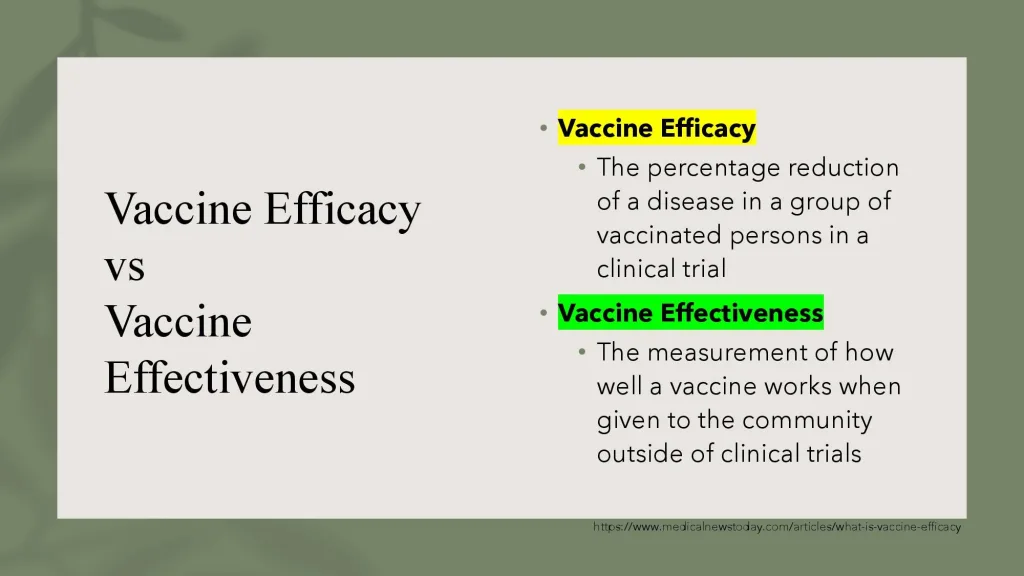
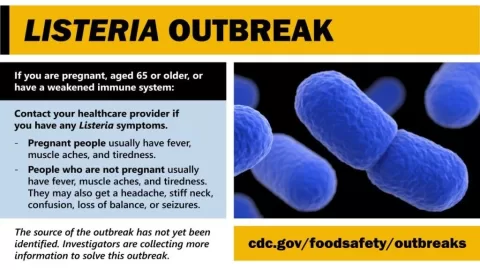
Vaccine Effectiveness and Safety are crucial topics as we navigate the complexities of respiratory viral infections. In light of recent findings on COVID-19 vaccines, RSV immunizations, and influenza vaccines, understanding how these vaccinations perform in real-world scenarios is essential for public health guidance. The comprehensive analysis from our systematic review published in the New England Journal of Medicine sheds light on the vital statistics surrounding these vaccines, providing clarity amidst ongoing discussions about vaccine safety. With a specific focus on how effective these vaccines are at preventing hospitalization, the numbers reflect a commitment to better health outcomes for our communities. It’s evident that maintaining vigilance over vaccine safety and effectiveness remains paramount as we head into the 2025-26 respiratory virus season.
Exploring the landscape of immunizations reveals the significant impact of vaccine performance on public health. The nuances surrounding vaccine safety, particularly for COVID-19, RSV, and seasonal influenza vaccines, demand attention as new data emerges. Recent evaluations highlight the importance of understanding vaccine efficacy in varying populations, especially among those most vulnerable. As we confront challenges in vaccine advisory processes, it becomes increasingly essential to rely on robust evidence to inform individual decisions about vaccination. This dialogue emphasizes the need for ongoing education about the protective benefits offered by vaccinations and their role in safeguarding public health.
Understanding COVID-19 Vaccine Effectiveness in 2025
The effectiveness of COVID-19 vaccines has become more complex as we enter the 2025 respiratory virus season. Recent data indicates that vaccines might show effectiveness rates ranging from 46% to 50% against hospitalization. However, interpreting these statistics requires a nuanced understanding, particularly when considering that many individuals have developed natural immunity due to previous infections. This pre-existing immunity plays a critical role in how well the vaccine provides additional protection. Clinicians and public health officials must navigate this landscape to accurately inform patients about their immunization options and associated risks.
