Vaccine hesitancy research has become a crucial focus in public health, especially as recent trends show alarming declines in vaccine uptake. The National Institutes of Health (NIH) has abruptly cut funding for over 33 significant research grants that aimed to address this issue, sparking concern among scientists and policymakers alike. With the ongoing surge in diseases like measles—currently affecting communities across the USA—understanding the factors contributing to vaccine skepticism is more vital than ever. These cuts coincide with a broader debate surrounding vaccine strategies and the recently appointed Department of Health and Human Services (HHS) secretary, Robert F. Kennedy Jr., whose known skepticism on vaccines raises important questions about future health policies. As mRNA vaccine studies remain pivotal in controlling outbreaks, the shift in funding priorities by NIH adds another layer of complexity to improving health outcomes and increasing public trust in vaccines.
Research on vaccine resistance and public perception surrounding immunization is more important now than ever, particularly against the backdrop of rising health crises. The recent decision by the NIH to withdraw support from numerous pivotal studies not only jeopardizes insights into why many individuals are reluctant to vaccinate but also hinders efforts to devise effective vaccine uptake strategies. As the U.S. grapples with a significant resurgence of preventable diseases, the challenge is to bridge the gap in understanding vaccine attitude and commitment. Under the leadership of HHS secretary Robert F. Kennedy Jr., whose skepticism regarding vaccines has been documented, the direction of health policy may take a turn that affects public health strategies. The urgency to enhance vaccine confidence is compounded by recent legislative actions and ongoing mRNA vaccine studies, stressing the need for a thorough analysis of community responses to vaccinations.
The Impact of NIH Research Cuts on Vaccine Hesitancy Studies
The recent decision by the National Institutes of Health (NIH) to terminate over 33 research grants on vaccination hesitancy significantly hampers our understanding of why some individuals resist vaccines. As the global health community continues to battle misinformation, particularly around mRNA vaccine studies, such cuts leave a gap in vital research that could uncover the psychological and societal factors influencing vaccine uptake. Understanding these factors is crucial, especially in the context of a rising measles outbreak that underscores the public health implications of vaccine hesitancy.
NIH’s focus on discontinuing vaccine hesitancy research reflects a troubling trend in prioritizing immediate scientific interests over the complex narratives surrounding vaccine discussions. The terminated grants were designed to explore various strategies to increase vaccine uptake, particularly within marginalized communities. Without this research, public health strategies may lack the nuanced understanding necessary to effectively combat misinformation and promote vaccine acceptance, leaving important populations vulnerable.
Connecting Vaccine Hesitancy to Current Health Challenges
The recent measles outbreak affecting the Texas-New Mexico border highlights the urgent need to address vaccine hesitancy as a public health threat. With over 253 individuals infected, many of whom were unvaccinated, the situation poses a reminder of the consequences of declining vaccination rates. The NIH’s decision to cut funding for research intended to explore vaccine hesitancy undermines essential efforts to comprehend and address these health crises, potentially leading to further outbreaks of vaccine-preventable diseases.
In light of this measles outbreak, it’s evident that the cuts to vaccine hesitancy research are misaligned with public health needs. Insights gleaned from studies that focus on behavioral and demographic factors influencing vaccination decisions could prove invaluable in designing targeted interventions. By redirecting resources away from understanding vaccine hesitancy, we may be compromising the ability to develop effective strategies that ensure the safety and health of the population.
The Role of Health Policy in Vaccine Uptake Strategies
The appointment of HHS Secretary Robert F. Kennedy Jr., known for his skepticism regarding vaccines, raises concerns about the direction of health policy relating to vaccine uptake. His influence could steer federal efforts towards narratives that undermine established scientific consensus on vaccinations, thus exacerbating vaccine hesitancy. This reversal in health policy could have profound impacts on vaccine uptake strategies across the United States, particularly during critical periods when public trust is needed most.
As health policy continues to evolve, it’s imperative to ensure that vaccine uptake strategies are rooted in solid scientific research rather than populist rhetoric. Cutting essential studies on vaccine hesitancy and adopting a more skeptical stance on the benefits of vaccines could hinder progress towards health goals, especially in light of increasing opposition and misinformation around vaccines. Addressing vaccine hesitancy effectively requires robust financial support for research to create data-driven public trust initiatives.
Understanding mRNA Vaccine Studies Amidst Emerging Hesitancy
The NIH’s recent shift away from funding mRNA vaccine studies, particularly those that include vaccine hesitancy as a variable, presents a significant challenge in understanding public sentiment towards novel vaccine technologies. As mRNA vaccines have become pivotal in combating infectious diseases like COVID-19, examining the factors influencing their acceptance is more crucial than ever. Research in this area could identify barriers to adoption and inform strategies aimed at increasing public confidence in these innovative medical interventions.
