Pandemic preparedness research is gaining heightened attention as global leaders emphasize the urgent need to bolster collective efforts in combating potential health crises. In a recent call by the Coalition for Epidemic Preparedness Innovations (CEPI) and the World Health Organization (WHO), experts pointed to the importance of understanding families of pathogens instead of focusing solely on individual infectious agents. This comprehensive approach is crucial for developing effective pandemic research strategies that ensure optimal epidemic readiness. By prioritizing pathogens based on their epidemic potential, researchers aim to enhance global health research and ultimately create a robust framework for anticipating and managing future pandemics. As new pathogens emerge and the landscape of infectious diseases evolves, continuous investigation and development will remain essential to safeguard public health.
Research into pandemic readiness encompasses a broad spectrum of studies aimed at mitigating the impacts of future infectious disease outbreaks. This vital inquiry extends to the prioritization of diverse pathogen families, adopting innovative practices in global health exploration which can help predict and respond to emerging threats. By addressing known and unknown pathogens through systematic investigative approaches, experts can better understand the dynamics of epidemic situations. Encompassing a wide array of global health research initiatives, epidemic readiness becomes a collective challenge that requires international collaboration and resource sharing to ensure that communities worldwide are prepared for potential health emergencies. The scientific community’s dedication to this cause signals a unified commitment to public health resilience in light of inevitable future pandemics.
The Importance of Pandemic Preparedness Research
Pandemic preparedness research is critical for mitigating the effects of future global health crises. As highlighted by the Coalition for Epidemic Preparedness Innovations (CEPI) and the World Health Organization (WHO), enhancing readiness requires a strategic focus on families of pathogens rather than solely relying on individual infectious microbes. By developing a comprehensive understanding of entire pathogen families, we can create robust frameworks for epidemic readiness that prioritize research on both high-risk and low-profile pathogens. This proactive approach is essential to identify potential threats before they escalate into widespread outbreaks.
Moreover, the emphasis on pandemic preparedness research shapes not only the scientific understanding of pathogens but also informs public health policies globally. By aligning global health research efforts with the direct findings of pathogen prioritization, countries can ensure that resources are allocated efficiently to address the most pressing epidemiological concerns. This collaborative effort calls for the integration of knowledge from diverse regions, recognizing that the landscape of pandemic threats is continuously evolving.
Pathogen Prioritization: A Key Strategy for Global Health
Pathogen prioritization is a cornerstone of effective pandemic research strategies aimed at identifying and mitigating potential public health threats. The recent WHO report illustrates a rigorous process where over 200 scientists evaluated the infectious potential of 1,652 pathogens, aiding in the classification of pathogen families based on their pandemic potential. This prioritization underlines the necessity to focus scientific and governmental resources on the most concerning pathogens, thereby improving our collective response to emerging infectious diseases.
Additionally, pathogen prioritization fosters the establishment of Family Expert Groups (FEGs) that can streamline research initiatives and drive consensus on the allocation of funding, surveillance strategies, and vaccine development. By engaging a global network of experts and employing data-driven methodologies, we not only enhance our preparedness for known threats but also build a scalable framework that can adapt to unexpected pathogen emergence.
Enhancing Epidemic Readiness Through Research Collaboration
The urgency of enhancing epidemic readiness cannot be understated, especially as global health experts call for cooperative research across multiple nations. This collaboration not only ensures that information is shared swiftly in times of crisis but also engages local scientists who understand their regions’ unique pathogen profiles. Through initiatives like the Collaborative Open Research Consortium, the WHO aims to connect research institutions and leverage collective intelligence to improve pathogen surveillance and infectious disease research across diverse demographics.
Furthermore, establishing a cooperative research framework enables the development of adaptable tools and methodologies that can be deployed rapidly during emerging health threats. These tools will assist countries in maintaining vigilance and preparedness, along with addressing gaps in knowledge related to pathogen transmission and human immunity responses. By laying out a global plan of action that emphasizes shared responsibility and transparency, we can collectively enhance our epidemic readiness.
Developing Prototype Pathogens for Future Preparedness
The concept of utilizing prototype pathogens is pivotal in advancing infection control and prevention measures. Prototype pathogens serve as models that encapsulate the characteristics of entire families of pathogens, allowing researchers to study transmission dynamics, host interactions, and treatment responses more effectively. This focus on prototype pathogens not only accelerates vaccine development but also enhances understanding of disease mechanisms, which is crucial for responding to future epidemic threats.
In addition to immediate research applications, developing prototype pathogens lays a foundation for ongoing scientific inquiry into previously under-researched areas of infectious diseases. By encouraging studies surrounding these representative pathogens, the scientific community can better prepare for the unforeseen nature of the next pandemic. Ongoing evaluations and advancements in research under this strategy will ensure humanity remains resilient against infectious disease outbreaks.
