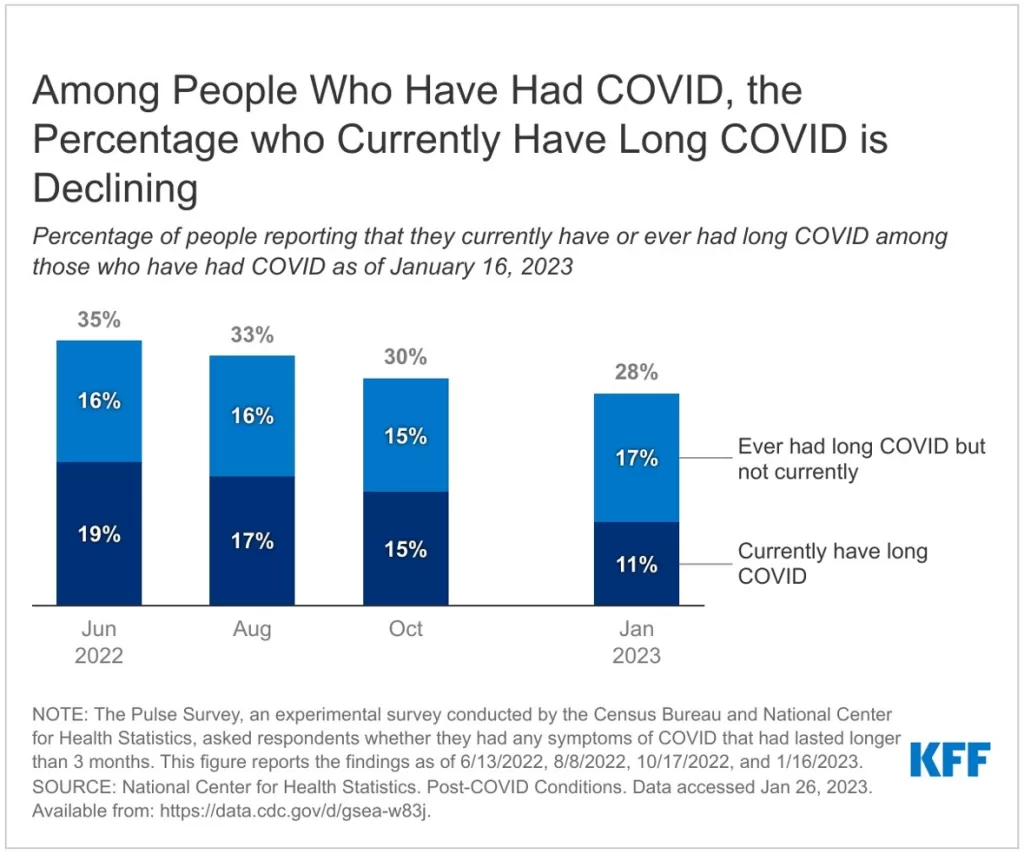
Long COVID prevalence has emerged as a critical concern in global health discussions following the COVID-19 pandemic. A recent study in BMJ Global Health revealed that about 25% of individuals who experienced symptomatic COVID-19 reported persistent symptoms, highlighting the long-lasting impact of the virus. This phenomenon appears to be particularly acute in less affluent nations and among specific demographic groups, such as individuals of Arab or North African descent. Compounding the issue, another long COVID study from China indicated that over 30% of surveyed patients experienced lingering effects that significantly disrupted their daily lives. The healthcare challenges posed by these symptoms underscore the ongoing COVID-19 recovery crisis, necessitating urgent attention to the management and treatment of long COVID symptoms across diverse populations.
The ongoing effects of COVID-19 have led to the emergence of post-viral syndromes, commonly referred to in the medical community as long COVID. This condition manifests through various lingering health issues that can severely hinder recovery and quality of life. Research indicates that a considerable fraction of those affected report debilitating symptoms that persist long after the acute phase of the infection has resolved. Notably, individuals from economically disadvantaged backgrounds and specific ethnic groups face heightened risk and prevalence of these enduring conditions. Understanding the broader implications of these long-term health challenges is essential to address the overarching impact of COVID-19 on global public health systems.
Understanding Long COVID Prevalence Across Global Populations
Long COVID prevalence varies widely across different demographics and geographic regions. Recent studies have revealed that approximately 25% of patients who experienced symptomatic COVID-19 reported lasting symptoms long after their initial infection. This rate is alarmingly higher among individuals from low-income countries, reaching up to 30.2% in studies conducted in places like China. Such findings underscore the widespread effects of COVID-19 recovery on public health globally, highlighting the urgent need for targeted healthcare strategies.
Notably, a pronounced disparity exists when examining long COVID symptoms among ethnic groups. Data indicates that individuals of Arab or North African descent have the highest reported prevalence at 36.1%. This highlights critical healthcare challenges faced by these populations, particularly in the aftermath of COVID-19. It emphasizes the importance of conducting long COVID studies that focus on diverse demographics to better understand the unique challenges they encounter.
