Prenatal syphilis screening has become a critical focus amid the alarming rise in syphilis infections among pregnant women in the United States. The US Preventive Services Task Force has definitively recommended early, universal syphilis screening during pregnancy, highlighting its importance in preventing congenital syphilis and safeguarding maternal health. With rates of congenital syphilis skyrocketing to levels not seen in decades, the need for effective STD testing for pregnant women is urgent. Following the CDC syphilis guidelines, expectant mothers are now urged to undergo testing at their first prenatal visit, ensuring timely diagnosis and treatment. As this crisis unfolds, awareness and proactive screening are essential to protect both mothers and their newborns from the serious complications associated with maternal syphilis.
Screening for syphilis during pregnancy, often referred to as maternal syphilis testing, is gaining heightened attention due to a notable increase in reported cases. The recent recommendations from health authorities advocate for comprehensive syphilis evaluations for all expectant mothers as a preventive measure against congenital syphilis, which poses severe risks to infant health. This resurgence in maternal infections has sparked a broader discussion about STD testing protocols for pregnant women, leading to critical updates in public health strategies. A reinforcement of the CDC’s guidelines on syphilis screening is imperative to combat the escalating rates of this sexually transmitted infection, ensuring that all women receive the necessary care during their pregnancy journey. As states implement mandated testing policies, the collective aim is to reverse the trend of rising maternal and congenital syphilis cases.
Importance of Prenatal Syphilis Screening
Prenatal syphilis screening is crucial for ensuring the health of both mothers and infants. According to recent guidelines from the US Preventive Services Task Force, all pregnant women should undergo screening for syphilis as soon as they enter care, ideally during their first trimester. This proactive approach significantly reduces the risk of maternal syphilis transmitting to the infant, leading to severe forms of congenital syphilis.
The Centers for Disease Control and Prevention (CDC) underscores the necessity of early syphilis detection in pregnant women. With rising congenital syphilis rates – reportedly ten times higher since 2015 – it’s essential that all healthcare providers prioritize this screening. Immediate action can make a striking difference in managing and preventing serious health complications like hearing loss and skeletal deformities in newborns.
Increasing Rates of Maternal Syphilis
The escalating maternal syphilis rates documented by the CDC, which tripled from 2016 to 2022, highlight a rising public health crisis. This alarming trend has been noted in 47 states, predominantly in the Southern United States. The surge in maternal syphilis cases poses significant health risks, not only to the mothers but also to their unborn children. As a result, states like Alabama and Texas have implemented mandatory syphilis testing protocols to combat this rising issue.
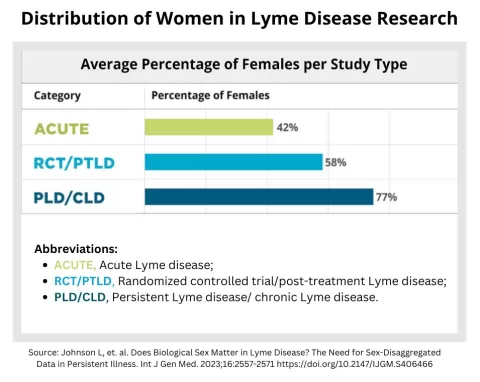
Understanding the demographics affected is critical. Non-White women show disproportionately higher rates of congenital syphilis, emphasizing an urgent need for targeted interventions. Establishing comprehensive screening protocols for syphilis during pregnancy across various healthcare settings is vital to reducing disparities in maternal and infant health outcomes.
Risks Associated with Congenital Syphilis
Congenital syphilis carries significant risks for newborns, leading to a spectrum of health issues ranging from developmental delays to severe sensory impairments. The CDC warns that infants can suffer from complications such as hearing loss, vision problems, and skeletal deformities if their mothers are untreated for syphilis during pregnancy. The latest statistics show an increasing number of congenital syphilis cases, marking a public health failure that could be mitigated through proper prenatal care.
Moreover, congenital syphilis is more than just a medical concern; it represents a systemic failure in maternal health care access, especially for marginalized communities. Preventative approaches, including routine syphilis screening during the prenatal period, could significantly reduce these risks and improve overall health outcomes for both mothers and babies, aligning with the CDC’s recommendations for STD testing for pregnant women.