Global Health Research: The Path to Pandemic Resilience
Global health research plays a critical role in building resilience against pandemics through comprehensive data collection and analytical methodologies. The approach toward broad-based research seeks to integrate knowledge from various domains such as epidemiology, virology, and public health policy to form an adaptive response framework. By enhancing collaboration among researchers worldwide, the goal is to generate robust insights that can inform governmental actions and public health responses.
Moreover, this expansive research network fosters innovation in surveillance technologies and theoretical modeling, thereby improving prediction accuracy for potential epidemics. Engaging in global health research not only addresses the immediate concerns of infectious disease control but also lays the groundwork for long-term preparedness strategies in an increasingly interconnected world. Continuous collaboration and sharing of results across nations strengthen the global response to new and ongoing health threats.
The Role of Data in Pathogens and Global Health Strategies
Data collection and analysis are fundamental to developing effective global health strategies, especially in understanding the behavior of pathogens that could trigger pandemics. Comprehensive datasets that include the geographical distribution, historical outbreaks, and genetic analysis of pathogens allow researchers to identify trends and patterns that may indicate potential risks. In the context of the recent WHO pathogen prioritization framework, these data-driven insights directly support the identification of high-risk pathogens that warrant immediate research attention.
The integration of sophisticated data analytics also aids in continuously updating risk assessments and response strategies. By systematically evaluating the evolving landscape of infectious diseases, public health officials can make informed decisions regarding vaccine distribution, treatment protocols, and effective surveillance measures. Leveraging data as a prime resource enhances not just the readiness but also the overall capacity to respond to pathogen-induced health emergencies, ensuring a spectrum of proactive health safeguards.
Innovations in Pathogen Surveillance and Response
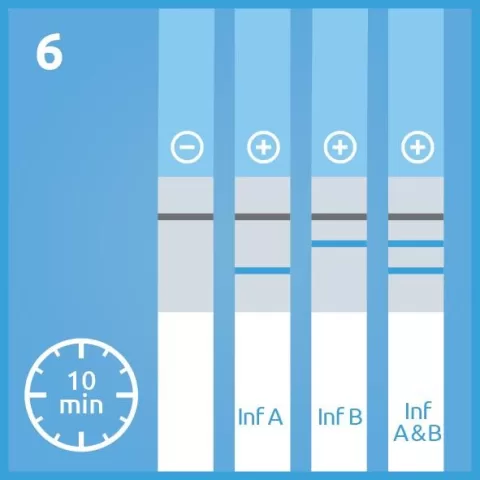
Innovative technologies are transforming pathogen surveillance and response mechanisms, drastically improving our ability to detect and respond to infectious diseases. Advances in genomic sequencing and bioinformatics enable rapid identification of pathogens, facilitating immediate public health response efforts. Such innovations ensure that health authorities can pivot quickly, implementing containment strategies before outbreaks escalate into pandemics.
Moreover, integrating real-time surveillance systems with international cooperation enhances our global readiness against infectious threats. Countries collectively sharing surveillance data can identify emerging pathogens that might not otherwise be detected. This collaborative approach not only increases situational awareness across borders but also creates a formidable global network capable of tackling epidemic readiness head-on.
Education and Training for Future Global Health Leaders
Investing in education and training for future global health leaders is essential for fostering the next generation of scientists and public health experts who will respond to pandemics. By incorporating comprehensive curricula that focus on epidemiology, infectious disease research, and global health policies, educational institutions can cultivate a workforce equipped to navigate the complexities of future health challenges.
Moreover, practical training opportunities should be emphasized to provide hands-on experiences in research settings. Initiatives that encourage internships and collaborative projects with established research institutions can enhance skill development and promote a culture of innovation. As the need for effective pandemic preparedness grows, nurturing a knowledgeable and adaptive workforce is vital to the ongoing fight against infectious diseases.
The Future of Pandemic Research: A Collaborative Effort
The future of pandemic research hinges on collaborative efforts between scientists, policymakers, and the global community. Building on the insights gained from past pandemics, stakeholders must work together to create frameworks that prioritize research on a wide variety of pathogens and disease vectors. This collective endeavor not only promises to enhance our understanding of infectious diseases but also strengthens global health systems by fostering unity in addressing common threats.
In conclusion, as we look ahead towards improving pandemic preparedness, the importance of collaboration and interdisciplinary research cannot be overstated. The multifaceted nature of pandemics requires a diverse range of expertise, and only through joint efforts can we hope to develop innovative solutions and effective responses to the challenges posed by infectious diseases. The proactive strategies laid forth by organizations like WHO and CEPI mark a turning point in how we combat future pandemics, emphasizing readiness and cooperation as our primary tools.
