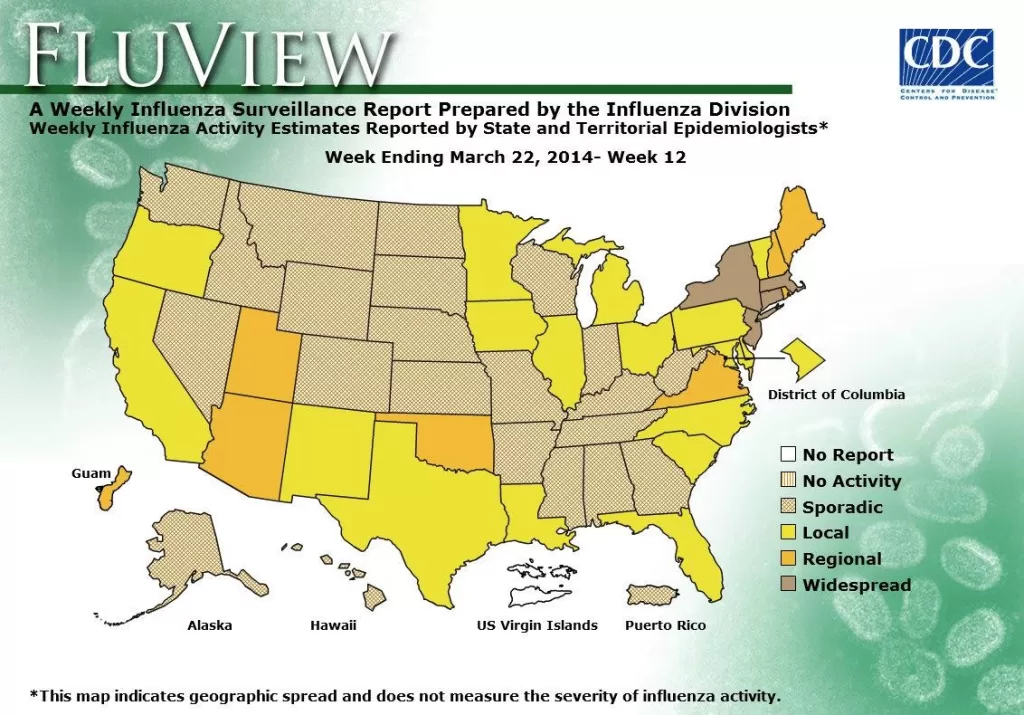
US flu activity has shown a noticeable decline over the past three weeks, yet its lingering effects cast a significant shadow over healthcare providers nationwide. As reported by the CDC in their latest influenza updates, outpatient clinics and hospitals continue to grapple with a heavy influx of flu-related cases, highlighted by an alarming rise in pediatric flu deaths. Amid the ongoing flu season in 2025, test positivity rates remain concerning, maintaining a high level even as they trend downward. With the increasing pressure from flu hospitalizations that have reached their peak since the 2010-11 season, the impact on public health is undeniable. As the CDC flu report reveals, vigilance is still required as we approach the latter part of this challenging flu season.
The current influenza outbreak across the United States has led to heightened concerns about public health, particularly as the flu season unfolds in 2025. The Centers for Disease Control and Prevention (CDC) is closely monitoring the situation, not only focusing on the overall flu activity but also emphasizing the rising pediatric flu fatalities. This year’s flu virus has proved to be quite virulent, causing significant hospitalizations and straining healthcare resources. With health practitioners and authorities working diligently to address the surge in flu-like illnesses, updates on influenza trends and treatment strategies are crucial for informed management. In the context of the ongoing battle against this respiratory illness, understanding the seasonal patterns and resultant health implications remains essential.
