Maternal obesity is an escalating health crisis that has far-reaching implications for the next generation. Recent research highlights a concerning connection between maternal obesity and increased instances of childhood infections, particularly in children whose mothers have a body mass index (BMI) of 35 or higher. These children face a higher likelihood of hospital admissions due to infections during their formative years, emphasizing the urgent need to address maternal health risks. As the prevalence of obesity continues to rise globally, with rates jumping from 8.7% in the 1990s to 16.3% between 2010 and 2019, the implications for both maternal and child health cannot be overstated. Understanding the relationship between BMI and health is crucial for developing effective strategies to combat obesity and its associated health consequences.
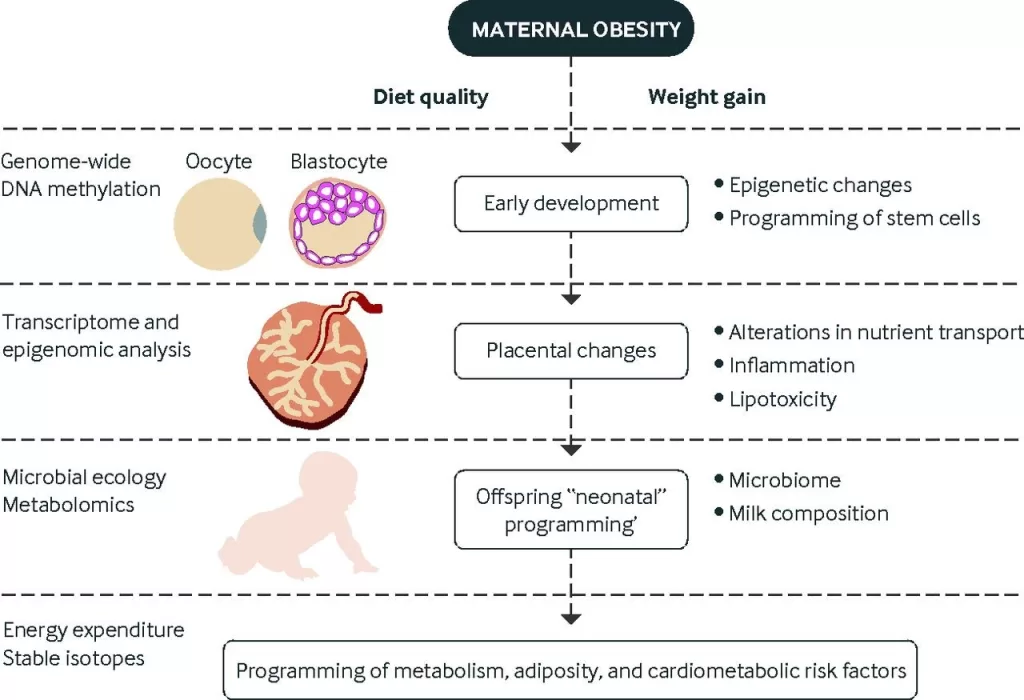
Maternal overweight and nutritional status are becoming increasingly critical topics in reproductive health discussions. The latest findings suggest that women with excessive weight gain during pregnancy are likely to deliver children with a compromised immune system, heightening the risk for various illnesses in early childhood. This phenomenon calls for extensive public health initiatives focused on the health of expectant mothers, as obesity is linked not only to childhood infections but also to broader health complications such as metabolic disorders. Engaging with these issues underlines the urgency for healthcare providers to support women in achieving optimal health prior to and during pregnancy. Overall, maternal weight management is integral to securing healthier outcomes for both mothers and their offspring.
Understanding Maternal Obesity and Its Impact on Children
Maternal obesity is not just a personal health concern; it has profound implications for the well-being of future generations. With approximately 26% of expectant mothers classified as obese (having a BMI of 35 or higher), the risks associated with this condition are drawing increasing attention from health professionals. Research indicates that obesity during pregnancy can lead to a variety of health challenges for children, notably an uptick in childhood infections. This increased risk can stem from weakened maternal immune responses and alterations in the child’s developing microbiome, which together heighten vulnerability to illnesses and can lead to hospital admissions during early childhood.
The long-term study published in BMJ Medicine highlights these alarming connections by tracking numerous births in the UK. Results show that children born to very obese mothers have a statistically significant higher risk, with an adjusted rate ratio of 1.41 for hospital admissions due to infections before age one. Such findings suggest that maternal health during pregnancy must be prioritized to safeguard the health of children, emphasizing the broad public health implications of addressing maternal obesity.
Childhood Infections and Hospital Admissions Trends
The relationship between maternal obesity and childhood infections extends beyond simple correlation; it showcases a troubling trend in health outcomes that can lead to frequent hospital admissions. According to the data analyzed, a considerable number of children are hospitalized for infections within their first five years due to maternal health risks during pregnancy. The breakdown of hospital admission rates reveals that 19% of children were admitted at least once, with a staggering 6% requiring multiple admissions. The peak age for these hospitalizations is in infancy, emphasizing the critical nature of immune development in early life, where obesity-related factors can impair this process.
