Viruses in human semen have garnered significant attention due to their implications for sexual transmission and reproductive health. Recent research, including a comprehensive review of 373 studies, has identified 22 viruses capable of being detected in semen following acute infections, which includes pathogens known for their pandemic potential. Among these, only 9 viruses exhibit evidence of transmission through sexual activity, underscoring the complex interaction between male reproductive fluids and infectious diseases. Notably, the study highlights persistent threats such as Zika and Ebola viruses, which continue to be viable in semen long after initial illness. Understanding viral persistence in semen is critical for public health strategies aimed at mitigating the risks of viral transmission during intimate contact and combating outbreaks effectively.
The presence of infectious agents in male reproductive fluids presents a unique challenge in addressing sexually transmitted infections and other viral diseases. Recent findings have illuminated the various viruses that linger in human semen post-infection, raising alarms about potential modes of transmission and long-term health consequences. This includes high-profile viruses such as the Ebola virus and Zika virus, which have been associated with severe reproductive and developmental issues. The study’s insights into viral longevity in semen not only inform the landscape of sexual health but also provide crucial data for vaccine development against these persistent pathogens. As we delve deeper into the understanding of sexual transmission pathways, it becomes imperative to explore how these viruses navigate the complexities of human physiology.
Understanding Viruses in Human Semen: A Systematic Review
A new systematic review published in The Lancet Microbe examines an alarming finding: 22 viruses can be detected in human semen following acute infections. This extensive study encompasses 373 individual investigations, all shedding light on the implications of viruses that possess pandemic potential. The review emphasizes the critical nature of sexually transmitted infections and their capability to persist within the male reproductive system. Notably, only a fraction of these viruses—nine out of the 22—demonstrated clear evidence of sexual transmission, underlining the nuances involved in viral persistence in semen.
The persistence of these pathogens in human semen raises crucial questions for public health and reproductive safety. As ongoing disease transmission poses a significant risk, understanding how these viruses interact and sustain themselves in male reproductive fluids becomes paramount. The findings from this review are significant not just for their immediate implications for patient health, but also for the future of vaccine development and therapeutic interventions against virulent pathogens that can remain viable long after the resolution of acute symptoms.
Viral Persistence in Semen and its Implications
Viral persistence in semen is a multifaceted issue that poses potential risks for both individual health and broader public health. The study highlights that certain viruses, particularly the Ebola virus, can remain detectable in semen for extended periods—up to 988 days in some cases. This prolonged presence may facilitate sexual transmission, exacerbating public health concerns surrounding the spread of infectious diseases. By evaluating the duration that various pathogens can survive in human semen, researchers can better understand transmission pathways and inform strategies to mitigate risks associated with viral outbreaks.
In contrast, other viruses demonstrated shorter persistence, such as the Kyasanur Forest disease virus, which was detectable for only 8 days post-onset. Such variations underline the necessity of tailored public health responses depending on specific viral characteristics. Understanding how long viruses like Zika and Ebola endure in semen not only helps in managing individual cases but also contributes to the larger conversation about the sexual transmission of viruses and the preventive measures that should be in place for sexually active populations, especially in regions experiencing outbreaks.
Strategies must be developed to address the potential risks associated with sexual transmission of viruses, particularly in regions with ongoing outbreaks. Governments and health organizations must prioritize education and awareness regarding these pathogens, the sexual transmission routes, and the need for safe practices to prevent further spread.
Recent Outbreaks and Their Association with Semen-Borne Viruses
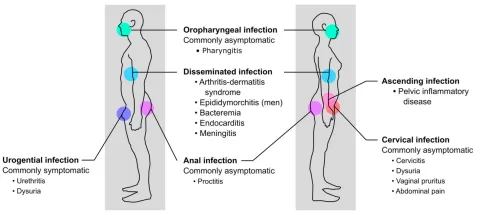
Recent outbreaks of Zika virus disease and Ebola virus disease have highlighted the alarming potential for viral pathogens to be transmitted through sexual contact. The systematic review underscores this connection by discussing the evidence of viruses detected in human semen following acute infections. Such findings are crucial for understanding the dynamics of viral spread in vulnerable populations. For instance, the persistence of Zika virus in semen for an average of 57 days suggests a continuous risk of sexual transmission even after recovery from the initial infection, complicating public health responses.