Current Trends in US Flu Activity
The latest CDC report indicates that US flu activity has continued its downward trend for the third consecutive week, a promising sign amidst a challenging flu season. Last week, the positivity rate for flu tests hovered around 18.9%, although it remains elevated compared to national averages. With outpatient visits for flu-like symptoms steadily exceeding the baseline for the past 14 weeks, healthcare facilities across the nation still endure significant pressure due to high hospitalization rates. This ongoing trend underlines the need for vigilance as the flu season progresses, particularly as influenza B strains could still emerge.
Despite these promising declines, the healthcare system remains under strain, particularly with rising pediatric flu deaths that now total 114 this season. The recent report of 16 additional pediatric flu fatalities highlights the critical impact that influenza continues to have on vulnerable populations. Healthcare providers are urged to remain proactive in the fight against flu, ensuring that they are equipped with updated data and resources to effectively respond to ongoing challenges associated with high flu hospitalization rates.
Understanding Pediatric Flu Deaths and Hospitalizations
The recent uptick in pediatric flu deaths has raised considerable concern, prompting public health officials to advocate for increased vaccination efforts among young children. The CDC attributes 15 of the reported pediatric deaths to the H1N1 strain of influenza A, emphasizing the importance of vaccination to safeguard this demographic. The vaccines play a crucial role in mitigating severe illness and preventing hospitalization during this flu season, particularly as flu-related hospitalizations reach the highest levels seen since the 2010-11 season.
Flu hospitalizations among children are alarming, with over 29,500 individuals hospitalized recently, indicating a harsh season for pediatric health. The ongoing threat of influenza A, particularly the H1N1 and H3N2 strains, necessitates targeted awareness campaigns and accessibility of vaccines to prevent further tragedies. Health professionals are encouraged to monitor local flu activity trends closely and inform parents about preventive measures to protect their children during this flu season.
Impacts of Flu Season 2025 on Healthcare Facilities and Resources
As the US flu season 2025 unfolds, its effects on healthcare facilities are becoming increasingly evident. Hospitals and outpatient clinics continue to operate under considerable strain, exacerbated by a significantly high rate of flu-related ailments. The cumulative rate of flu hospitalizations last week surpassed levels observed for years, indicating that healthcare systems are taxed to their limits amidst ongoing public health challenges. This situation is reflective of the persistent nature of influenza infections and the effectiveness of public health responses in managing these outcomes.
Moreover, the fact that flu-related hospitalizations are still on an upward trajectory despite a decrease in overall flu activity illustrates the critical need for healthcare facilities to be prepared for peak flu periods. Staffing shortages and resource limitations can be further complicated by simultaneous outbreaks of respiratory illnesses, reflecting a crucial need for ongoing investment in healthcare resources and robust response planning for future flu seasons.
Latest Influenza Updates and Recommendations from the CDC
With the CDC’s latest influenza updates indicating a gradual decline in flu activity, public health officials continue to emphasize the importance of remaining vigilant. Although the flu positivity rate has ceased to climb, flu-related complications and hospitalizations persist. The CDC urges individuals, especially those in high-risk categories, to get vaccinated and stay informed about the ongoing situation through reliable sources. These efforts are vital in reducing the incidence and death associated with flu infections.
In coalescing the information provided in the CDC’s flu report and the current activity landscape, healthcare providers are urged to engage in discussions about vaccine updates and safety protocols during ongoing consultations with patients. Tailored communications regarding the flu vaccines’ efficacy and the necessity for annual vaccinations can bolster public health outcomes, ensuring optimal healthcare practices moving forward.
Strategies for Reducing Flu Hospitalizations
Reducing flu hospitalizations remains a primary target for health departments nationwide, particularly as the flu season 2025 progresses. Public health officials are advocating for enhanced vaccination campaigns, targeting vulnerable populations such as children and the elderly who are at heightened risk of severe outcomes from influenza. Increasing the availability of flu vaccinations at community health centers and clinics plays a vital role in improving overall flu vaccination rates. The aim is to build herd immunity, which is essential to curbing flu transmission.