Notably, the study also categorizes infections by type, observing increased admissions not only for general infections but specifically for respiratory and gastrointestinal infections. This trend underscores the complexity of how maternal obesity can affect child health, suggesting that it’s not only the direct effects on the child’s physical development but also how systemic health issues can escalate to require medical intervention. Hence, understanding these infection types plays a crucial role in developing targeted healthcare strategies to mitigate risks associated with obesity in mothers.
The Role of Maternal Health Risks in Childhood Disease
Maternal health risks, particularly concerning obesity, are increasingly recognized as significant factors in the development of childhood diseases. As indicated in the findings, children from obese mothers face heightened risks of developing various conditions, which can manifest as frequent hospital visits for infections. The study points out that conditions such as asthma and metabolic diseases are also linked to maternal obesity, leading to a cycle of health complications that can persist throughout a child’s life.
Addressing maternal obesity is crucial not only for the immediate health of the mother but also for the long-term outcomes of her children. The authors stress the importance of public health initiatives aimed at encouraging women of reproductive age to maintain a healthy BMI. By improving maternal health, we can potentially reduce the prevalence of infections in children, subsequently leading to fewer hospital admissions and a healthier population overall.
Influence of Maternal BMI on Children’s Immune System Development
The study gathered insights into how differing levels of maternal BMI can profoundly impact a child’s immune system development. With obesity being a chronic inflammatory state, mothers with higher BMI may inadvertently transmit these inflammatory markers to their children during gestation. As a result, the immune systems of these children may be compromised from the beginning, rendering them more susceptible to infections and poor health outcomes as they grow.
Furthermore, factors like maternal obesity may also interfere with the establishment of a balanced gut microbiome in children, which is essential for a robust immune response. Research continues to suggest that children born to obese mothers may experience shifts in their microbiota, leading to increased disease vulnerability. As healthcare professionals consider these aspects, they are better positioned to devise effective interventions that can improve both maternal and child health, effectively addressing the hurdles placed by maternal obesity.
The Importance of Breastfeeding in the Context of Obesity
While breastfeeding is often hailed for its protective effects on child health, the recent study presents a surprising nuance: it found that breastfeeding alone might not shield children from infections, especially those born to obese mothers. The limited scope of the study, which primarily considered breastfeeding up to six weeks postpartum, raises questions about long-term breastfeeding’s role in immune development. This observation emphasizes the need for comprehensive approaches addressing maternal obesity in conjunction with breastfeeding practices.
The benefits of breastfeeding are well-documented, ranging from reduced risks of infections to better overall health. However, for children born to mothers with obesity, additional factors, including the mother’s nutritional status and metabolic health, may complicate the potential protective effects of breastfeeding. Therefore, initiatives that promote proper maternal nutrition and sustained breastfeeding practices may be necessary to optimize health outcomes in children at risk due to maternal obesity.
Public Health Recommendations for Managing Maternal Obesity
Given the implications of maternal obesity on childhood infections and overall health, it is imperative that public health campaigns address this issue proactively. Health professionals must be equipped with the right tools and support to aid women in achieving healthy weights before, during, and after pregnancy. This can involve education on nutrition, exercise, and the importance of regular health check-ups to monitor changes in BMI and assess potential risks associated with obesity.
The findings from the BMJ Medicine study highlight a pressing need for targeted interventions aimed at reducing maternal obesity rates. Community programs that provide resources, such as nutritional counseling or weight management support, can help women make healthier choices. By addressing the root causes of obesity, we can reduce the incidence of complications, hospital admissions due to infections, and myriad health issues that arise from maternal obesity, ultimately leading to a healthier next generation.
Exploring the Link Between BMI and Long-term Child Health Outcomes
The relationship between maternal BMI and long-term child health outcomes paints a complex picture that deserves in-depth analysis. As evident from the data, increased maternal BMI is linked to a greater incidence of serious health complications in children, ranging from recurrent infections to chronic diseases later in life. Understanding this correlation is crucial for structuring effective clinical approaches and policy initiatives aimed at ameliorating these risks for the overall population.
Long-term studies like those derived from the Born in Bradford analysis provide valuable insights into the trajectory of health across generations. By recognizing the implications of maternal obesity on child health from early stages, healthcare providers can develop comprehensive strategies to monitor and support at-risk families, potentially altering the future health landscape of entire communities. Effective health strategies must combine prevention, education, and intervention to help combat the obesity epidemic and its far-reaching effects.
Childhood Asthma: A Consequence of Maternal Obesity?