CDC Recommendations for Syphilis Screening
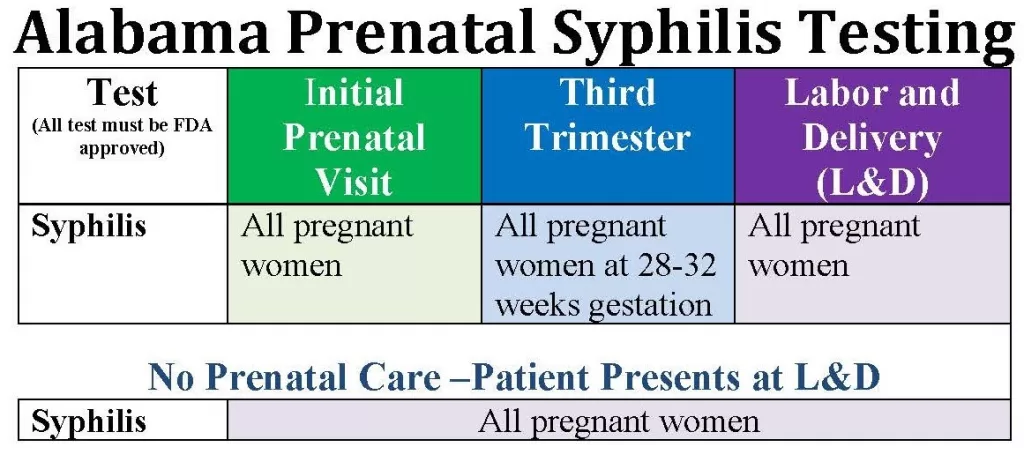
The CDC’s current guidelines advocate for universal prenatal syphilis screening, reinforcing the need for testing at key stages of pregnancy: at the first prenatal visit, during the third trimester, and at delivery. These recommendations are grounded in mounting evidence of rising syphilis rates among pregnant women and the associated risks of transmitting syphilis to their infants. By adhering to these guidelines, healthcare providers can play a crucial role in reversing this troubling trend.
Additionally, the 2023 recommendations stress that, while mandatory testing in certain states provides an important baseline, comprehensive access to testing must be made available nationwide. An integrated public health response is essential to ensure that all women benefit from prenatal syphilis screening and that congenital cases are effectively prevented.
Public Health Implications of Rising Syphilis Rates
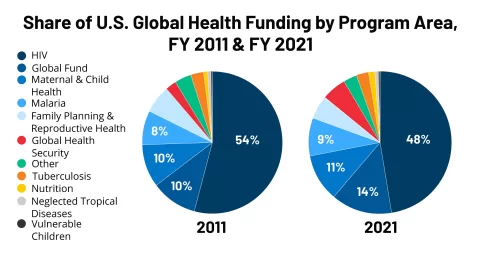
The resurgence of syphilis cases in the United States signals a critical need for revitalizing public health initiatives. The task force’s recommendations underscore the importance of effective public health infrastructure, which has been deteriorating since 2010. As the public health response shifts towards private facilities, the lack of accessible testing and care options could contribute to further increases in maternal and congenital syphilis rates.
Addressing this public health crisis requires not only compliance with screening guidelines but also a broader investment in health care education and access to services. Increased awareness of syphilis and its implications can empower more women to seek the necessary prenatal care, thus preventing the cycle of transmission and protecting future generations.
The Role of Education in Preventing Syphilis
Education plays a pivotal role in preventing syphilis and protecting maternal health. When pregnant women are well-informed about the risks associated with syphilis and the importance of timely screening, they are more likely to seek the necessary care. Comprehensive educational programs focusing on the risks of sexually transmitted infections can help destigmatize testing and encourage proactive health behaviors.
Furthermore, health care providers must be equipped with the resources to educate their patients effectively. This includes not only disseminating the latest CDC guidelines on syphilis screening during pregnancy but also addressing cultural and socioeconomic factors that may affect a woman’s ability to seek care. A well-informed approach can lead to improved health outcomes and reduce the rates of both maternal and congenital syphilis.
Community Health Initiatives and Syphilis Prevention
Community health initiatives are fundamental in combating rising syphilis rates. Programs that target vulnerable populations can help increase awareness about the importance of prenatal syphilis screening and provide much-needed resources to access testing and treatment. Collaborations between public health agencies and community organizations can foster environments that promote sexual health education and encourage regular STD testing.
Moreover, outreach efforts should focus on educating at-risk populations about maternal syphilis and the potential consequences for their infants. Empowering communities through knowledge can significantly contribute to lowering congenital syphilis rates and ensuring healthier pregnancies. Engaging local healthcare providers in these initiatives can amplify the message and enhance service delivery.
Challenges in Public Health Capacity
The decline of public health capacity poses significant challenges in addressing the syphilis epidemic. With state-mandated screening becoming increasingly common, a lack of financial and logistical support for public health initiatives exacerbates the situation. Effective contact tracing, education, and treatment programs are hindered by workforce shortages and limited funding for STD prevention efforts.