The implications extend beyond immediate health outcomes, as the transmission of such viruses can lead to devastating consequences, including congenital anomalies like microcephaly associated with Zika infection. This calls for further research to explore vertical transmission avenues and identify strategies to educate affected populations on the importance of sexual health and disease prevention. Continuous monitoring and public health initiatives are necessary to curtail the spread of these viruses and preserve reproductive health.
The Role of Sexual Transmission in Infectious Disease Spread
The sexual transmission of viruses is a growing concern in the context of infectious diseases, especially given the findings from the systematic review regarding the detection of 22 viruses in human semen. This aspect significantly complicates the management and control of viral outbreaks, as it introduces another vector for transmission that may not be adequately addressed by standard public health measures. In particular, the review notes that while not all detected viruses exhibit evidence of sexual transmission, the potential for those that do poses substantial risks for sexual health and community wellbeing.
To further complicate matters, the variability in the duration of virus persistence in semen among individuals implies that health guidelines must be adaptable and based on the latest research. Public health authorities need to establish comprehensive frameworks that address both the immediate needs of those infected and the broader implications for sexual health, thereby reducing the likelihood of widespread transmission events.
The Impact of Viral Persistence on Fertility and Reproductive Health
Persistent viruses in semen can have significant implications for fertility and reproductive health. For instance, the presence of Zika virus or Ebola virus in male reproductive fluids may not only pose risks for sexual partners but also impact embryonic development and fertility outcomes in couples attempting to conceive. This sparks urgent discussions in medical communities about the need for screening and preventive strategies that mitigate the risk of transmission during conception efforts.
Moreover, addressing the potential impact of viruses in semen on fertility can also lead to better reproductive health policies. Fertility clinics and healthcare providers need to stay informed about the latest research findings on viral persistence and transmission routes, guiding them in advising patients on safe practices during family planning and conception.
Future Research Directions: Exploring Semen as a Viral Reservoir
The discovery of various viruses present in human semen following acute infections opens up new avenues for research into how viruses act as reservoirs within the male reproductive system. Understanding the mechanisms behind viral persistence can help to trace infection routes and develop targeted interventions. Future research should focus on identifying specific characteristics of viruses that contribute to their longevity in semen, as this knowledge will be essential for addressing emerging viral threats.
Additionally, exploring potential antiviral treatments and vaccine strategies aimed at preventing the sexual transmission of these pathogens will be vital. By building a robust body of research around the implications of viral persistence in semen, scientists and health professionals can work together to enhance public safety and reduce the incidence of sexually transmitted viral infections.
Ebola Virus and Its Long Persistency in Semen
The Ebola virus stands out in discussions about viral persistence due to its remarkably long detectability in human semen. Studies have shown that remnants of the Ebola virus can linger for nearly three years post-infection, raising red flags for public health authorities regarding the risks of sexual transmission. This revelation has necessitated the need for rigorous follow-up protocols for Ebola survivors, especially concerning their reproductive health and the potential risk they pose to sexual partners.
Public awareness campaigns can play a crucial role in educating Ebola survivors about the risks associated with prolonged viral presence in semen. Implementing guidelines for safe sexual practices, including the use of condoms, is essential for preventing further transmission of the virus and ensuring the health of intimate partners. The implications of these findings stretch beyond the individual, as community outreach programs can help mitigate the overall spread of Ebola and improve public health outcomes.
The Zika Virus: A New Frontier in Viral Persistence Studies
The Zika virus has gained significant attention due to its association with birth defects and prolonged viral persistence in semen. This virus has demonstrated an ability to survive in the male reproductive tract for extended durations, leading to concerns about its potential for sexual transmission long after the acute phase of the disease has resolved. Understanding the pathways of viral persistence in the case of Zika can enhance public health strategies aimed at reducing the impact of the virus on reproductive health.
With proactive measures and greater awareness surrounding Zika virus transmission, reproductive health professionals can better advise at-risk populations on preventive strategies. They can inform individuals of the potential risks associated with sexual transmission of the virus, engendering safer practices and ultimately protecting both maternal and fetal health. Future investigations into the nuances of Zika virus persistence in semen will yield crucial insights necessary for developing effective public health interventions.
