Type 1 diabetes (T1D) is an autoimmune disease that can significantly increase an individual’s risk of developing other autoimmune diseases as well. With the Centers for Disease Control and Prevention reporting that 1.7 million adults and numerous children live with T1D in the United States, understanding the comorbid autoimmune diseases linked to this condition becomes crucial. Those diagnosed with T1D face a higher likelihood of complications, ranging from hypothyroidism to celiac disease, which can complicate their daily management of diabetes. This interrelation highlights the need to be aware of autoimmune disease risk factors as part of a comprehensive approach to managing type 1 diabetes effectively. Patients can benefit from education and lifestyle adjustments to mitigate these risks and maintain optimal health.
Type 1 diabetes, commonly referred to as T1D, is not just a standalone condition but rather a catalyst for various other autoimmune disorders that can complicate a patient’s health. Often stemming from a malfunctioning immune system, individuals with T1D may find themselves battling additional health issues, known as comorbid autoimmune diseases, which can hinder their overall well-being. These interconnected medical challenges exemplify the complexity that patients with this type of diabetes face daily. To effectively manage diabetes and mitigate complications, it is essential to recognize the risk factors associated with autoimmune diseases. Thus, a holistic approach that includes lifestyle changes and ongoing medical support becomes imperative for those navigating the difficulties of type 1 diabetes and its associated conditions.
Understanding Type 1 Diabetes and Autoimmune Disease Connections
Type 1 diabetes (T1D) is an autoimmune condition where the immune system mistakenly attacks insulin-producing beta cells in the pancreas. This disruption leads to elevated blood glucose levels and requires ongoing management. Interestingly, T1D is not just a singular condition; it is associated with a wide range of comorbid autoimmune diseases. Understanding these connections is vital as patients with T1D risk developing additional autoimmune disorders that can complicate their diabetes management and overall health.
Recent studies indicate that approximately one in five individuals with T1D will face an additional autoimmune disease, with ailments such as hypothyroidism and celiac disease being common. These coexisting conditions can exacerbate insulin resistance and complicate the glycemic control required for effective diabetes management. By acknowledging the relationship between T1D and other autoimmune diseases, healthcare providers can offer improved care and guidance to patients navigating these challenges.
Complications of Type 1 Diabetes and Autoimmune Disorders
The presence of multiple autoimmune diseases can lead to several complications for those with Type 1 diabetes. For instance, diabetic retinopathy, nephropathy, and neuropathy are common long-term complications that can worsen with other autoimmune conditions. The interconnection between T1D and disorders such as rheumatoid arthritis or lupus can result in heightened inflammation and increased insulin resistance, which can pose additional difficulties in managing blood sugar levels effectively.
Moreover, autoimmune conditions may introduce their own set of complications. For example, conditions like autoimmune gastritis or thyroid autoimmune disorders can adversely affect metabolism and nutrient absorption, creating a vicious cycle that complicates diabetes management. It becomes essential for individuals with T1D to monitor not only their blood glucose levels but also the symptoms of other potential autoimmune disorders in order to maintain their health and quality of life.
Autoimmune Disease Risk Factors in Type 1 Diabetes Patients
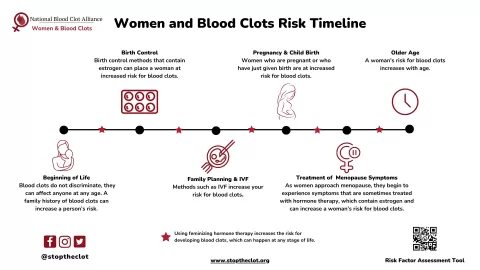
Patients with Type 1 diabetes often face increased risk factors for subsequent autoimmune diseases due to shared genetic markers and immune dysregulation. This heightened susceptibility can be linked to specific environmental triggers, stress levels, and lifestyle choices that impact immune function. For example, exposure to certain viral infections or dietary gluten in predisposed individuals may initiate the onset of conditions like celiac disease in those with T1D.
Additionally, research highlights the importance of understanding gender differences in autoimmune disease prevalence, as many autoimmune disorders disproportionately affect women. This factor, compounded with lifestyle factors such as diet and physical health, can further complicate the risk profile for individuals living with T1D. Awareness of these risk factors is crucial for proactive monitoring and management, allowing for timely interventions and education regarding potential autoimmune threats.