These challenges underline the need for a renewed commitment to public health infrastructure. Increasing access to prenatal care, improving syphilis screening processes, and ensuring adequate training for healthcare professionals are critical steps to control the rising rates of syphilis among pregnant women. Communities require robust systems to support preventive measures that can help reverse the alarming trends noted in recent years.
Advocacy for Stronger Policies on Syphilis Screening
Advocacy for stronger policies regarding prenatal syphilis screening is essential in combating the public health crisis. Health professionals and organizations must unite to lobby for comprehensive policies that ensure universal testing and access to care for all pregnant women. This coalition can ensure that syphilis screening becomes a non-negotiable standard of care during pregnancy,
Furthermore, advocating for policy changes to allocate more resources towards maternal health initiatives can strengthen public health infrastructures. Ensuring that all pregnant women have access to timely syphilis screening can ultimately reduce rates of congenital syphilis and protect future generations from the often devastating consequences of untreated maternal syphilis.
Frequently Asked Questions
What is prenatal syphilis screening and why is it important?
Prenatal syphilis screening involves testing pregnant women for syphilis to prevent potential complications like congenital syphilis in newborns. The U.S. Preventive Services Task Force recommends early and universal screening as it can lead to timely treatment, reducing risks of severe health issues for both mothers and infants.
When should syphilis screening during pregnancy be conducted?
Syphilis screening during pregnancy should ideally be conducted at the first prenatal visit. If not done at that time, testing should occur as soon as possible, even upon admission for delivery, to ensure maternal health and prevent congenital syphilis.
What are the CDC guidelines regarding maternal syphilis screening?
The CDC recommends universal syphilis screening for all pregnant women early in their pregnancy. This is crucial due to the alarming rise in maternal and congenital syphilis rates across the United States.
What are the risks of untreated maternal syphilis?
Untreated maternal syphilis can lead to serious complications, such as congenital syphilis in infants, which may result in hearing or vision loss, skeletal deformities, and developmental delays. Early screening and treatment can prevent these severe outcomes.
How does congenital syphilis affect newborns?
Congenital syphilis can cause a range of serious health issues in newborns, including damage to internal organs, developmental disabilities, and even stillbirth. Prenatal syphilis screening is essential to prevent these outcomes.
What trends are being observed in maternal syphilis rates?
Maternal syphilis rates have tripled from 2016 to 2022 in the United States, with significant increases reported in 47 states. This resurgence underscores the need for effective prenatal syphilis screening practices.
How can pregnant women access STD testing for syphilis?
Pregnant women can access STD testing for syphilis through healthcare providers during prenatal visits. It’s crucial to discuss testing options and follow the guidelines recommended by the CDC for optimal maternal and infant health.
What are the implications of the rise in congenital syphilis cases?
The rise in congenital syphilis cases is alarming and signals a public health crisis. Increased prenatal syphilis screening and treatment are needed to address this issue, especially since the rate of congenital infections is at its highest in decades.
Why has the CDC emphasized early syphilis screening during pregnancy?
The CDC has emphasized early syphilis screening during pregnancy to combat the rapid increase in cases of maternal and congenital syphilis, which can have devastating effects on both mothers and their infants.
What resources are available for prenatal syphilis screening information?
Resources for information on prenatal syphilis screening include the CDC guidelines, healthcare provider consultations, and maternal health organizations that offer educational materials on the importance of STD testing for pregnant women.
| Key Points | Details |
|---|---|
| US Preventive Services Task Force Recommendation | Grade ‘A’ recommendation for early, universal prenatal syphilis screening for all women. |
| Escalating Rates of Syphilis | Rates of congenital syphilis are ten times higher than in 2015, with the highest number of cases in 30 years recorded in 2023. |
| Maternal Syphilis Statistics | The rate of maternal syphilis tripled from 2016 to 2022, with significant increases reported in 47 states. |
| Risks for Non-White Women | Congenital syphilis rates are disproportionately higher in American Indian, Alaska Native, and Black populations. |
| Need for Public Health Reinforcement | The decline in public health capacity has limited syphilis testing and outbreak responses. |
Summary
Prenatal syphilis screening is crucial for the health of both mothers and their infants, as it allows for early detection and treatment of syphilis infections. With alarming rises in syphilis and congenital syphilis rates in the United States, healthcare providers must prioritize and implement these screenings to counteract the growing crisis. Addressing this issue is critical to improving maternal and infant health outcomes and restoring the downward trend in syphilis cases.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.