COVID-19 mortality remains a critical concern as studies reveal that, despite widespread availability of vaccines, the virus still poses a greater short-term risk of death compared to seasonal flu. Recent research indicates that hospitalized COVID patients face significantly higher mortality rates than those suffering from influenza. In fact, a study highlighted that individuals diagnosed with COVID-19 have a 76% higher chance of dying within 30 days compared to their counterparts with flu, showcasing the stark contrast in COVID death rates. Furthermore, the effectiveness of the COVID-19 vaccine does not seem to bridge the gap entirely, particularly among vulnerable populations such as those aged 18 to 64 years. This data emphasizes the importance of understanding COVID-19 mortality within the context of overall health risks, including influenza risk comparison and the effectiveness of vaccination strategies for both diseases.
The fatalities associated with the COVID-19 pandemic continue to be alarming, especially when juxtaposed with data on influenza-related deaths. While both illnesses can have severe consequences, the statistics suggest that coronavirus presents a more lethal threat in the healthcare environment, particularly for patients requiring hospitalization. Factors such as COVID-19 vaccine effectiveness and the demographics of hospitalized COVID patients are paramount in assessing ongoing mortality trends. Additionally, understanding how COVID vs flu mortality rates differ can provide critical insights for public health strategies moving forward. Addressing these disparities is vital as we strive to mitigate risks and enhance vaccine uptake across various age groups.
Understanding COVID-19 Mortality Rates Compared to Influenza
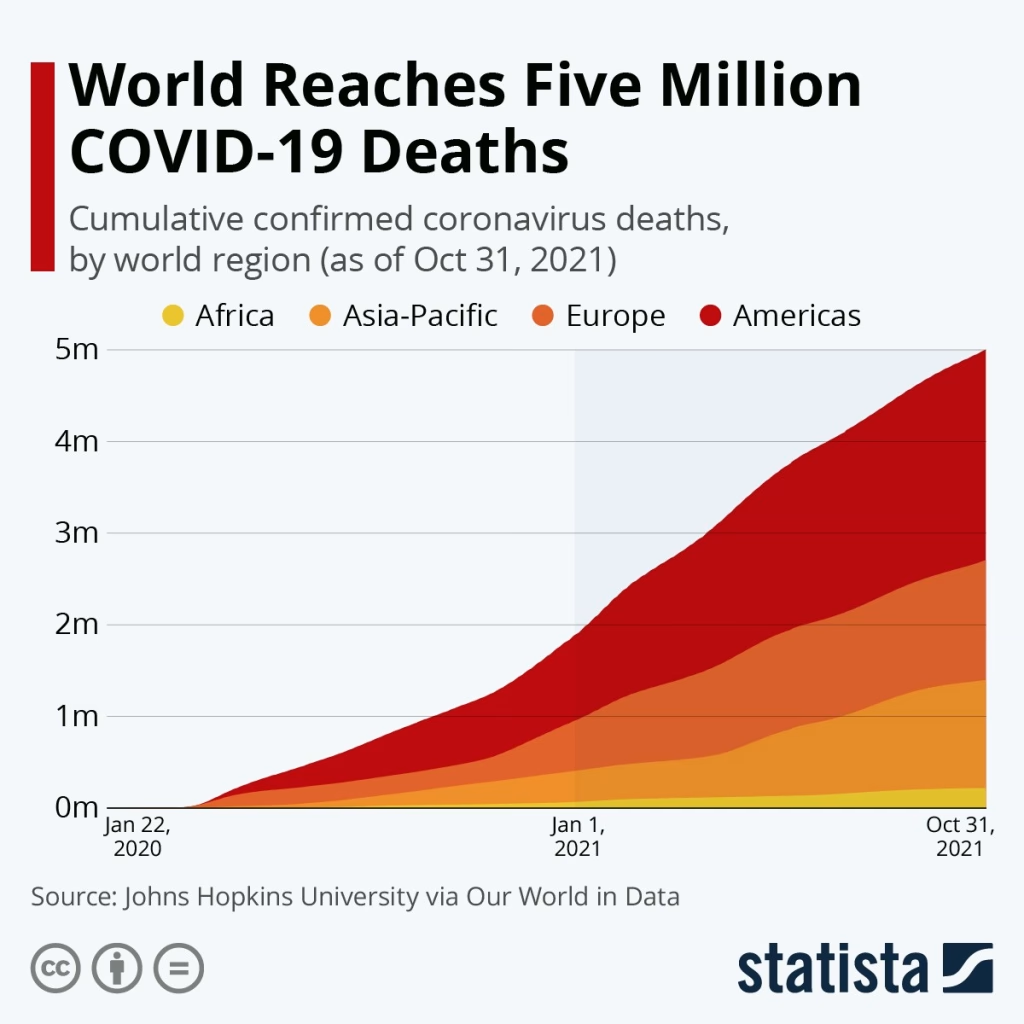
Recent studies show that despite the widespread availability of COVID-19 vaccines, the mortality associated with COVID-19 remains significantly higher than that of influenza. In hospitalized patients, the data indicates a shocking disparity; COVID-19 carries a 76% greater risk of death within 30 days compared to seasonal flu. This statistic reveals crucial insights into the ongoing challenges posed by COVID-19, especially regarding patient demographics and the severity of illnesses such as heart disease or diabetes that can exacerbate outcomes.
