DoxyPEP, or doxycycline post-exposure prophylaxis, is gaining attention in the realm of sexual health due to its role in combating sexually transmitted infections (STIs). However, recent studies indicate a concerning trend in antimicrobial resistance, particularly with Neisseria gonorrhoeae resistance escalating in tandem with increased tetracycline usage. Findings from sexual health clinics reveal that while doxyPEP effectively reduces STI risks among vulnerable populations, it simultaneously raises concerns regarding resistance patterns and the impact on non-target bacteria. The implementation of doxyPEP guidelines by health officials, influenced by clinical trial data, illustrates its clinical efficacy but also highlights the urgent need to monitor antimicrobial resistance within treated individuals. As use of doxyPEP expands, understanding the implications of tetracycline resistance becomes crucial for safeguarding sexual health and overall public health outcomes.
Doxycycline post-exposure prophylaxis (doxyPEP) has emerged as a prominent strategy in the fight against STIs, particularly among at-risk populations. This approach, however, brings forth significant discussions surrounding antibiotic resistance, especially concerning increasing resistance in Neisseria gonorrhoeae and other related pathogens. Recent investigations conducted in sexual health clinics provide critical insights into the dynamics of tetracycline resistance and its ramifications on both targeted and non-target bacterial populations. As health authorities refine doxyPEP guidelines based on real-world findings, the relationship between this prophylactic measure and the development of antimicrobial resistance is placing a spotlight on the delicate balance between prevention and the emergence of resistant strains. Thus, ongoing surveillance and research will be paramount in understanding and mitigating the potential adverse effects of doxyPEP’s expanded use on public health.
Understanding DoxyPEP and Its Role in Antimicrobial Resistance
Doxycycline post-exposure prophylaxis (doxyPEP) has emerged as a significant method to curb the transmission of sexually transmitted infections (STIs) among at-risk populations, particularly men who have sex with men (MSM) and transgender women. Its implementation, guided by robust clinical trial data, demonstrates a marked decrease in infections. However, this beneficial intervention raises valid concerns regarding antimicrobial resistance (AMR), particularly in relation to Neisseria gonorrhoeae and other bacteria such as Staphylococcus aureus. Tetracycline resistance within these bacterial populations has been surging, demanding a careful evaluation of doxyPEP’s long-term impacts on AMR following its widespread adoption in clinical practice.
Recent studies, including those published by researchers at the University of Washington, highlight the complexities of addressing AMR in the context of doxyPEP usage. Despite initial evidence suggesting that doxyPEP is effective in reducing STI rates, it has also been associated with an increase in tetracycline resistance genes among non-target bacteria. As health departments like Public Health–Seattle and King County implement new doxyPEP guidelines, it is crucial to balance the need for effective STI prevention with the ominous specter of rising antimicrobial resistance. Monitoring the long-term effects of doxyPEP usage will be key in understanding its full implications on public health.
Frequently Asked Questions
What is doxyPEP and how does it relate to antimicrobial resistance?
DoxyPEP, or doxycycline post-exposure prophylaxis, is an intervention designed to reduce the risk of sexually transmitted infections (STIs) among at-risk populations, particularly men who have sex with men (MSM) and transgender women. However, its usage has raised concerns about increasing antimicrobial resistance (AMR), particularly in Neisseria gonorrhoeae, which has shown rising resistance to tetracyclines, including doxycycline. Research indicates that while doxyPEP effectively reduces STI risks, it may also exert pressure on bacterial populations, contributing to heightened resistance rates.
What findings on Neisseria gonorrhoeae resistance were reported from sexual health clinics?
Recent findings from a study at a sexual health clinic indicated a significant increase in resistance to tetracyclines in Neisseria gonorrhoeae isolates. The prevalence of tetracycline resistance genes (tetR) rose dramatically from 27% in early 2023 to 70% by mid-2024. This alarming trend is likely influenced by the increased use of doxyPEP among patients, sparking concerns that doxyPEP may foster antimicrobial resistance in N. gonorrhoeae and reduce its preventive efficacy.
How does tetracycline resistance affect the effectiveness of doxyPEP?
The increasing prevalence of tetracycline resistance in Neisseria gonorrhoeae may significantly undermine the effectiveness of doxyPEP. As more bacterial strains become resistant, the ability of doxyPEP to prevent gonorrheal infections could be compromised. If resistance continues to escalate, public health officials worry that the anticipated benefits of doxycycline prophylaxis could diminish, necessitating ongoing surveillance and potential changes in treatment guidelines.
What do the updated doxyPEP guidelines recommend regarding tetracycline resistance monitoring?