Managing Type 1 Diabetes With Comorbid Autoimmune Diseases
Managing Type 1 diabetes alongside other autoimmune diseases requires a comprehensive and tailored approach. Effective diabetes management strategies must take into account the unique challenges posed by coexisting autoimmune conditions. Regular medical check-ups, personalized dietary plans, and tailored exercise regimens can help mitigate risks and improve overall health outcomes for patients with T1D and other autoimmune diseases.
Moreover, mental health should not be overlooked in this multifaceted management strategy. Conditions like depression and anxiety can arise from the stress of managing multiple chronic conditions. Therefore, a holistic approach that includes psychological support and education about both diabetes and its associated autoimmune risks can enhance quality of life and empower patients in their self-care practices.
Lifestyle Modifications to Reduce Autoimmune Disease Risks
Adopting a healthy lifestyle is integral for reducing the risk of developing further autoimmune diseases among individuals with Type 1 diabetes. This encompasses balanced nutrition, regular physical activity, stress management techniques, and adequate sleep. Engaging in these practices can boost immune function, enhance metabolic health, and reduce the incidence of diabetes-related complications.
Particularly important are dietary choices that consider the potential for celiac disease and other autoimmune reactions. A diet rich in whole foods, low in processed sugars, and tailored to individual health needs can help manage blood glucose and support immune health. By being proactive about lifestyle modifications, patients can significantly impact their ability to manage T1D and potential comorbid autoimmune diseases.
Insights into the Genetics of Type 1 Diabetes and Autoimmunity
Genetic predisposition plays a pivotal role in the development of both Type 1 diabetes and related autoimmune diseases. Research suggests that certain shared genetic markers increase the propensity for immune system dysfunction, leading to multiple autoimmune disorders. Understanding these genetic factors can provide insights not only into disease onset but also into personalized treatment approaches that may reduce the risk of developing additional conditions.
Ongoing studies are investigating the genetic interplay between T1D and other autoimmune diseases, refining our understanding of why certain individuals are more susceptible than others. These insights can ultimately guide genetic screening practices, inform at-risk individuals of their potential for additional autoimmune conditions, and enhance ongoing research efforts focused on prevention and treatment strategies.
The Role of Environmental Triggers in Autoimmune Disease Development
Environmental factors are critical in the interplay between Type 1 diabetes and the development of other autoimmune conditions. Studies have indicated that triggers such as infections, toxins, and even dietary elements like gluten can potentially initiate autoimmunity. Recognizing these environmental influences can empower individuals with T1D to modify their environments for better health outcomes.
By being aware of these environmental triggers, patients can adopt preventative measures to mitigate exposure. This proactive approach is crucial in managing autoimmune conditions and promoting long-term health, particularly for those already navigating the complexities of Type 1 diabetes. Collaborative efforts among healthcare providers, patients, and researchers will further illuminate the significant impact of these factors.
Mental Health Considerations for Type 1 Diabetes Patients
Mental health is a critical component often overlooked in the management of Type 1 diabetes and its associated autoimmune conditions. Patients frequently experience heightened anxiety and depression due to the chronic nature of their illnesses and the daily challenges of managing diabetes alongside potential autoimmune diseases. Recognizing and addressing these mental health concerns is imperative to improving the overall well-being of T1D patients.
Integrating mental health support into diabetes care can provide patients with coping strategies, reducing the stress associated with managing multiple health conditions. Mindfulness practices, counseling, and support groups can offer significant relief, improving the patients’ quality of life and resilience in facing their dual challenges of T1D and other autoimmunity-related issues.
Research Frontiers: Curing Type 1 Diabetes and Autoimmunity
The quest to cure Type 1 diabetes while addressing autoimmune responses is an area of active research. Emerging therapies are focused on directly targeting autoimmunity to halt the progression of diabetes and its complications. Advances in immunotherapy, gene therapy, and regenerative medicine hold promise for altering the course of disease and preventing the onset of additional autoimmune conditions in susceptible individuals.
Equally important is understanding how new treatment strategies impact the overall immune system. Balancing the need for interventions that mitigate autoimmunity while preventing further complications associated with T1D is essential. Ongoing clinical trials and studies are critical in paving the way toward innovative solutions for managing Type 1 diabetes and enhancing patient outcomes in the face of comorbid autoimmune diseases.
Frequently Asked Questions
How does Type 1 diabetes increase the risk of other autoimmune diseases?
Type 1 diabetes (T1D) increases the risk of other autoimmune diseases due to shared genetic foundations that influence immune function. Studies indicate that approximately one-fifth of individuals with T1D also develop comorbid autoimmune conditions such as hypothyroidism, celiac disease, and rheumatoid arthritis. These conditions can complicate diabetes management by increasing insulin resistance or affecting glycemic control.