To further understand this, researchers analyzed over 15 million health records from South Korean patients diagnosed with either COVID-19 or influenza from July 2022 to December 2023. The findings demonstrated an overall COVID-19 death rate of 0.20%, compared to the mere 0.016% for influenza. The severity of these death rates highlights the necessity for continued vigilance in public health measures and healthcare strategies, particularly in treating high-risk populations.
The Impact of COVID-19 Vaccines on Mortality Rates
Despite the significant advancements in COVID-19 vaccine effectiveness, the data suggests that these vaccines may not entirely mitigate the mortality risk for hospitalized patients. For instance, the study notes that among patients requiring mechanical ventilation, the death risk was 1.88 times greater for those with COVID-19 compared to influenza cases. This finding implies that while vaccination can reduce severe illness and hospitalization risks, it may not sufficiently protect all individuals, particularly those with existing health conditions.
Moreover, vaccination rates reveal a troubling picture. Adults aged 65 and older exhibited an 82.5% uptake for influenza vaccines, yet only 45% received their COVID vaccine. This inequality in vaccine coverage potentially contributes to the higher mortality rates observed among younger COVID-19 patients. Ongoing efforts must focus on improving vaccine uptake across all demographics to enhance community resilience against COVID-19.
Assessing the effectiveness of vaccines is essential in addressing both immediate and long-term public health consequences. Enhanced education and outreach programs targeting vulnerable groups will be necessary to improve these numbers and consequently reduce the death rates associated with COVID-19.
Comparison of COVID-19 and Influenza Mortality
The comparison of COVID-19 and influenza mortality rates provides critical insights into the differentiation between two respiratory illnesses. It is evident that COVID-19 poses a considerably higher mortality risk, which raises essential questions about healthcare strategies and public health responses during ongoing influenza seasons. As COVID-19 continues to dominate health discussions, understanding the comparative mortality data helps prioritize resources and interventions.
Furthermore, the study highlights the importance of understanding different risk factors associated with each virus. For example, young adults with underlying health issues showed increased mortality rates with COVID-19. This detail points to a need for tailored vaccination strategies that consider individual health profiles and can provide more effective outcomes against both COVID-19 and flu.
Hospitalized COVID Patients: An In-Depth Analysis
For hospitalized COVID patients, the implications of mortality rates are critical. The study indicated significant disparities, particularly among specific age groups and those with pre-existing conditions. The increased risk of death among COVID patients receiving mechanical ventilation emphasizes the urgent need for comprehensive care strategies that focus on the most vulnerable populations. Understanding the intricacies of COVID patient care can drive improvements in treatment protocols and outcomes.
In addition, the research indicates an adjusted odds ratio of 2.93 for adults aged 18 to 64, illustrating that younger patients are not immune to severe effects from COVID-19. These patients’ healthcare demands will remain high, necessitating effective healthcare infrastructure and resource allocation to handle surges in hospitalization during outbreaks.
The Role of Targeted Vaccination Strategies
Given the disparities between COVID-19 and influenza mortality rates, targeted vaccination strategies become paramount in mitigating risks. The data suggests that efforts must be intensified to improve vaccine uptake, particularly in younger populations, who display lower coverage rates for COVID-19 vaccines. Customized outreach campaigns aimed at educating younger adults about the importance of vaccination can play a significant role in public health.
Moreover, authorities must also consider creating incentives for vaccination and ensuring easy access to vaccines. Enhancing collaboration between healthcare providers and community organizations could lead to improved vaccination rates in underserved areas, thus contributing to a decrease in the overall mortality rates associated with COVID-19 and ensuring better protection against influenza.
Long-Term Implications of COVID-19 Mortality on Public Health
The ongoing examination of COVID-19 mortality rates carries significant implications for public health policy and preparedness for future pandemics. Documenting the contrasting mortality rates between COVID-19 and influenza not only underscores the urgent need for effective responses during active outbreaks but also informs future vaccine distribution strategies. Building on lessons learned, public health officials can better prepare for fluctuations in virus prevalence.
As new variants emerge and populations evolve, continuous research into the effectiveness of vaccines and treatment strategies will be vital. The potential implications for long-term health care systems, which may face increased demand as the population grapples with the healthcare consequences of COVID-19, are an important focus for future research efforts.
