, often matching or exceeding human doctors in symptom analysis. However, they lack the contextual understanding and adaptability of human physicians, which remain essential for managing complex and atypical cases.
What ethical considerations surround AI in medical diagnostics?
Ethical considerations include data privacy, algorithmic bias, and transparency. AI systems must be developed to ensure fairness and accountability, particularly addressing disparities in healthcare outcomes for marginalized populations. Regulations like the GDPR and the EU AI Act provide frameworks for ethical AI deployment.
Can machine learning medicine improve diagnostic outcomes?
Yes, machine learning medicine significantly improves diagnostic outcomes by analyzing large datasets and recognizing patterns in complex medical data. AI models have shown high accuracy in predicting conditions such as antimicrobial resistance and classifying tumors in oncological imaging.
What role does explainable AI (XAI) play in medical diagnostics?
Explainable AI (XAI) is crucial for making AI-driven diagnoses transparent and interpretable. It helps medical professionals understand and validate AI predictions, thereby fostering trust in AI diagnostics tools and enhancing patient care.
What are the limitations of AI in medical diagnostics?
AI limitations include dependency on the quality and quantity of data, potential algorithmic bias, and challenges with interoperability among different systems. Additionally, ethical concerns regarding data privacy and the need for human oversight persist.
How has AI contributed to diagnostics during the COVID-19 pandemic?
During the COVID-19 pandemic, AI played a significant role in early diagnosis, vaccine development, and drug repurposing. AI systems quickly analyzed data and assisted healthcare professionals in making informed decisions, enhancing overall public health response.
What future advancements can we expect in AI medical diagnostics?
Future advancements in AI medical diagnostics include the integration of Quantum AI, which may improve data processing speed and predictive accuracy, and General AI, which aims to replicate human-like reasoning in diagnostics. These developments will require careful ethical and regulatory oversight.
How can AI tools ensure patient safety in medical diagnostics?
AI tools can ensure patient safety by being developed under strict regulatory frameworks, such as the EU AI Act, that mandate reliability, accountability, and ethical standards. Continuous monitoring and validation of AI tools in real-world settings are also essential to maintain high safety and efficacy.
What impact does AI have on the doctor-patient relationship?
AI impacts the doctor-patient relationship by streamlining diagnostics and decision-making processes, allowing doctors to focus more on patient care. However, it’s vital that AI complements human interaction rather than replace it, preserving trust and empathy in healthcare.
| Aspect | AI Advantages | AI Limitations | Comparison to Human Doctors |
|---|---|---|---|
| Accuracy | High precision in diagnostics leveraging large datasets. | Data bias may lead to inaccuracies; human intuition is not considered. | AI can deliver accurate diagnoses but lacks the contextual understanding of human doctors. |
| Speed | Instant responses leading to reduced wait times for diagnoses. | Requires large datasets for training which may not be readily available. | AI tools provide rapid assessments but human exams are necessary for complex evaluations. |
| Diagnostic Outcomes | Consistent and scalable, even for high-volume case scenarios. | Limited in handling unique or rare conditions due to lack of adaptability. | Doctors provide personalized care and can make adaptable decisions. |
Summary
AI in Medical Diagnostics is transforming the healthcare landscape by enhancing the accuracy, efficiency, and speed of disease detection and analysis. The integration of AI-driven tools into medical practice has proved beneficial, particularly in areas such as imaging interpretation and clinical decision-making. While AI systems excel in processing vast amounts of data and can match diagnostic accuracies comparable to human doctors, they still face challenges such as data bias and ethical concerns. Human doctors’ contextual understanding and adaptability remain critical, especially in complex scenarios. The future of AI in medical diagnostics looks promising, with the potential for developments such as Quantum AI and General AI to further refine its capabilities. However, a balanced approach that considers human oversight and regulatory standards will be essential to maximize the effectiveness of AI while ensuring ethical healthcare practices.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.