Without adequate research resources dedicated to exploring the complexities surrounding vaccine hesitancy, particularly related to mRNA technologies, we risk a fraction of the population remaining resistant to vaccination. Such resistance poses severe threats not only to individual health but also to community immunity. Expanding our understanding of these dynamics is essential, especially as advancements in vaccine technology continue to reshape the landscape of public health.
Public Health Implications of Vaccine Hesitancy Research Cuts
The termination of critical research grants aimed at understanding vaccine hesitancy at the NIH is alarming, especially in the context of public health threats like the ongoing measles outbreak. These cuts may yield long-term consequences for vaccination programs and public health initiatives, as less understanding of vaccine reluctance translates to ineffective health communication strategies. Health professionals rely on evidence-based research to create campaigns that resonate with communities, making this funding withdrawal particularly detrimental.
Effective public health strategies designed to combat vaccine hesitancy must be informed by rigorous research that examines the motivations behind reluctance. Without funding focused on these areas, public health messaging may fall short of persuading hesitant individuals, thereby compromising efforts to improve vaccine uptake in critical populations. The intersection of public health advocacy and research voices must be reinforced to counteract the challenges posed by vaccine skepticism.
Innovations in Vaccine Uptake Strategies During a Measles Outbreak
As the current measles outbreak makes headlines, it is crucial to strategize innovative approaches to improve vaccine uptake. Vaccination campaigns that utilize technology and data analysis to identify target populations can optimize outreach efforts while addressing apprehensions that contribute to vaccine hesitancy. Employing community leaders and trusted figures in these initiatives can also enhance the perceived reliability of such programs, leveraging social influence to promote vaccination.
Moreover, understanding demographic patterns surrounding vaccine hesitancy will inform targeted interventions more effectively. Public health organizations must integrate comprehensive data that captures specific community worries and educate individuals using tailored messaging strategies. Such proactive approaches not only counter existing myths surrounding vaccines but also foster an environment where the importance of vaccination becomes inherently understood in the context of community health.
Future Direction of NIH Funding for Vaccine Research
The future of NIH funding for vaccine research, particularly in understanding vaccine hesitancy, requires a reassessment of priorities as public health challenges continue to emerge. With the potential for new variants and outbreaks, the need for comprehensive vaccine research remains critical. Advocacy for funding must emphasize the implications of vaccine hesitancy on community immunity and stress the importance of maintaining a keen focus on research that reveals the underlying reasons for vaccine reluctance.
Transitioning funding back towards exploration in vaccine hesitancy could redefine public health initiatives, ensuring that new strategies align closely with population needs. Investing in this area is paramount to fostering a culture of vaccination acceptance and resilience against misinformation, particularly as new studies and data emerge in light of the COVID-19 pandemic. The NIH must recognize that addressing vaccine hesitancy now secures public health for generations to come.
Recognizing Vaccine Acceptance and Its Societal Impact
Vaccine acceptance hinges on myriad societal factors ranging from cultural beliefs to misinformation campaigns. By breaking down these barriers through concerted research efforts, public health organizations can better prepare strategies that resonate with diverse communities. Understanding the societal impact of vaccination is crucial in combating the spread of diseases, particularly as we face rising numbers of uncontrolled outbreaks like measles. Through informed research, communities can be educated, empowered, and protected against such preventable diseases.
Fostering environments that embrace vaccination necessitates addressing both concerns and misinformation simultaneously. Public perception of vaccines emerges through a complicated web of societal interaction, where targeted educational efforts can lead to increased acceptance. Public health advocates must work tirelessly to build trust and convey accurate information, especially in areas affected by cultural mistrust or skepticism towards the medical establishment. Through sustained dialogue and education, vaccine acceptance can significantly improve community health outcomes.
Leveraging Community Engagement in Vaccine Programs
Engagement with local communities plays an integral role in enhancing vaccine uptake, particularly when addressing vaccine hesitancy. By working closely with community leaders, health organizations can transform defensive attitudes towards vaccinations into supportive consensus, fostering a collaborative approach to healthcare. Community-centered programs can help individuals feel informed and connected, driving down the rates of vaccine hesitancy while boosting uptake.
Grassroots mobilization can prove especially effective in reaching isolated or distrustful populations. Educational initiatives that focus on dialogue and understanding community-specific worries can help healthcare providers address concerns empathetically. By creating a respectful and open framework for discussion, public health efforts can change perceptions about vaccines significantly, encouraging a culture of health that benefits everyone.