Emerging evidence links maternal obesity with an increased prevalence of childhood asthma, a chronic condition that can lead to long-term health issues. The connection appears to stem from the inflammatory environment created by obesity, which may adversely affect the development of the fetal respiratory system. Understanding this relationship is critical for devising preventative measures that can alleviate the burden of asthma in children, particularly those born to obese mothers.
Moreover, asthma management in children has considerable implications for healthcare systems, given the need for frequent medical interventions, exacerbating hospital admissions. Early identification and management of at-risk children, especially those coming from a maternal background of obesity, can pave the way for better health outcomes. Public health efforts must aim at educating parents about managing asthma from early childhood while simultaneously tackling the underlying issue of maternal obesity.
Role of Healthcare Professionals in Mitigating Risks of Maternal Obesity
Healthcare professionals are at the frontline of addressing maternal health risks associated with obesity. Their role extends beyond just treatment; it encompasses education, advocacy, and support for women throughout their reproductive years. By empowering women to understand the implications of their weight on both their health and their children’s, providers can significantly impact health outcomes. Providing accessible resources and creating safe environments for discussing these issues without stigma is key.
Furthermore, healthcare systems must prioritize the training of professionals to effectively communicate the importance of healthy weight management during pregnancy. By fostering a collaborative approach that includes dietary counseling, physical activity programs, and mental health support, healthcare professionals can contribute to a marked decline in the rates of maternal obesity, resulting in improved health for mothers and their children alike.
Frequently Asked Questions
How does maternal obesity affect childhood infections in infants?
Maternal obesity, defined as a body mass index (BMI) of 30 or higher, has been linked to an increased risk of hospital admissions for infections in children. A study showed that children born to very obese mothers (BMI 35 or higher) are particularly vulnerable, facing higher rates of serious infections during their first five years of life.
What are the health risks associated with maternal obesity during pregnancy?
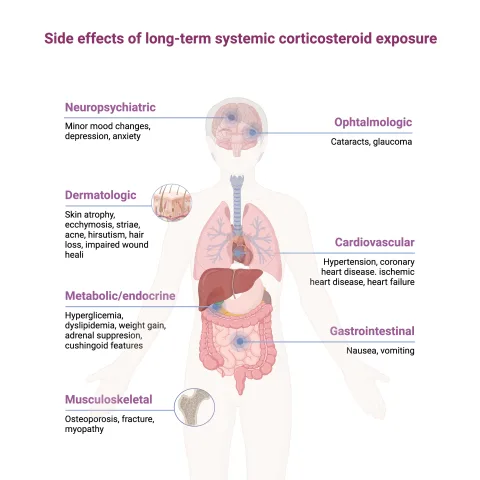
Maternal obesity poses significant health risks, including increased likelihood of gestational diabetes, hypertension, and complications during childbirth. Children born to obese mothers are also at greater risk for obesity, metabolic diseases, and infections, especially in their early years.
What is the relationship between maternal obesity and childhood asthma?
Research indicates that maternal obesity can adversely impact a child’s immune system and microbiome development, which may increase the risk of asthma in young children. This correlation arises from inflammation associated with obesity that disrupts normal immune responses.
Are hospital admissions for infection higher in children of obese mothers?
Yes, children born to mothers classified as obese have a significantly higher rate of hospital admissions for infections. Specifically, children under one year old have the highest admission rates, with increasing risk correlating with higher maternal BMI.
What public health measures are recommended to combat maternal obesity?
Public health campaigns aimed at women of reproductive age are essential to promote healthy weight management before and during pregnancy. Support from healthcare professionals is crucial in helping expectant mothers achieve and maintain a healthy BMI to reduce risks for both maternal and child health.
| Key Points | Details |
|---|---|
| Maternal Obesity and Childhood Infections | Children born to mothers with a BMI of 35 or higher are at increased risk of hospital admission for infections. |
| Study Overview | A long-term study from the Born in Bradford project analyzed 9,540 singleton births and tracked health outcomes from birth to about 15 years. |
| Obesity Statistics | 26% of expectant mothers in the study were classified as obese, with 10% categorized as grade 2 or 3 obesity. |
| Hospital Admissions Data | 5,009 hospital admissions among children were tracked; 19% had at least one admission by age 15. |
| Infection Risk Factors | Higher maternal BMI during the first trimester correlated with a greater risk of serious infections in children. |
| Types of Infections | Similar trends were found across various types of infections including respiratory and gastrointestinal. |
| Breastfeeding Findings | The study noted that breastfeeding for six weeks did not show protective benefits against infections. |
| Public Health Implications | The authors emphasized the need for campaigns to support healthy weight maintenance in women of reproductive age. |
Summary
Maternal obesity poses significant risks for childhood infections, as new research indicates that children born to very obese mothers (with a BMI of 35 or higher) are more likely to be admitted to hospitals for infections in their early years. This alarming trend suggests an urgent need for public health initiatives aimed at promoting healthy weight management among women of reproductive age to safeguard future generations from preventable health issues.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.