In addition to vaccination, public health strategies must also include education on effective hygiene practices, such as regular hand washing and respiratory etiquette. By instilling these practices in communities, the potential for widespread transmission can be significantly reduced, thus decreasing the burden on healthcare facilities. Emphasizing the importance of early recognition of flu symptoms can also lead to quicker medical interventions, reducing the likelihood of hospitalization and improving treatment outcomes during this critical healthcare season.
Impact of Influenza Strains on Public Health 2025
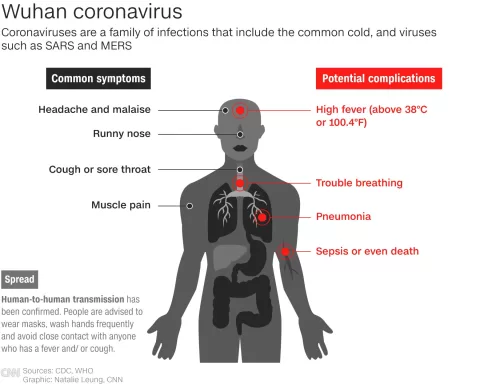
This flu season has seen a prevailing dominance of the H1N1 strain among reported cases, with 54.4% of positive flu tests identified as such. Understanding the implications of different influenza strains on public health is essential. The CDC has reported that while flu activity is declining, strains such as H3N2 and B can still spike late in the season, necessitating ongoing vigilance from healthcare professionals. This understanding of strain dynamics allows targeted communication strategies about vaccine efficacy and public awareness initiatives.
Public health messaging must educate communities on the continued risk presented by various strains of influenza, emphasizing that flu season does not conclude with initial declines in activity. Engaging in robust communication throughout the flu season is vital, ensuring individuals remain aware of the fluctuations and risks associated with emerging influenza strains. This will help mitigate severe impacts and ensure communities are prepared for potential spikes in flu cases.
Role of the CDC in Monitoring Flu Trends
The Centers for Disease Control and Prevention (CDC) plays a crucial role in monitoring flu trends and disseminating vital information to both the public and healthcare professionals. By providing regular updates, such as flu positivity rates and hospitalization statistics, the CDC helps to create a clearer understanding of the ongoing situation. These insights are vital for timely responses to fluctuations in flu activity and aid in planning and resource allocation across healthcare systems.
Additionally, the CDC’s reports encourage local health authorities to conduct their own surveillance and adjust response strategies as needed. The transparency offered by the CDC allows for improved preparedness at the community level, fostering a proactive approach to manage flu season impacts effectively. With accurate data at their fingertips, health officials can educate the public and ensure that necessary precautions are taken to reduce flu transmission rates.
Addressing Vaccine Hesitancy in the 2025 Flu Season
Vaccine hesitancy poses a significant challenge in combating influenza during the 2025 flu season. Many communities exhibit skepticism towards flu vaccinations, often fueled by misinformation and a lack of understanding regarding flu severity. Public health campaigns must address these barriers head-on, providing evidence-based information on the safety and efficacy of the flu vaccine to encourage greater uptake among diverse populations. Special outreach programs targeting historically marginalized communities can also strengthen trust and encourage flu vaccination.
In addition to improving vaccine communication strategies, healthcare providers must foster relationships with patients to discuss their concerns about flu vaccinations openly. Establishing a rapport can facilitate more meaningful conversations about vaccine benefits and health outcomes, leading to increased vaccination rates and improved public health during the flu season. This approach not only seeks to reduce flu-associated deaths but also builds a culture of preparedness for future influenza seasons.
Navigating Co-occurring Respiratory Illnesses
As the flu season 2025 progresses, healthcare professionals face the unique challenge of navigating co-occurring respiratory illnesses alongside influenza outbreaks. With ongoing COVID-19 concerns still influencing public health responses, the dual threats of these viral infections require amplified vigilance from healthcare providers. The CDC’s monitoring and reporting mechanisms are essential in helping delineate trends and symptoms prevalent during this period, informing healthcare responses effectively.