Frequently Asked Questions
What is the significance of pandemic preparedness research?
Pandemic preparedness research is crucial for enhancing our response to global health threats. It focuses on understanding pathogens and developing strategies to mitigate the impacts of future pandemics. By prioritizing pathogen families and engaging in global health research, scientists aim to enhance epidemic readiness and ensure communities are better protected against emerging infectious diseases.
How does pathogen prioritization improve pandemic research strategies?
Pathogen prioritization is essential in pandemic research strategies as it allows researchers to identify and focus on the most significant pathogens with pandemic potential. By categorizing pathogens into families and assessing them based on their risks, scientists can develop targeted research agendas and countermeasures, improving global health outcomes during infectious disease outbreaks.
What role does global health research play in epidemic readiness?
Global health research plays a pivotal role in epidemic readiness by fostering international collaboration among scientists to study infectious disease dynamics. This collaborative approach enhances our understanding of pathogen transmission and human immune responses, ultimately leading to more effective surveillance and public health strategies to combat future pandemics.
What are prototype pathogens and why are they important in pandemic preparedness?
Prototype pathogens serve as representative model organisms within pathogen families that researchers study to gain insights into broader groups of infectious agents. Understanding these prototype pathogens helps scientists develop vaccines and treatments that can be swiftly adapted, enhancing pandemic preparedness by ensuring that we can react quickly to unexpected outbreaks.
How does the WHO’s framework for pandemic preparedness impact global research efforts?
The WHO’s framework for pandemic preparedness impacts global research efforts by providing structured guidelines for threat assessment, pathogen prioritization, and collaborative research initiatives. This framework promotes a unified approach to understanding infectious disease risks and enhances global cooperation, ensuring that resources are effectively mobilized to tackle future pandemics.
What challenges does pandemic preparedness research face in resource-limited settings?
Pandemic preparedness research in resource-limited settings faces several challenges, including insufficient infrastructure, lack of funding, and limited access to scientific expertise. These regions often harbor high biodiversity and potential novel pathogens, but their under-researched status highlights the need for increased investment and international cooperation to strengthen research capacities.
How can emerging infectious diseases be better monitored through pandemic preparedness research?
Emerging infectious diseases can be better monitored through pandemic preparedness research by establishing comprehensive surveillance systems that assess pathogen prevalence and transmission dynamics. Integrating advanced technologies, such as genomic sequencing and data analytics, can enhance the detection of new pathogens and facilitate timely public health responses to mitigate outbreaks.
Why is loss of biodiversity a concern for pandemic preparedness?
Loss of biodiversity is a significant concern for pandemic preparedness because it can disrupt ecosystems and increase human exposure to zoonotic pathogens. As wildlife habitats diminish, animals come into closer contact with human populations, raising the risk of spillover events that lead to new infectious diseases. Protecting biodiversity is therefore essential for global health security.
What impact do Family Expert Groups (FEGs) have on pandemic research?
Family Expert Groups (FEGs) significantly impact pandemic research by facilitating expert consensus on high-risk pathogen families. By prioritizing specific pathogens within each family based on their pandemic potential, FEGs help streamline research and development efforts, ensuring resources are directed towards the most pressing threats to public health.
How does international collaboration enhance pandemic preparedness?
International collaboration enhances pandemic preparedness by enabling countries to share knowledge, resources, and best practices in infectious disease research. By fostering a collaborative open research consortium, the global community can tackle complex health challenges, leading to more effective strategies for epidemic response and improved overall public health outcomes.
| Key Points |
|---|
| Global leaders emphasize importance of cooperative research in pandemic preparedness. |
| CEPI and WHO called for research on pathogen families and individual microbes. |
| A report details a global prioritization of pathogens involving over 200 scientists. |
| Focus on highest-risk pathogens for pandemic potential to enhance global health safety. |
| Ongoing strategies will allow continuous risk assessment of emerging infectious diseases. |
| WHO aims to establish a Collaborative Open Research Consortium for pathogen families. |
Summary
Pandemic preparedness research is essential in today’s interconnected world. The recent call from CEPI and WHO highlights the urgent need for a collaborative, comprehensive approach to studying pathogens as families instead of focusing solely on specific viruses or bacteria. This strategy aims to improve our understanding of infectious diseases and develop effective countermeasures against future pandemics. By involving global research institutions and prioritizing resources towards higher-risk pathogens, we can better prepare for unforeseen health threats. Continuous assessment and research are key, ensuring that as new pathogens emerge, our understanding and response mechanisms adapt effectively.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.