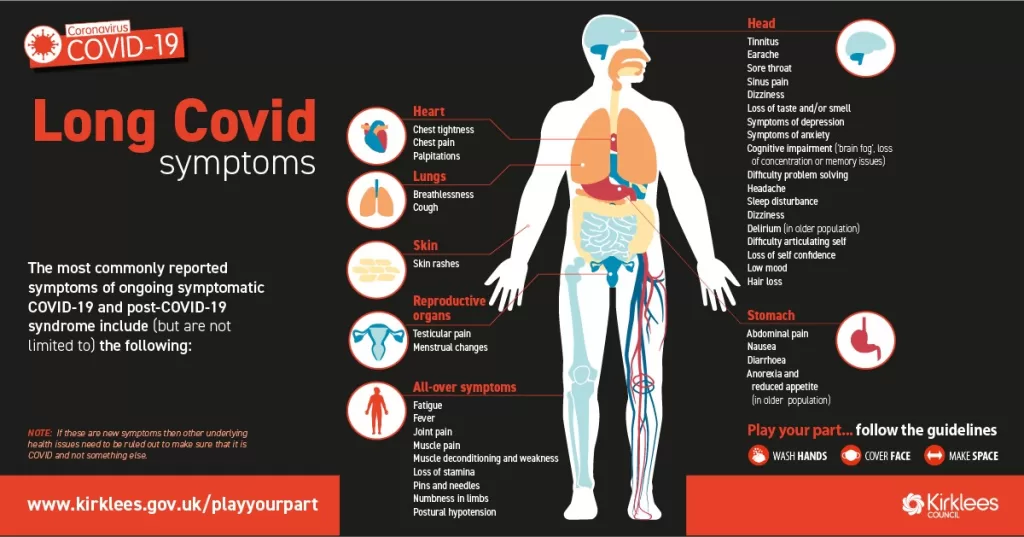
Long COVID symptoms are a significant concern for many individuals who have recovered from COVID-19. Unlike typical respiratory illnesses, long COVID presents a unique array of persistent effects that can linger for months, challenging the recovery process. Research has shown that these post-COVID syndrome symptoms, including chronic COVID fatigue, shortness of breath, and joint pain, diverge sharply from those associated with flu or pneumonia. Understanding the long-term effects of COVID-19 is crucial, as it highlights the need for comprehensive care in COVID-19 recovery. With persistent COVID symptoms affecting a substantial portion of the population, healthcare providers are increasingly focused on diagnosing and managing these conditions effectively.
Commonly referred to as post-acute sequelae of SARS-CoV-2 infection (PASC), long COVID encapsulates a range of lingering health effects following the initial COVID-19 infection. This condition is characterized by the ongoing presence of diverse symptoms that can severely impact daily life, illustrating the complexities of COVID-19 recovery. Patients often report experiences akin to chronic fatigue syndrome, experiencing debilitating energy levels and cognitive impairments that do not align with their previous health status. Moreover, the COVID-19 long-term effects extend beyond respiratory issues, encompassing neurological and psychological manifestations that further complicate recovery efforts. Ultimately, recognizing alternative terminologies is essential in fostering a more comprehensive understanding of the challenges faced by those navigating life after COVID-19.
Understanding Long COVID Symptoms
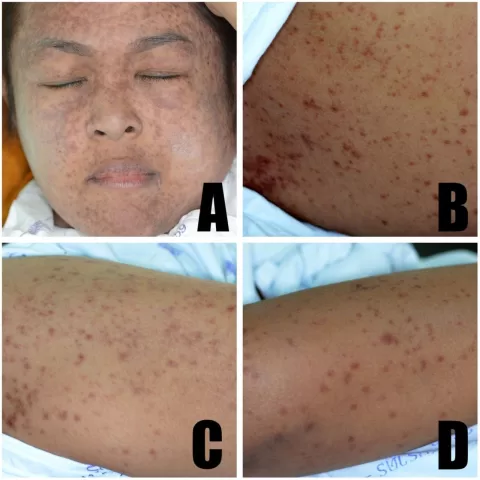
Long COVID symptoms manifest differently compared to those associated with typical respiratory infections such as the flu or pneumonia. Research shows that the unique symptom profile of long COVID includes persistent fatigue, shortness of breath, and joint pain experienced by COVID patients long after their initial infection. These setbacks arise even among individuals who had mild cases of the virus, creating a spectrum of long-term effects that can diverge widely from the recovery trajectories observed in flu or pneumonia cases.