Furthermore, a closer examination of data from recent studies, such as those conducted within the Veterans Affairs health system, suggests that specific vaccine formulations can yield varying success depending on circulating virus strains. For example, the KP.2 vaccine demonstrated a notable effectiveness of 68% against hospitalizations, which is significantly higher than the 32% effectiveness observed during the earlier JN.1 variant’s prevalence. Thus, through continuous monitoring and adaptation of vaccine strategies, healthcare providers can enhance patient outcomes in a rapidly changing viral environment.
RSV Vaccination: Protecting Our Most Vulnerable
Recent findings on respiratory syncytial virus (RSV) immunizations reveal a promising 75% to 80% effectiveness against hospitalization in individuals aged 60 and older. This high level of effectiveness is particularly noteworthy since it reflects a stark contrast against the backdrop of various vaccination approaches. For adults who have previously been exposed to RSV but have never received an RSV vaccine, the introduction of immunizations provides a crucial line of defense against severe disease. Given RSV’s known burden of hospitalizations, having effective vaccination strategies is essential for public health.
Additionally, innovations such as maternal immunization with the RSVpreF vaccine have shown impressive results, achieving a 68% effectiveness rate against infant hospitalizations through the transfer of antibodies. Similarly, the utilization of long-acting monoclonal antibodies like Nirsevimab has emerged as a powerful tool, boasting 80% to 85% effectiveness in preventing severe outcomes. These advances have transformed the landscape of RSV prevention, allowing for targeted interventions that can save lives, especially among high-risk populations such as infants and the elderly.
Flu Vaccines: Yearly Adaptation for Ongoing Protection
Influenza vaccines remain a critical component of public health strategies, demonstrating varying effectiveness rates year-to-year based on how well they match circulating strains. The pooled effectiveness found in our recent review highlights that vaccination can reduce hospitalization rates to 67% in children, while rates vary between 42% and 53% in older adults. This variability underscores the necessity of annual vaccine formulations that can adapt to the changing landscape of influenza strains, thereby optimizing protection for the general population.
Despite fluctuations in efficacy, it’s imperative to recognize the valuable protective capabilities of flu vaccines. Enhanced formulations, particularly for older adults, consistently show superior effectiveness compared to standard doses. This evidence reinforces public health recommendations advocating for its preferential use in vulnerable populations. Continuous surveillance and data analysis are key to understanding and improving flu vaccine strategies, ensuring that all individuals—especially those at higher risk—benefit from effective immunization against seasonal infections.
The Importance of Vaccine Safety Surveillance
Safety is a paramount concern when discussing vaccines. Our extensive analysis across numerous studies reassuringly indicates that the risk of myocarditis following COVID-19 mRNA vaccination remains low, particularly among most demographics. Reportedly, cases are predominantly found in adolescent males, where incidence rates are significantly lower than those observed in 2021. Moreover, findings from large observational studies have demonstrated that the risk of myocarditis following COVID-19 infection itself surpasses the post-vaccine risk, highlighting a favorable risk-benefit balance for vaccine recipients.
In terms of RSV vaccines, safety monitoring has also been rigorous. Although some studies raised concerns about Guillain-Barre syndrome (GBS) following the administration of RSVpreF, the overall risk remains very low, ensuring that vaccine benefits—illustrated through substantial reductions in hospitalization—outweigh potential adverse effects. The Food and Drug Administration’s ongoing assessments and any updates on safety warnings are vital for maintaining public trust in vaccination efforts, paving the way for broader community uptake and improved public health outcomes.
Navigating Vaccine Choices in an Evolving Landscape
Today, making informed decisions about immunizations requires a thorough understanding of how different vaccines interact with individual health statuses and existing immunity levels. A healthy 30-year-old with a robust background immunity might approach COVID-19 vaccination differently than a 75-year-old with heightened risks from RSV. Knowledge of vaccine effectiveness against specific diseases and variants will empower individuals to weigh their options and make choices aligned with their health needs.