Emerging Pathogens: Oropouche Virus and Sexual Transmission Potential
Recent findings concerning the Oropouche virus add another layer of complexity to our understanding of viral persistence and transmission. The detection of Oropouche virus genomes in semen raises questions about the potential for sexual transmission, a subject that remains poorly explored. The implications for maternal-fetal health are particularly concerning, given reports linking the virus to severe outcomes, including fetal death in cases of vertical transmission.
As research into emerging pathogens like the Oropouche virus progresses, it is critical to establish frameworks for monitoring transmission routes and communication with healthcare providers. This can ensure that preventative measures are implemented to shield vulnerable populations from the risks associated with these emerging viral threats.
Frequently Asked Questions
What viruses are commonly found in human semen related to sexual transmission?
A systematic review identified 22 viruses detected in human semen post-infection, of which only 9 had noted evidence of sexual transmission. These include known pandemic potential viruses such as the Zika virus and Ebola virus, highlighting significant concerns regarding viral persistence in semen.
How does viral persistence in semen impact sexual transmission?
Viral persistence in semen can extend the window for sexual transmission of infections. For instance, the Ebola virus demonstrated persistence for up to 988 days in semen, while the Zika virus was detectable for 941 days. This raises critical implications for sexual health and infection control.
What are the implications of finding Ebola virus in human semen?
The presence of the Ebola virus in human semen, which can persist for years, raises concerns about potential sexual transmission long after recovery. This persistence underscores the need for continued surveillance and preventive measures to limit transmission risks.
Can the Zika virus infect through semen?
Yes, the Zika virus can be transmitted sexually, and recent studies reveal that it can persist in human semen for an extended period, with maximum detection at 941 days after infection. This highlights the importance of safe sexual practices post-Zika virus infection.
How long do viruses last in human semen after infection?
The duration of viral persistence in semen varies significantly. For example, the Ebola virus can remain detectable for up to 988 days, while other viruses like yellow fever and dengue are shorter, persisting only 21 and 37 days respectively. Individual variability is considerable, emphasizing the need for personalized assessment.
Are there viruses other than Zika and Ebola that persist in human semen?
Yes, a variety of viruses can persist in human semen, including yellow fever virus, West Nile virus, and dengue virus, among others. Each virus has a different persistence timeline, which can influence potential sexual transmission risks.
What are the potential consequences of viral transmission through human semen?
Viral transmission through human semen can lead to persistent infections, affecting not only the health of sexual partners but also posing risks for fetal development in pregnancy. The implications extend to public health strategies aimed at controlling outbreaks.
Is sexual transmission of the Oropouche virus confirmed?
Sexual transmission of the Oropouche virus has not been definitively established, but recent findings of its genome in semen and other fluids suggest potential for transmission. Continued research is necessary to fully understand its implications.
How do researchers study the persistence of viruses in human semen?
Researchers analyze semen samples from infected individuals over time to detect the presence of viral genomes. Recent reviews have evaluated the duration of persistence and transmission implications based on data collected from multiple studies.
What other viruses besides Zika and Ebola are recognized for their sexual transmission potential?
Alongside Zika and Ebola, viruses such as Hepatitis A, vaccinia virus, and Crimean-Congo hemorrhagic fever virus have been associated with sexual transmission, though their presence in semen varies and requires further investigation.
| Key Point | Details |
|---|---|
| Viruses Detected | 22 viruses found in human semen after acute infections with implications for disease transmission. |
| Sexual Transmission | Out of the 22 viruses, only 9 showed evidence of sexual transmission. |
| Persistence Duration | Varied by virus: Ebola had the longest persistence (988 days); shortest was Kyasanur Forest disease (8 days). |
| Other Viruses | 3 additional viruses found in the male reproductive tract but not in semen (Crimean-Congo, hantavirus, Heartland virus). |
| Recent Findings | Oropouche virus found in semen and other fluids; potential for vertical transmission. |
| Study Reference | Study published in The Lancet Microbe highlights impacts on drug and vaccine development. |
Summary
Viruses in human semen pose significant concerns for health and disease transmission. The recent systematic review identified 22 different viruses present in human semen post-infection, some with potential pandemic implications. This highlights the importance of understanding how these viruses persist and the risk of sexual transmission, which can contribute to outbreaks and affect reproductive health. The insights from this study underscore the need for ongoing research in this area to help in the development of effective novel treatments and preventive measures.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.