The Impact of Long COVID Symptoms on Daily Life
The debilitating nature of long COVID symptoms significantly impairs daily functioning, affecting everything from work productivity to social engagements. In a survey involving nearly 3,700 patients in China, 30.2% of respondents reported experiencing at least one long COVID symptom that persisted for six months post-infection. Among these, symptoms like fatigue, sleep disorders, and joint pain were most prevalent. The impact of these symptoms can lead to prolonged health complications and raise concerns regarding the long-term recovery from COVID-19.
Individuals struggling with long COVID often find themselves facing daily challenges that can hinder their quality of life. Many report that cognitive issues, often referred to as ‘brain fog,’ exacerbate their struggles, making even simple tasks daunting. Understanding the multifaceted impact of long COVID symptoms is essential for developing effective treatment protocols and support systems to aid recovery and enhance the quality of life for those affected.
Healthcare Challenges Faced by Long COVID Patients
Long COVID presents significant healthcare challenges that require immediate attention from medical professionals and health policymakers alike. The need for a robust framework to address the ongoing health issues faced by survivors of COVID-19 cannot be overstated. As studies show a concerning prevalence rate of long COVID, especially among individuals who were hospitalized or had underlying health issues, healthcare systems are left under strain, struggling to manage the influx of patients presenting chronic post-acute sequelae.
Additionally, the increasing costs related to long COVID treatment are expected to place a heavy burden on healthcare resources, particularly in countries that are already facing economic constraints. The observation that lower middle-income countries report higher long COVID rates emphasizes a critical need for investment in healthcare infrastructure to adequately address this public health crisis. There is an urgent call for more focused long COVID studies and research into effective treatment options that address the unique health profiles of affected populations.
Demographic Correlations with Long COVID Risks
Recent research highlights key demographic correlations with long COVID risks that may inform healthcare strategies and public health policies. Older age and female gender have been identified as significant risk factors for developing long COVID symptoms. This finding emphasizes the importance of tailoring long COVID recovery programs that prioritize the needs of older adults and women, potentially through dedicated healthcare services designed for these vulnerable populations.
Moreover, the data suggests that COVID-19 re-infection raises the risk of experiencing long COVID symptoms even further. This reinforces the necessity for preventive measures such as vaccinations and public awareness campaigns, especially in communities where the disease’s impact is more pronounced. Addressing these demographic factors can facilitate more effective long-term management of COVID-19 recovery efforts.
Long COVID and its Socioeconomic Implications
The socioeconomic implications of long COVID are profound, particularly for individuals from lower-income backgrounds who may already be facing various challenges. As highlighted in studies, the prevalence of long COVID symptoms is markedly higher among populations in middle- and low-income countries. This raises concerns about the existing disparities in health equity, access to care, and resources available for those needing long-term support and management.
The long-term impact of COVID-19 on economic stability is yet to be fully realized, but early indicators suggest that it may contribute to increased inequality. Patients with long COVID often experience decreased work capacity, leading to financial strains not only on themselves but also on the broader community. Policymakers must recognize these issues and work towards implementing policies that support affected individuals economically, socially, and medically.
Coping Strategies for Long COVID Patients
Coping with long COVID requires a multifaceted approach that encompasses physical, emotional, and mental health support. Patients and their families are encouraged to engage in personalized rehabilitation plans that may include physical therapy, mental health counseling, and nutritional support. Developing a strong support network can significantly aid individuals facing the myriad challenges associated with long COVID, boosting their resilience.
Additionally, exploring alternative therapies along with conventional medicine might benefit some patients in their recovery journey. For instance, starting traditional practices such as mindfulness or gentle yoga could potentially alleviate symptoms like fatigue and stress, contributing to improved overall well-being. To navigate the complexities of long COVID, it’s essential for patients to actively seek resources and self-care strategies tailored to their unique experiences.
The Role of Healthcare Professionals in Long COVID Management
Healthcare professionals play a crucial role in the management and treatment of long COVID patients. Identifying and recognizing the symptoms associated with long COVID is essential for effective continuity of care. Clinicians must stay informed about the latest long COVID studies and share this knowledge with patients, providing them with accurate information regarding their recovery process and possible symptoms to look out for.
Moreover, fostering a collaborative relationship between patients and healthcare providers can enhance treatment success. Support groups and regular check-ins can open the lines of communication, allowing professionals to track recovery progress closely and make necessary adjustments to treatment plans. Ultimately, a proactive approach within the healthcare community could lead to improved outcomes for those afflicted by long COVID.
Ongoing Research into Long COVID
The urgency for ongoing research into long COVID cannot be overstated, as millions of individuals worldwide continue to experience lingering symptoms long after their initial COVID-19 infection. Current studies are focusing on the pathophysiology of long COVID, seeking to understand how the virus affects various organ systems and the underlying mechanisms that contribute to persistent symptoms. A comprehensive understanding of these factors is crucial for developing effective treatment protocols.