This evolving landscape necessitates that clinicians provide tailored guidance to patients, emphasizing the nuances of effectiveness based on personal health situations. Vaccination strategies must account for the variations in risk from COVID-19, RSV, and influenza, helping patients navigate the complexities surrounding vaccine offerings. By fostering an environment of informed decision-making, healthcare providers play a crucial role in promoting public adherence to vaccination schedules—ultimately enhancing community immunity and reducing infection rates across populations.
Public Health Guidance and the Role of Vaccine Development
As we adapt to the post-pandemic world, the significance of robust public health guidance cannot be overstated. The challenges faced during the federal vaccine advisory processes have highlighted the need for reliable, transparent, and independent evidence to inform vaccine policies. The findings from our systematic review serve as a testament to the importance of ongoing research to guide decision-making in vaccination strategies, especially as variants and epidemiological trends emerge.
Moreover, future vaccine development needs to focus on enhancing administrative processes and addressing public concerns regarding safety and efficacy. By prioritizing evidence-based approaches and leveraging comprehensive data to support vaccine recommendation frameworks, we can build public confidence and foster community engagement toward vaccine uptake. The evolution of public health guidance will play an instrumental role in navigating the complexities of respiratory viruses, ultimately shaping our approach to both existing and novel vaccines.
Evidence Synthesis as a Tool for Public Trust
The publication of comprehensive, data-driven reviews has become an essential tool for promoting trust in vaccine effectiveness and safety. As disruptions to traditional advisory processes arise, independent evidence synthesis through platforms like interactive web applications offers the necessary transparency for healthcare providers and patients alike. Making this information publicly accessible ensures that communities stay informed about the most recent vaccine developments, efficacy rates, and safety concerns.
Additionally, fostering open dialogue between healthcare providers and patients enhances the credibility of the vaccination process. By offering clear explanations and evidence-backed data, clinics can overcome vaccine hesitancy and empower patients to make well-informed decisions regarding their health. This emphasis on transparency alongside thoughtful public health communication can significantly assist in improving vaccine uptake, ensuring that populations are better protected against challenging viral threats.
The Interconnectedness of Vaccines in Protecting Public Health
Understanding the interconnectedness of COVID-19, RSV, and influenza vaccines is vital for a cohesive public health strategy. The success of one vaccination program often influences the others, particularly in regions with overlapping seasonal outbreaks. For instance, leveraging high vaccination coverage for COVID-19 may reduce overall burden on healthcare systems, allowing for more attention and resources allocated towards influenza and RSV mitigation efforts. This comprehensive approach cultivates a more adaptable and resilient public health framework.
Simultaneously, health organizations must continue to collaborate and innovate, sharing data and insights across different virus domains. By harmonizing vaccination efforts and developing integrated messaging, public health entities can maximize the benefits of immunization campaigns while addressing any emerging challenges head-on. In a world of dynamic viral circulations, this collaborative spirit will be essential in maintaining and enhancing community health amidst evolving respiratory threats.
Navigating Patient Conversations Around Vaccination
Effective communication about vaccination remains crucial in today’s health landscape. With the myriad of options available, healthcare providers must engage in thoughtful conversations with patients about individual health conditions, vaccination history, and the effectiveness of available vaccines against specific viruses. By personalizing vaccine discussions, providers can help patients better understand the benefits of COVID-19, RSV, and influenza vaccinations tailored to their unique circumstances.
Addressing patients’ concerns—such as potential side effects or safety profiles—requires transparency and evidence-based information. Empowering individuals with knowledge allows them to actively engage in their health decisions, ultimately leading to higher vaccination rates and improved outcomes. This careful, empathetic approach builds trust in healthcare systems and reaffirms the importance of immunization in safeguarding public health.
Frequently Asked Questions
How effective are COVID-19 vaccines compared to prior immunity?
COVID-19 vaccine effectiveness is estimated at 46% to 50% against hospitalization, adding additional protection atop pre-existing immunity from past infections and vaccines. The effectiveness can vary depending on the circulating strain and individual immunity backgrounds.
What is the effectiveness of RSV immunizations for older adults?