The updated doxyPEP guidelines emphasize the importance of monitoring for tetracycline resistance among bacterial pathogens, particularly N. gonorrhoeae. Health providers are advised to be cautious when prescribing doxycycline for patients using doxyPEP, especially for skin or lower respiratory infections, due to the potential for increased resistance development. Continuous evaluation of doxyPEP’s effects on AMR and the microbiome is recommended to guide future public health strategies.
What role does surveillance play in managing doxyPEP and antibiotic resistance?
Surveillance plays a crucial role in assessing the impact of doxyPEP implementation on bacterial colonization and antimicrobial resistance. By closely monitoring resistance patterns, particularly in Neisseria gonorrhoeae and non-target bacteria like Staphylococcus aureus, public health authorities can make informed decisions about treatment protocols and guidelines. Enhanced surveillance can help identify emerging resistance trends and inform necessary adjustments to doxyPEP usage, ensuring that it remains an effective tool in STI prevention.
Are there any risks associated with doxyPEP as identified by researchers?
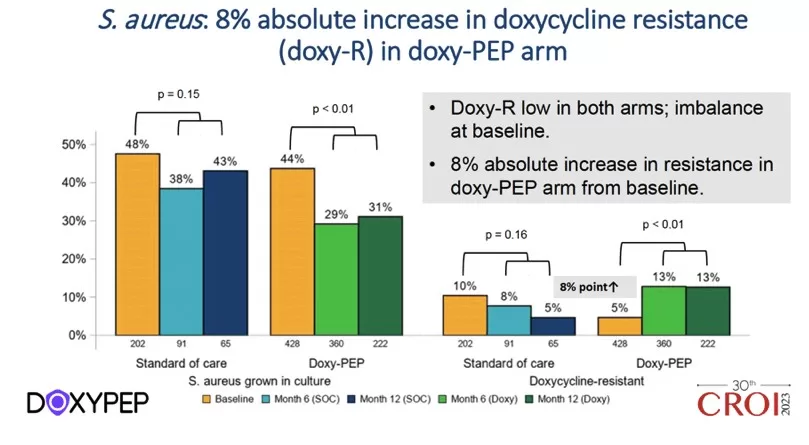
Yes, researchers have identified risks associated with doxyPEP, particularly concerning its potential to increase antimicrobial resistance among both targeted STIs and non-target bacteria. For instance, increased tetracycline resistance rates in Staphylococcus aureus were noted among doxyPEP users. Despite its benefits in reducing STIs, the long-term consequences of repeated doxycycline use on microbial ecology and resistance patterns need careful consideration and further research to mitigate risks effectively.
How did doxyPEP affect non-target bacteria in patients?
DoxyPEP may have implications for non-target bacteria, with evidence indicating an increase in tetracycline-resistant Staphylococcus aureus among users compared to non-users. While overall colonization rates of S. aureus were lower in doxyPEP users, the prevalence of antibiotic-resistant strains was higher. This suggests that even with beneficial effects on STIs, doxyPEP could result in unintended consequences for the microbiome, raising concerns about monitoring and managing AMR in non-target bacteria.
| Key Point | Details |
|---|---|
| Study Origin | University of Washington’s research on Neisseria gonorrhoeae. |
| Findings on Resistance | Increased resistance to tetracyclines noted in N. gonorrhoeae. |
| DoxyPEP Introduction | PHSKC issued doxyPEP guidance based on DoxyPEP Study trial data. |
| Efficacy | Reduced risk of STIs in MSM and transgender women. |
| Resistance Monitoring | Concerns over doxyPEP impact on antimicrobial resistance in non-target bacteria. |
| Data Analysis | Gonorrhea data showed increase in tetracycline resistance over time. |
| Overall Impact of doxyPEP | Increase in antimicrobial pressure possibly affecting efficacy of doxyPEP. |
| Future Recommendations | Call for enhanced surveillance and monitoring of AMR and microbiome changes. |
Summary
DoxyPEP and antimicrobial resistance are critical concerns emerging from recent studies revealing increased tetracycline resistance in Neisseria gonorrhoeae. The implementation of doxycycline post-exposure prophylaxis (doxyPEP) has shown significant efficacy in preventing STIs but raises important questions regarding its effects on antimicrobial resistance. With reported increases in resistance rates and changes in the gut microbiome, public health officials emphasize the need for vigilant monitoring of both targeted and non-target bacterial populations as doxyPEP usage expands. Continued research is essential to ensure that the benefits of doxyPEP do not come at the cost of increasing antimicrobial resistance.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.