Addressing the Differences in Vaccine Uptake
One of the key findings from the study revolves around the differences in vaccination uptake between COVID-19 and influenza vaccines. With a stark contrast in vaccine coverage rates—82.5% for influenza versus only 45% for COVID-19 among older adults—this discrepancy highlights a significant public health challenge. Addressing vaccine hesitancy and misinformation is critical in increasing uptake, particularly among demographic groups that have lower vaccination rates.
Proactive measures, such as community educational initiatives and outreach to high-risk populations, can help alleviate concerns regarding COVID-19 vaccinations. By creating environments that encourage informed decision-making and increasing accessibility, health authorities stand a better chance of improving vaccination rates and ultimately reducing COVID-19 mortality.
Future Research Directions on COVID Mortality
Future research must continue to explore the underlying factors contributing to COVID-19’s higher mortality rates compared to influenza. Identifying key demographics and examining the effectiveness of current vaccination strategies will provide a clearer picture of how to address these challenges. Understanding the nuances of infected populations—with varying health conditions—can drive tailored healthcare responses.
Additionally, the exploration of long-term effects and complications from COVID-19 will become increasingly important as the world transitions toward a post-pandemic reality. Such research can inform both clinical practices and public health policies aimed at ensuring better preparedness for potential future outbreaks.
The Importance of Continued Vigilance Against COVID-19
As COVID-19 continues to pose health risks, the importance of sustained vigilance cannot be overstated. Health officials must emphasize the need for ongoing monitoring of infection and mortality rates while adapting policies to the evolving landscape of COVID-19. This awareness aids in effectively managing healthcare resources and addressing the needs of populations that remain vulnerable.
In addition, public awareness campaigns concentrating on the significance of remaining vigilant against COVID-19, even with available vaccines, will be crucial. Encouraging continued preventive measures, such as masking and social distancing when necessary, can complement efforts to reduce overall mortality and ensure a healthier society moving forward.
Frequently Asked Questions
What are the COVID-19 mortality rates compared to influenza?
Research indicates that COVID-19 has significantly higher mortality rates compared to influenza. A recent study highlighted that individuals diagnosed with COVID-19 faced a 76% higher risk of death within 30 days compared to those with flu. Specifically, 0.20% of COVID patients died within this period, contrasted with just 0.016% for influenza, representing a 12.5-fold difference in crude mortality rates.
How does COVID-19 vaccine effectiveness influence mortality rates?
Despite the availability of COVID-19 vaccines, the study reveals that COVID-19 still poses a greater short-term mortality risk than seasonal flu. The effectiveness of COVID-19 vaccines appears limited in reducing mortality among certain demographics, particularly younger individuals, emphasizing the importance of increasing vaccine coverage to mitigate COVID-19 mortality rates.
What is the difference in COVID vs flu mortality for hospitalized patients?
Among hospitalized patients, COVID-19 is associated with a significantly higher risk of death. For those requiring mechanical ventilation, the risk of mortality is nearly 1.88 times higher for COVID-19 patients than for influenza cases. These findings underscore the seriousness of COVID-19, particularly in more severe health situations.
How do COVID death rates vary by age group?
COVID-19 mortality rates are particularly high among younger adults aged 18 to 64, with an adjusted odds ratio of 2.93 for mortality compared to influenza. This suggests that even younger adults, who may perceive COVID-19 as less dangerous, are at a greater risk than previously understood when facing severe infections.
What factors contribute to the higher COVID-19 mortality in certain populations?
Factors contributing to higher COVID-19 mortality rates include underlying health conditions such as heart disease, chronic lung disease, or diabetes. For instance, research indicates that COVID-19 patients with these conditions face more than twice the risk of death compared to those with influenza, emphasizing the need for targeted public health strategies.
| Key Points |
|---|
| COVID-19 has a higher mortality rate than influenza for hospitalized patients, despite vaccine availability. |
| COVID diagnosis associated with 76% higher odds of death within 30 days compared to influenza. |
| 0.20% of COVID patients died within 30 days versus 0.016% of influenza patients, marking a 12.5-fold difference in mortality. |
| Higher risk of death linked to those receiving mechanical ventilation (1.88 times higher for COVID). |
| Younger adults (aged 18-64) show 2.93 times higher risk compared to others, particularly among hospitalized patients. |
| Disparity in vaccination uptake: 82.5% for influenza vs. 45% for COVID in adults aged 65 and older. |
Summary
COVID-19 mortality remains a critical concern, evidenced by the latest study revealing that despite the widespread availability of vaccines, COVID-19 is still deadlier than the flu among hospitalized patients. The study highlighted that individuals diagnosed with COVID-19 have a significant increase in mortality risk compared to those with influenza. Furthermore, disparities in vaccination rates, particularly among the older population, may contribute to the continued high mortality associated with COVID-19.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.