Effective triage protocols within healthcare systems can aid in managing patients presenting with flu-like symptoms, minimizing the risk of overwhelming healthcare facilities. By equipping providers with clear guidelines and public health recommendations, the smart management of dual outbreaks becomes a more achievable goal. Public discourse also plays a vital role in educating communities on distinguishing between different respiratory illnesses and understanding how to seek appropriate medical care during this flu season.
Upcoming Changes in Influenza Vaccination Recommendations
The FDA’s recent announcement regarding upcoming changes in influenza vaccination recommendations for the 2025-26 season underscores the dynamic nature of public health strategies related to flu prevention. These recommendations are critical, as they inform vaccine manufacturers’ approaches to strain selection, ensuring that the upcoming flu vaccines are tailored to combat the most prevalent strains. The timely dissemination of these recommendations allows for a smoother transition into the next flu season, equipping the healthcare community for optimizing vaccination efforts.
Moreover, public health officials must remain proactive in communicating these changes to ensure that healthcare providers and the general public understand the significance of adapting vaccination strategies based on surveillance findings. Enhanced awareness can lead to a more informed public that appreciates the value of updated vaccinations as a tool for preventing influenza, ultimately contributing to lower hospitalization rates and improved health outcomes as we approach subsequent flu seasons.
Frequently Asked Questions
What is the current status of US flu activity in the 2025 flu season?
As of early March 2025, US flu activity has declined for the third consecutive week. The CDC reports a test positivity rate of 18.9%, indicating a downward trend, even though the flu season remains severe. Hospitalizations from flu are on the rise, having reached levels not seen since the 2010-11 season.
How many pediatric flu deaths have occurred during the 2025 flu season in the US?
So far in the 2025 flu season, there have been 114 reported pediatric flu deaths. This number marks a serious concern as it shows a significant impact of flu on children, particularly with recent reports of 16 new pediatric flu deaths.
What does the CDC flu report say about flu hospitalizations?
According to the latest CDC flu report, more than 29,500 individuals were hospitalized for flu last week, showing a cumulative hospitalization rate this season that is the highest since the 2010-11 flu season. The data highlights the ongoing challenges faced by the healthcare system during the current influenza season.
What strains of influenza are currently predominant in the US?
In the US flu season 2025, influenza A predominates, with 96% of positive flu tests being from this strain. Specifically, the subtyped strains include 54.4% of the 2009 H1N1 strain and 45.6% of the H3N2 strain, which are critical for public health monitoring.
What has been the impact of the 2025 flu season compared to previous years?
The 2025 flu season has been marked by high flu activity levels not experienced since the 2017-18 season. With high hospitalization rates and a significant number of pediatric flu deaths, it indicates an unusual severity level for this time of year, raising public health concerns.
How can I stay updated on US flu activity throughout the 2025 flu season?
To stay updated on US flu activity during the 2025 flu season, regularly check the CDC flu report for the latest statistics, vaccination updates, and guidance. The CDC provides vital information about flu trends and health recommendations to help manage and prevent flu outbreaks.
| Key Point | Details |
|---|---|
| Flu Activity Decline | US flu activity has declined for three consecutive weeks, although health impacts remain significant. |
| Pediatric Deaths | 16 new pediatric flu deaths reported last week, bringing the total to 114 for the season. |
| Test Positivity Rates | Flu test positivity was at 18.9%, with outpatient visits for flu-like illness above national baseline for 14 weeks. |
| Hospitalizations | Cumulative hospitalization rate high, with 29,500 hospitalized last week. |
| Influenza A Dominance | 96% of positive flu tests were influenza A, predominantly H1N1 and H3N2. |
Summary
US flu activity has shown a decline over the past few weeks, indicating a positive trend in combating the virus. However, the ongoing effects on healthcare systems remain critical, especially with significant pediatric mortality and high hospitalization rates. As healthcare providers focus on managing flu cases, understanding these dynamics is essential for public health preparation.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.