Frequently Asked Questions
What is vaccine hesitancy research and why is it important?
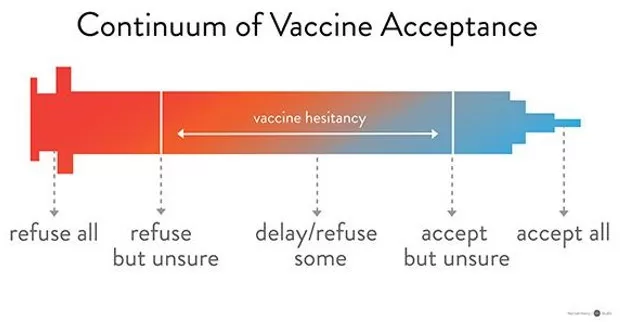
Vaccine hesitancy research investigates the factors that lead individuals to delay or refuse vaccinations, impacting public health efforts to increase vaccine uptake. Understanding these factors is crucial, especially during health crises like the current measles outbreak in the USA, as it enables the development of tailored strategies to improve vaccine acceptance and commitment.
How have NIH research cuts affected vaccine hesitancy research?
Recent NIH research cuts have resulted in the termination of at least 33 grants focused on vaccine hesitancy and vaccine uptake strategies. These cuts could hinder progress in understanding the reasons behind vaccine skepticism and limit the development of effective interventions to boost vaccination rates.
What impact does the new HHS secretary, Robert F. Kennedy Jr., have on vaccine hesitancy research?
HHS Secretary Robert F. Kennedy Jr., known for his skepticism towards vaccines, may influence policy changes that affect vaccine hesitancy research funding and priorities. His stance could lead to reduced focus on critical research aimed at promoting vaccine uptake during significant health outbreaks.
Why is understanding vaccine hesitancy critical in the context of recent mRNA vaccine studies?
Understanding vaccine hesitancy is essential in the context of mRNA vaccine studies as it helps identify barriers to acceptance and informs strategies to enhance public confidence in newly developed vaccines. Given the current landscape of vaccine misinformation, effective communication is key to improving vaccine uptake.
How does vaccine hesitancy relate to the ongoing measles outbreak in the USA?
The ongoing measles outbreak, which has primarily affected unvaccinated individuals, highlights the urgency of addressing vaccine hesitancy. Research in this area can uncover the motivations behind refusal to vaccinate and help health authorities create effective outreach programs to increase vaccine interest among affected communities.
What strategies are being explored to counter vaccine hesitancy?
Strategies to counter vaccine hesitancy include community engagement initiatives, educational campaigns addressing common myths, and policies designed to make vaccine access easier. Research on these approaches is vital to bolster vaccine uptake, especially in communities disproportionately affected by misinformation.
What role does research play in addressing vaccine hesitancy among minority groups?
Research plays a crucial role in understanding and addressing vaccine hesitancy among minority groups by providing insights into cultural, social, and economic factors that influence health behaviors. Tailored health interventions informed by this research are essential for improving vaccination rates within these communities.
| Key Point | Details |
|---|---|
| NIH Termination of Grants | NIH has terminated at least 33 research grants focused on vaccine hesitancy. |
| Scope of Affected Research | Nine additional grants were significantly scaled back, impacting studies on various vaccines and addressing vaccine uptake. |
| Reason for Grant Termination | NIH stated the research no longer aligns with agency priorities, specifically avoiding studies on why individuals refuse vaccines. |
| Current Public Health Concerns | The decision comes during a significant measles outbreak affecting primarily unvaccinated individuals. |
| Influence of HHS Secretary | HHS Secretary Robert F. Kennedy Jr. is known for his vaccine skepticism, influencing NIH’s funding priorities. |
| Impact on Research Diversity | Some terminated grants specifically targeted vaccine uptake in racial minority groups, indicating potential gaps in future research. |
Summary
The recent cuts in NIH funding highlight a troubling trend in vaccine hesitancy research. Specifically, the termination of 33 research grants dedicated to understanding vaccine hesitancy significantly undermines efforts to address public concerns and increase vaccination rates. As vaccine hesitancy continues to pose a substantial public health challenge, these funding reductions could limit crucial insights necessary for developing effective interventions. The involvement of politically motivated figures, such as HHS Secretary Robert F. Kennedy Jr., further complicates the landscape of vaccine policy and research priorities. Overall, this shift in focus away from vaccine hesitancy research raises alarm bells as the nation confronts public health crises like measles outbreaks.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.