Moreover, long COVID studies aiming at diverse populations can yield valuable insights into how different ethnicities and socioeconomic backgrounds might influence recovery outcomes. Such research efforts are fundamental in informing public health strategies and healthcare policies, ensuring equitable treatment and support for all survivors of COVID-19. Collaboration among researchers, healthcare providers, and affected communities is vital for a comprehensive approach to tackling long COVID.
Community Support for Long COVID Patients
Community support systems can play a pivotal role in the recovery journey of long COVID patients, providing essential resources that foster resilience and hope. Organizations can facilitate peer support networks where individuals share experiences, coping strategies, and encouragement, ultimately reducing feelings of isolation that often accompany prolonged illness.
Additionally, raising awareness within communities about the prevalence and impact of long COVID is crucial for garnering support for those affected. Initiatives that promote education and understanding can help mitigate stigma and encourage compassion among community members, paving the way for a collective approach to supporting long COVID patients in their quest for better health.
Frequently Asked Questions
What is the prevalence of long COVID among COVID-19 patients?
Recent studies indicate that approximately 25% of patients report long COVID symptoms after symptomatic COVID-19. Particularly, 30.2% of COVID-19 patients surveyed in China experience at least one persistent long COVID symptom, demonstrating a significant prevalence of long COVID across various populations.
How do long COVID symptoms differ by geographical region?
Long COVID prevalence tends to vary by region. The first study noted a prevalence of 29.8% among patients from lower middle-income countries, compared to 14.4% from high-income nations, highlighting how socioeconomic factors impact long COVID symptoms and healthcare challenges.
What demographic factors contribute to long COVID prevalence?
Demographic factors such as age, gender, and ethnicity significantly influence long COVID prevalence. The highest rates were observed in patients of Arab or North African descent and those aged over 50. Additionally, re-infection with COVID-19 also correlates with an increased risk of developing long COVID.
What types of long COVID symptoms are most commonly reported?
Common long COVID symptoms reported include sleep disorders (12.8%), joint pain (9.8%), fatigue (8.7%), and headaches (8.1%). These symptoms can significantly affect the quality of life and daily functioning of individuals recovering from COVID-19.
How does hospitalization impact long COVID prevalence?
Hospitalized COVID-19 patients face a higher risk for long COVID symptoms, with a study indicating an adjusted odds ratio (aOR) of 2.04 for those experiencing long COVID, compared to non-hospitalized patients. This emphasizes the need for ongoing care and monitoring post-discharge.
What role does socioeconomic status play in long COVID prevalence?
Socioeconomic status is a critical factor in long COVID prevalence. The data shows that lower middle-income countries report nearly double the prevalence of long COVID symptoms compared to high-income countries, indicating that existing healthcare challenges exacerbate health issues in lower income regions.
Are there any protective factors against developing long COVID?
Certain factors appear to mitigate the risk of long COVID, including the use of traditional Chinese medicine and receiving more than three doses of the COVID vaccine. These factors may help in reducing the severity or duration of long COVID symptoms for certain individuals.
What can be done to address the healthcare challenges posed by long COVID?
Addressing healthcare challenges associated with long COVID requires comprehensive healthcare planning, increased research funding, and improved healthcare access, especially in low-income regions. Collaborative international studies can enhance understanding and treatment approaches for long COVID, benefiting affected populations globally.
| Key Points | Description |
|---|---|
| Study Overview | A BMJ Global Health study across 13 middle- and high-income countries analyzed long COVID prevalence. |
| Prevalence Rate | 25% of symptomatic COVID-19 patients reported long COVID symptoms. |
| Demographic Impact | Higher prevalence in participants from less affluent nations and among those of Arab/North African descent (36.1%). |
| Symptoms | Common symptoms included sleep disorders (12.8%), joint pain (9.8%), fatigue (8.7%), and headaches (8.1%). |
| Economic Burden | Countries that are less equipped for healthcare are likely to bear a greater burden from long COVID-related costs. |
| Age and Gender Factors | Older age, female gender, and COVID re-infection increase the risk of long COVID symptoms. |
| Protective Factors | Using traditional Chinese medicine and receiving more than three vaccine doses may reduce long COVID risk. |
Summary
Long COVID prevalence continues to be a pressing issue, with studies indicating significant rates among COVID-19 survivors. In particular, research shows that 25% of patients who experienced symptomatic COVID-19 suffer from persistent symptoms, with higher rates observed in certain demographics. The burden of long COVID is disproportionately felt in lower-income countries and among specific ethnic groups, underscoring the need for targeted healthcare strategies. Overall, understanding long COVID prevalence is essential for shaping public health responses and ensuring that affected individuals receive the necessary support and treatment.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.