What are common comorbid autoimmune diseases associated with Type 1 diabetes?
Common comorbid autoimmune diseases associated with Type 1 diabetes include hypothyroidism, celiac disease, autoimmune gastritis, vitiligo, adrenal insufficiency, and lupus. Individuals with T1D often have shared genetic markers that predispose them to these additional autoimmune conditions, making patient education about these risks essential for effective management.
What lifestyle changes can help manage Type 1 diabetes and reduce autoimmune disease risks?
To manage Type 1 diabetes and potentially mitigate the risk of developing additional autoimmune diseases, patients are advised to adopt a healthy lifestyle that includes eating a balanced diet, exercising regularly, maintaining a consistent sleep schedule, managing stress, and avoiding environmental toxins. Regular medical checkups can help in early detection and management of any emerging autoimmune conditions.
How can stress and environmental factors influence autoimmune diseases in Type 1 diabetes?
Stress and environmental triggers have been shown to play a significant role in the development and exacerbation of autoimmune diseases in individuals with Type 1 diabetes. Literature suggests that stress-related life circumstances can increase susceptibility to autoimmune conditions. Reducing stress and addressing environmental factors may help in managing both T1D and associated autoimmune risks.
Is there a proven method to prevent autoimmune diseases in individuals with Type 1 diabetes?
Currently, there is no proven method to prevent the onset of additional autoimmune diseases in individuals with Type 1 diabetes. However, being vigilant about new symptoms and maintaining a proactive healthcare approach through regular monitoring can help in early identification and treatment of potential comorbid conditions.
What role does genetic predisposition play in Type 1 diabetes and autoimmune diseases?
Genetic predisposition plays a crucial role in both Type 1 diabetes (T1D) and associated autoimmune diseases. Shared genetic markers contribute to an overactive immune response, increasing the likelihood of developing conditions such as autoimmune thyroid disorders and celiac disease among those with T1D. Understanding these genetic connections is essential for risk assessment and management.
Can Type 1 diabetes complications interact with other autoimmune diseases?
Yes, complications from Type 1 diabetes can interact with other autoimmune diseases, complicating overall disease management. Conditions like gastroparesis and chronic kidney disease can arise from poor glycemic control and may coincide with other autoimmune disorders, thereby increasing insulin resistance and complicating treatment regimens.
What are the signs and symptoms of autoimmune diseases that Type 1 diabetes patients should monitor?
Individuals with Type 1 diabetes should monitor for new symptoms that may indicate the onset of autoimmune diseases, such as unexplained weight loss, chronic fatigue, digestive issues, or changes in mood and energy levels. Awareness of these signs is critical for prompt medical evaluation and intervention.
How prevalent are autoimmune diseases in individuals with Type 1 diabetes?
Autoimmune diseases are notably prevalent in individuals with Type 1 diabetes, with studies suggesting that nearly 20% may develop at least one other autoimmune condition. Autoimmune thyroid disorders and celiac disease are particularly common, highlighting the necessity for regular screening and education on associated risks.
| Key Points | Details |
|---|---|
| Prevalence of Type 1 Diabetes | 1.7 million adults and 304,000 children and adolescents affected in the U.S. |
| Daily Management Challenges | 42 factors influence blood glucose levels; one-third of daily choices affected by T1D. |
| Long-term Complications | Includes diabetic retinopathy, nephropathy, neuropathy, cardiovascular disease, and more. |
| Increased Risk of Other Autoimmune Diseases | 1 in 5 individuals with T1D have at least one comorbid autoimmune condition. |
| Common Autoimmune Conditions Associated with T1D | Includes hypothyroidism, celiac disease, rheumatoid arthritis, lupus, and more. |
| Factors for Autoimmunity | Shared genetic markers, overactive immune response, environmental triggers, and stress. |
| Lifestyle Recommendations | Healthy diet, exercise, stress reduction, and regular medical checkups advised. |
| Research and Prevention Efforts | Ongoing research into curing T1D and emerging therapies for autoimmunity. |
Summary
Type 1 diabetes autoimmune diseases represent a significant health concern, significantly impacting the management and quality of life of those affected. Individuals with Type 1 diabetes face a heightened risk for various other autoimmune disorders, such as hypothyroidism and celiac disease, due to shared genetic factors and immune system characteristics. Understanding these risks and implementing preventative lifestyle measures can help mitigate the complications associated with Type 1 diabetes and improve patient outcomes.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.