RSV immunizations show a strong effectiveness of 75% to 80% against hospitalization in adults aged 60 and older. This high effectiveness reflects a comparison between immunized individuals and those who have never received an RSV vaccine, providing substantial protection.
Are influenza vaccines effective against hospitalization in various age groups?
Influenza vaccines displayed variable effectiveness, with pooled estimates of 67% in children, 48% in working-age adults, and 42% to 53% in older adults. The effectiveness changes yearly depending on how well the vaccine matches circulating strains.
What does vaccine safety data show about COVID-19 vaccines?
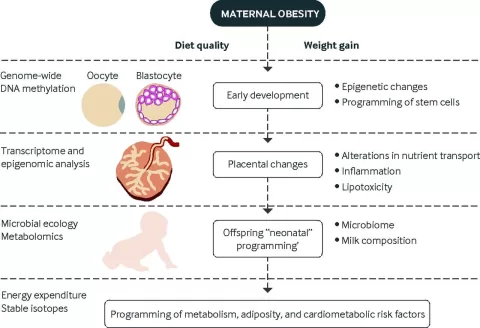
Extensive safety analysis over five years for COVID-19 vaccines indicates that myocarditis cases are rare, particularly in young males, and are significantly lower than risks from COVID infections. Safety data also demonstrate no increase in miscarriage or stillbirth risks from vaccination during pregnancy.
How does the effectiveness of RSV vaccines compare with the risk of complications like Guillain-Barre syndrome?
The RSV vaccines have shown approximately 9 excess cases of Guillain-Barre syndrome per million doses. Despite this risk, given the high hospitalization rates from RSV, the overall benefit-risk balance significantly favors vaccination, especially for older adults.
What factors influence the effectiveness of influenza vaccines?
The effectiveness of influenza vaccines can fluctuate annually based on how well the vaccine formula matches the prevalent circulating strains, ranging from 20% to over 60% depending on the year’s match quality.
How does COVID-19 vaccine effectiveness vary among different populations?
COVID-19 vaccine effectiveness varies significantly across populations. For instance, a healthy younger adult may see different benefits compared to an older adult with underlying health conditions, reflecting their unique immune profiles and prior exposures.
What is the significance of maternal vaccination for RSV in preventing infant hospitalization?
Maternal vaccination for RSV shows about 68% effectiveness in preventing hospitalization for infants through antibody transfer, representing a promising strategy for protecting vulnerable populations.
How reliable is the data regarding vaccine safety and effectiveness?
The data on vaccine safety and effectiveness comes from a systematic review of 511 studies, emphasizing transparent evidence synthesis to ensure informed decision-making in light of emerging viral strains and public health perspectives.
What should individuals understand about the different vaccines’ protection levels?
Individuals should comprehend that COVID vaccine effectiveness is incremental, RSV vaccine provides substantial protection in naive populations, and influenza vaccines offer meaningful but variable protection, all vital in preventing severe disease outcomes.
| Vaccine Type | Effectiveness Against Hospitalization | Population | Key Insights |
|---|---|---|---|
| COVID-19 Vaccines | 46% to 50% | Varies by age and pre-existing immunity | Effectiveness represents additional protection on top of existing immunity. |
| RSV Vaccines | 75% to 80% | Adults 60+ and infants | High effectiveness relative to unvaccinated; major advancements for vulnerable populations. |
| Influenza Vaccines | 42% to 67% | Children, working-age adults, older adults | Effectiveness fluctuates yearly based on strain match, with older adults benefiting from enhanced formulations. |
Summary
Vaccine effectiveness and safety are crucial aspects of public health, particularly as we enter the 2025 respiratory virus season. This comprehensive review highlights the intricacies involved in understanding vaccine efficacy across different viruses such as COVID-19, RSV, and influenza. As we decipher these numbers, it’s imperative to recognize the broader context of patient immunity and the variable effectiveness associated with different populations. With ongoing advancements in vaccine technology and safety measures established through extensive surveillance, individuals can make informed decisions on vaccinations, which remain a vital tool in reducing severe illness and hospitalization.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.