Additionally, the duration of these symptoms tends to linger significantly longer in COVID-19 survivors, with high rates reported at multiple intervals post-diagnosis. For instance, the study noted a fatigue prevalence of 25.4% among patients four weeks post-infection. This is in stark contrast to the symptom resolution generally seen in flu and pneumonia patients, suggesting that the impact of COVID-19 can be profoundly more debilitating, thus leading to the categorization of ‘long COVID’.
Frequently Asked Questions
What are the common long COVID symptoms reported by patients?
Common long COVID symptoms include chronic COVID fatigue, shortness of breath, joint pain, and brain fog. Research has shown that over 25% of COVID-19 patients experience persistent fatigue even after four weeks post-infection, making it one of the most prevalent long COVID symptoms.
How does long COVID differ from post-COVID syndrome?
Long COVID, often referred to as post-COVID syndrome, encompasses a range of symptoms that persist long after the initial COVID-19 infection has resolved. Symptoms of long COVID can include chronic fatigue, respiratory issues, and neurological effects, distinctive from typical recovery processes seen in other illnesses like the flu.
What is the time frame for recovery from long COVID symptoms?
The recovery time for long COVID symptoms can vary significantly among individuals. While some may start to feel better within a few weeks, many individuals experience persistent COVID symptoms for months, with chronic fatigue being one of the longest-lasting effects reported.
How prevalent are long-term effects of COVID-19 among recovering patients?
Studies have indicated that a significant number of individuals who recover from COVID-19 experience long-term effects. Approximately 25% of patients report ongoing symptoms such as fatigue and respiratory issues at the four-week mark, underlining the uniqueness of long COVID compared to traditional illnesses.
Can individuals without severe COVID-19 experience long COVID symptoms?
Yes, individuals who had mild cases of COVID-19 can still experience long COVID symptoms. Research shows that even those with less severe illness severity may develop persistent symptoms like fatigue, brain fog, and anxiety.
What chronic conditions exacerbate long COVID symptoms?
Chronic conditions such as rheumatoid arthritis, ischemic heart disease, and asthma have been shown to increase the odds of experiencing long COVID symptoms. Patients with these comorbidities often face a greater risk for persistent symptoms beyond the acute phase of COVID-19.
How do the symptoms of long COVID compare to flu or pneumonia?
Long COVID symptoms are distinct from those experienced after flu or pneumonia. Unlike flu or pneumonia, where symptoms typically resolve over time, long COVID can cause ongoing issues such as chronic fatigue and brain fog, which are not commonly reported in flu recovery patterns.
Are there any demographic differences in experiencing long COVID symptoms?
Yes, research indicates that different demographic groups experience long COVID symptoms variably. For instance, white patients have reported higher instances of anxiety and chronic fatigue compared to their Asian, Black, and Hispanic counterparts.
What are the implications of ongoing long COVID symptoms for patient care?
Patients experiencing long COVID symptoms may require additional support and tailored treatment plans focused on managing chronic conditions and addressing persistent symptoms. Understanding the unique nature of long COVID is crucial for effective recovery strategies.
Is there a correlation between COVID-19 severity and the risk of long COVID symptoms?
Yes, there is a correlation between the severity of COVID-19 and the likelihood of developing long COVID symptoms. Individuals who experienced more severe infections are more likely to report ongoing symptoms such as chronic fatigue and shortness of breath.
| Key Point | Details |
|---|---|
| Long COVID Symptoms | Long COVID features unique symptoms that persist longer than those of flu or pneumonia. |
| Study Context | The research analyzed health claims data from over 121,205 COVID-19 patients and compared them to flu and pneumonia patients. |
| Common Symptoms Post-Infection | Fatigue, shortness of breath, and joint pain are the most common symptoms in long COVID. |
| Symptom Duration | Symptoms persisted more in the most severe COVID-19 cases compared to flu or pneumonia. |
| Impact of Severity and Comorbidities | Higher severity levels are associated with increased odds of persistent symptoms. |
| Demographic Differences | Certain demographic groups show varied symptom experiences related to long COVID. |
Summary
Long COVID symptoms represent a significant concern as they extend well beyond what is typically seen in flu or pneumonia cases. Research indicates that individuals suffering from COVID-19 experience prolonged symptoms like fatigue, shortness of breath, and joint pain for weeks and even months after the initial infection. This condition, distinct from the recovery timelines of other respiratory illnesses, underscores the unique challenges faced by COVID-19 survivors. Furthermore, demographic factors and pre-existing health conditions play a role in the severity and persistence of these long COVID symptoms, highlighting the need for ongoing research and tailored treatment approaches for affected populations.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.